1 Department of Neurosurgery, Affiliated Hospital of Southwest Medical University, 646000 Luzhou, Sichuan, China
2 Department of Gerontology, Affiliated Hospital of Southwest Medical University, 646000 Luzhou, Sichuan, China
3 Department of Neurosurgery, West China Hospital, Sichuan University, 610000 Chengdu, Sichuan, China
Abstract
Recent studies suggest that the anterior limb of the internal capsule may be an area of convergence for multiple compulsion loops. In this study, the role of different dopaminergic compulsion loops in the mechanism of obsessive-compulsive disorder (OCD) was investigated by selectively damaging dopaminergic neurons or fibers in the corresponding targets with 6-hydroxydopamine (6-OHDA) and depicting the anatomical map of various compulsion loops located in the anterior limb of the internal capsule.
A total of 52 male Sprague Dawley (SD) rats were exposed to either saline (1 mL/kg, NS group, n = 6) or quinpirole (QNP, dopamine D2-agonist, 0.5 mg/kg, n = 46) twice weekly for 5 weeks. After each injection, the rats were placed on an open field to analyze aspects of their behaviour, including the number of home base visits (NOH), average time between each home base visit (ATBO), and total distance travelled (TDM). After model setup, 46 QNP rats were divided randomly into five groups: 6-OHDA anterior limb of internal capsule (AC) stereotactic injection group (QNP+AC group, n = 10), 6-OHDA mediodorsal thalamic nucleus (MD) stereotactic injection group (QNP+MD group, n = 10), 6-OHDA nucleus accumbens (NAC) stereotactic injection group (QNP+NAC group, n = 10), saline stereotactic injection group (QNP+NS-S group, n = 10), and non-surgical group (QNP+Non-S group, n = 6). In the NS group, rats simultaneously received a 6-OHDA stereotactic injection (NS+6-OHDA-S group, n = 6: AC2, MD2, NAC2). All QNP-treated rats were then continued to be given QNP twice a week for 4 weeks, and their behaviour was observed after each infusion. After 4 weeks, immunofluorescence staining was used to monitor the distribution of dopamine neurons and nerve fibers in different areas of the intervention nerve loops, and quantitative analysis was performed.
Compulsive behaviour declined gradually in the QNP+AC and QNP+NAC groups 3 and 4 weeks after surgery, with the QNP+AC group decreasing more rapidly. The QNP+MD group had decreased by 3 weeks after surgery but increased to almost the same level as pre-surgery at 4 weeks post-surgery. Postoperative fluorescence staining and quantitative analysis suggested the number of dopamine (DA) neurons or nerve fibers in the corresponding target area of the 6-OHDA injection were significantly reduced compared with the QNP+Non-S group.
6-OHDA selectively damages the targets of dopaminergic neurons or nerve fibers within the OCD loop, which somewhat alleviates compulsive behaviours. The results suggest that the AC might be the best target for therapeutic interventions for OCD.
Keywords
- obsessive-compulsive disorder
- 6-hydroxydopamine
- anterior limb of internal capsule
- nucleus accumbens
- mediodorsal thalamic nucleus
Obsessive-compulsive disorder (OCD) in humans is proposed to be multidimensional with different neurobiological underpinnings, often associated with neuropsychiatric and neuropsychological disorders [1, 2]. For almost 40 years, numerous investigators have tried to identify an ideal OCD animal model [3, 4, 5]. Some studies have suggested that the dopamine neurotransmitter system is closely related to OCD [6, 7]. The dopamine receptor (DR) belongs to the G protein-coupled receptor (GPCR) family and includes five receptor subtypes: D1R, D2R, D3R, D4R, and D5R [8]. The D2R and D3R isomers are highly homologous and bind to nearly the same site as the dopaminergic ligand [9, 10]. The D2R and D3R subtypes are mainly associated with schizophrenia, drug addiction, depression, Tourette’s syndrome, and sexual compulsion [11].
Quinpirole (QNP, a dopaminergic D2R and D3R agonist) was first used to establish OCD models when Szechtman et al. [12] accidentally discovered that quinpirole-sensitized animals showed constant repeated examination and reward-related behavioural changes during an experiment that examined animal models of schizophrenia. To systematically evaluate compulsive-like behaviours generated by QNP, suitable behavioural evaluation tools and corresponding behavioural evaluation criteria were developed [13]. It was shown that most rats began to show compulsive-like behaviours such as repeated home return 15 min after subcutaneous injection of quinpirole, with the effect most evident around 30 min and lasting for 55 min. This stable expression of repetitive homecoming behaviour has increasingly been used in animal models of compulsive behaviour [13].
The QNP-induced animal model has been shown sufficient in all three aspects, including apparent validity [14, 15], predictive validity [16], and structural validity [17], and has been widely used in numerous studies. 6-Hydroxydopamine (6-OHDA), a hydroxylated dopamine analogue, has been well-established as a neurotoxin through intracranial injection. 6-OHDA is widely used to create a rodent model of Parkinson’s disease (PD) through the substantia nigra striatum pathway in animals [6, 18]. Due to its chemical structure and dopamine (DA) similarity, 6-OHDA can be taken up by DA nerves and oxidatively decomposed to generate toxic levels of reactive oxygen species, which ultimately induces DA neuron death [19]. However, 6-OHDA characteristically induces retrograde degeneration of DA neurons and nerve fibers, an effect that has regional differences in susceptibility and the differential generation of dopamine neuron compensation in other regions [20, 21, 22].
Recently, increased attention has been paid to the role of the dopaminergic nervous system in the mechanism of OCD. Several studies have suggested that there is a considerable anatomical correlation between the dopamine transmitter system and the OCD loop theory [23, 24, 25]. Physical interventions, such as surgery on neurons or nerve fibers along neural circuits, may lead to corresponding changes in neurotransmitter release, which can help treat obsessive-compulsive symptoms [26, 27]. Clinical study by the current and other authors have shown that deep brain stimulation (DBS) of the ventral middle segment of the anterior limb of the internal capsule is a better target than the nucleus accumbens (NAC) and subthalamic nucleus (STN) for improving obsessive-compulsive symptoms but with higher stimulation parameters [28]. It is supposed that OCD possibly exists in multiple pathological neural circuits, with the medial forebrain bundle and the anterior thalamic radiation subserving different OCD loops. DBS high-energy stimulus or radiofrequency ablation causes widespread damage to the fibers of the anterior limb of internal capsule (AC) and simultaneously suppresses multiple neural circuits [29, 30]. Therefore, AC intervention provides a better curative effect than individual targets in any other single neural circuit. If this hypothesis is correct, the question becomes how the various OCD circuits are arranged in the AC region, as it is not clear which is more critical in the OCD mechanism.
In this study, we established a 6-OHDA OCD animal model, in which we pathologically analyzed the structural changes of both the DA neurons in various brain regions and nerve fibers associated with OCD. We then combined these findings with the results of behaviour evaluation in animal models of OCD to describe the DA neural circuits related to OCD.
A total of 52 male Sprague Dawley (SD) rats (5 weeks, 150–200 g) were purchased from Dahuo Animal Company (Chengdu, China) and housed in a specific pathogen free (SPF) grade animal laboratory at the Southwest Medical University. Groups of six rats were housed in a translucent box (35 cm
The 52 SD rats were divided randomly into QNP model groups (n = 46) and one saline control group (NS group, n = 6). A subcutaneous neck injection of QNP (Q102, Sigma-Aldrich, St. Louis, MO, USA; 0.5 mg/kg dissolved in saline, NaCl 0.9%, at a volume of 1 mL/kg) was given twice a week for a total duration of 5 weeks to the 46 QNP group rats. Ten minutes after each injection, the rats were observed and recorded to determine whether they continued typical foraging behaviour (exploring the ground or an object with the nose for at least 5 sec), grooming, and other compulsive behaviours. A subcutaneous neck injection of saline (1 mL/kg; NaCl 0.9%) was also similarly given twice a week to each of the six rats in the NS group.
To verify the accuracy of coordinates of each surgical target, much early work was required. Target coordinates were obtained from the anatomical map of rats (Paxinos & Watson, 1997): NAC (2 mm anterior to bregma, 1.5 mm lateral to the midline, and 8.5 mm ventral to skull); AC (1.5 mm posterior to bregma, 3 mm lateral to the midline, and 7.1 mm ventral to skull); MD (3 mm posterior to bregma, 0.7 mm lateral to the midline, and 5.5 mm ventral to skull).
After the model setup, 46 QNP rats were randomly divided into five groups: 6-OHDA anterior limb of internal capsule (AC) stereotactic injection group (QNP+AC group, n = 10), 6-OHDA mediodorsal thalamic nucleus (MD) stereotactic injection group (QNP+MD group, n = 10), 6-OHDA nucleus accumbens (NAC) stereotactic injection group (QNP+NAC group, n = 10), saline (NS) stereotactic injection group (QNP+NS-S group, n = 10), and non-surgical group (QNP+Non-S group, n = 6). In the NS group, rats simultaneously received a 6-OHDA stereotactic injection (NS+6-OHDA-S group, n = 6: AC2, MD2, NAC2).
Rats were anaesthetized for surgery with 2% sodium pentobarbital (P3761, Sigma-Aldrich, St. Louis, MO, USA; 60 mg/kg) intraperitoneal injection, fixed on the animal stereotaxic, and the tooth and ear rods were adjusted to fit appropriately. After confirmation of no active bleeding, a 5-µL trace syringe was slowly inserted intracranially to reach targets. A semi-automatic constant rate trace injection pump injected 12.5 µg 6-OHDA (H116-5 mg, Sigma, Lot# 066M4602V, Pcode:1002800500, USA, 1 µL/5 µg) within 2 min into the targets, making the drugs fully diffuse. The same procedure was applied to the other side of the injection group (normal saline injection in the same way). The operation was completed, and a 38 °C constant temperature water bath blanket was used for rewarming. When fully awake after anesthesia, the rats were put back into their original environment.
First, it was verified whether the behavior of the rats tested in the groups differed significantly from that of rats tested separately. Twenty-four rats with the same conditions were randomly divided into four groups, with six in each group. After the injection of QNP, each rat in group A was evaluated separately, whereas after injection of QNP, all three rats in group B were evaluated together; after the injection of normal saline, each rat in group C was evaluated separately; after the injection of normal saline, all three rats in group D were evaluated together. The results showed no significant differences in behaviour between groups A and B or C and D (Table 1). Therefore, in formal experiments, we took the approach of placing three rats simultaneously on an open platform for behavioral assessments (a schematic of behavioral assessment is shown in Fig. 1). The Noldus EthoVision XT (Noldus Information Technology BV., Beijing, China) behavior observation, record, and analysis system recorded and analyzed the behavior of the rats in detail. After the evaluation of each group, any rat feces on the open platform were removed, and the venue was cleaned and disinfected to avoid interference with subsequent observations.
| Group | NOH | ATBO (s) | TDM |
| A | 14.6 (6.7) | 19.7 (2.7) | 301.9 (78.9) |
| B | 15.3 (4.6) | 19.1 (5.5) | 298.3 (88.5) |
| C | 3.2 (1.1) | 148.3 (48.5) | 83.1 (48.3) |
| D | 3.6 (1.5) | 151.5 (52.1) | 82.2 (51.1) |
NOH, number of home base visits; ATBO (s), average time between each home base visit; TDM, total distance travelled.
 Fig. 1.
Fig. 1. Behavioral assessment and modeling schematic. The open site platform size was 160 cm
Rodents characteristically explore new things and seek shelter. Szechtman et al. [13] observed that rats visited a box on the open platform the most and stayed the longest in a certain period after QNP injection, so it was defined as “home”. The rats’ behavior was mainly analyzed as the behavioural indicators related to “home”. The home base consisted of four transparent glass boxes (10 cm
Number of home base visits (NOH): the box with the most visits was identified as the home base [13]. The total number of home base visits within 30 min was recorded. Most parts of a rat’s head and at least one forepaw went into the glass box for at least 1 s per “home” visit, and if they either visited the same “home” within a 3-s interval or there was a clear tendency to move away from home but then returned, this was counted as a single visit.
Average time between each home base visit (ATBO) (s): the average time interval between each trip to and from the home base within 30 min [13].
Total distance travelled (TDM) (number of squares): the total number of squares entered by each rat during the 30 min observation period was counted [13].
The rats were decapitated under deep anaesthesia (2% sodium pentobarbital 60 mg/kg), before which QNP was subcutaneously injected for the last time. Frozen specimen sections in the coronal plane at a 5-µm thickness were obtained from six brains of each group. There were four consecutive coronal sections for each region. Verification of placements was performed using the atlas of Paxinos and Watson. Only injections placed correctly in the target area were included in the statistical analysis of results. The sections were soaked in 0.1% Triton X-100 for 30 min, then blocked by 1% bovine serum albumin (BSA) for 1 h, followed by incubation with rabbit anti-tyrosine hydroxylase (TH) (ab6211, Abcam, Cambridge, MA, USA; 1:1000) for 48 h at 4 °C. The sections were then washed three times with PBS (15 min per wash) and incubated with Alexa Fluor™ 647 Donkey anti-Rabbit IgG (ab150075, Abcam, Cambridge, MA, USA; 1:500) overnight at 4 °C. Images were collected as soon as possible under an orthotopic two-photon laser confocal microscope (NIKON, Tokyo, Japan). Finally, the results were analyzed using the NIS-Elements BR image analysis system (NIKON, Tokyo, Japan).
SPSS version 19.0 (IBM, Armonk, NY, USA) was used to process data; measurement data were expressed as mean
After 5 weeks of QNP injections, the rats showed significant compulsive behaviour in the open field, and the number of “home” visits (NOH) in each group was nearly 5–7 times that of the NS+6-OHDA-S group. The results of the Mann-Whitney U analysis indicated that all the QNP groups were significantly different to the NS+6-OHDA-S group 2.6 (1.7) and the results were as follows: QNP+AC group 16.6 (5.2), Z = –3.261, p = 0.001; QNP+MD group 14.3 (5.8), Z = –3.259, p = 0.001; QNP+NAC group 14.2 (4.9), Z = –3.271, p = 0.001; QNP+NS-S group 13.9 (5.1), Z = –3.261, p = 0.001; QNP+Non-S group 13.3 (4.6), Z = –2.887, p = 0.004. The grade of NOH results at the 5-week time-point were as follows: 10 rats extremely severe (more than 20), 14 rats severe (16–20), 14 rats moderately severe (11–15), four rats mild severe (6–10), and four rats invalid (0–5). The same results were obtained for ATBO and TDM, with all p-values
| Group | NOH | ATBO (s) | TDM |
| QNP+AC | 16.6 (5.2)* | 18.3 (5.5)* | 313.2 (75.5)* |
| QNP+MD | 14.3 (5.8)* | 17.9 (6.3)* | 293.0 (92.7)* |
| QNP+NAC | 14.2 (4.9)* | 18.8 (5.7)* | 323.2 (86.9)* |
| QNP+NS-S | 13.9 (5.1)* | 17.4 (6.1)* | 309.8 (98.1)* |
| QNP+Non-S | 13.3 (4.6)* | 18.7 (4.3)* | 314.5 (97.9)* |
| NS+6-OHDA-S | 2.6 (1.7) | 147.5 (55.2) | 78.2 (53.4) |
*: Significant statistical difference compared with the NS+6-OHDA-S group, p
After the rats received a QNP injection for 3 weeks post-surgery, open-field NOH was reduced to different degrees in the three target groups (QNP+AC, QNP+MD, and QNP+NAC groups) (Fig. 2a). The Wilcoxon signed rank test results indicated differences between pre-surgical 16.6 (5.2) and 3-week post-surgery 12.4 (4.6), Z = –1.901, p = 0.057 in the QNP+AC group; pre-surgical 14.3 (5.8) and 3-week post-surgery 8.8 (3.9), Z = –2.316, p = 0.021 in the QNP+MD group; and pre-surgical 14.2 (4.9) and 3-week post-surgery 11.3 (4.3), Z = –1.480, p = 0.139 in the QNP+NAC group. The QNP+MD group showed the most remarkable improvements (p
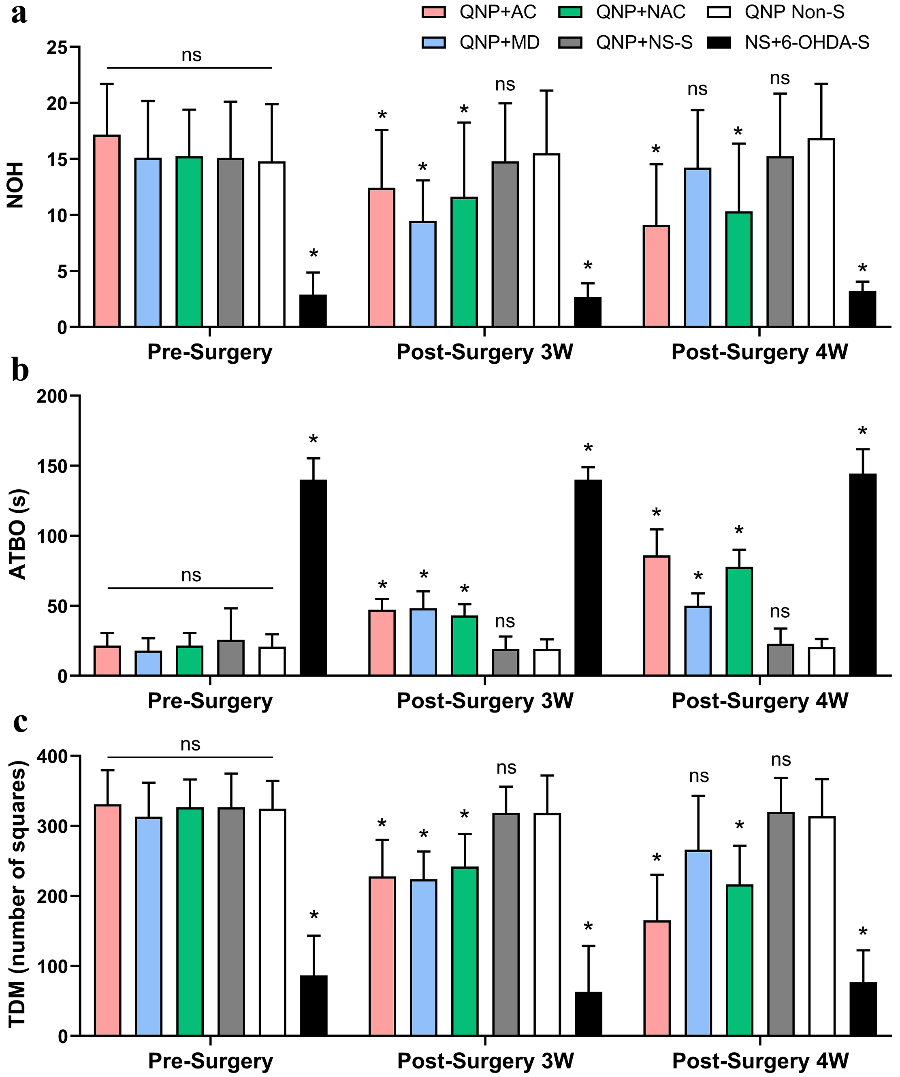 Fig. 2.
Fig. 2. Behavioral changes of rats in each group before surgery, and 3 and 4 weeks after surgery. (a) Statistical analysis of NOH, (b) ATBO, and (c) TDM at three time points in each group. Compulsive behaviors of rats in the QNP+AC, QNP+MD and QNP+NAC groups were significantly improved after surgery, especially in the QNP+AC group. *Significant statistical difference compared with the QNP+Non-S group, p
Immunofluorescence image acquisition at 4 weeks post-surgery showed TH staining in the corresponding target regions (internal capsule (IC), MD, NAC and ventral tegmental area (VTA)) was significantly reduced in the three 6-OHDA-injected groups (QNP+AC, QNP+MD, and QNP+NAC) compared with the QNP+Non-S group (Fig. 3a,b). TH fluorescence was widely seen in all regions of the QNP+Non-S group, among which the IC region is mainly composed of DA nerve fibers, while the NAC, MD, and VTA regions are primarily composed of DA neurons. TH fluorescence analysis in each region of the QNP+AC group indicated that the fluorescence of DA nerve fibers across the IC region was significantly reduced. DA neurons in the VTA region were decreased, and a comparison between the QNP+AC group 79.3 (27.6) and QNP+Non-S group 184.1 (23.6) in the VTA region, Z = –2.446, p = 0.017, was found to be statistically significant. On the contrary, the NAC and MD regions showed no significant change. TH fluorescence analysis of each region in the QNP+MD group indicated that the fluorescence of DA neurons in the MD region was significantly decreased. While DA nerve fibers across the IC region were also partially reduced, the central areas were concentrated in the middle segment’s medial part. DA neurons in the IC region in the QNP+MD group 143 (58.3) were compared with the QNP+Non-S group 238 (72.6), Z = –1.473, p = 0.037, and the difference was statistically significant. TH fluorescence analysis of all regions in the QNP+NAC group indicated that, compared with the QNP+Non-S group, the numbers of DA neurons in the NAC and VTA regions were decreased. The number of DA nerve fibers across the IC region was also partially reduced. However, the MD region showed no significant change in DA neurons.
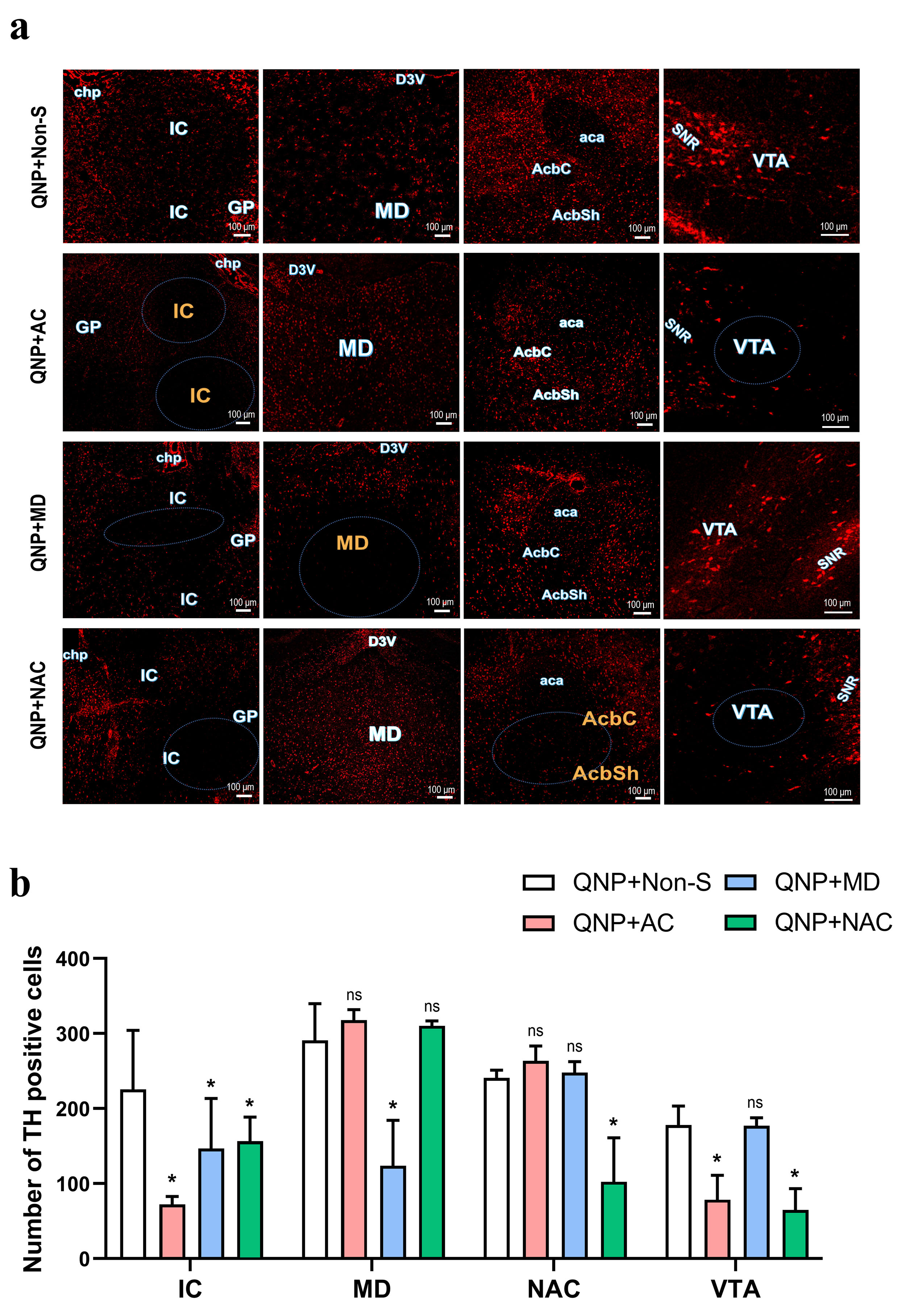 Fig. 3.
Fig. 3. Immunofluorescence analysis of dopamine neurons and fibers. (a) Representative images of TH (red) immunofluorescence staining (the scale bar represents 100 µm). IC, Internal capsule; GP, Globus pallidus; chp, Choroid plexus; MD, Mediodorsal thalamic nucleus; D3V, Dorsal 3rd ventricle; AcbC, Core of nucleus accumbens; AcbSh, Shell of nucleus accumbens; NAC, nucleus accumbens (including AcbC and AcbSh); aca, Anterior union; VTA, Ventral tegmental area; SNR, Reticular part of substantia nigra. (b) Immunofluorescence expression analysis of dopamine neurons and fibers in rats of each group. *Significant statistical difference compared with the QNP+Non-S group, p
Many studies have confirmed that the time window of action of 6-OHDA is between 3 and 4 weeks, with the most pronounced effect around 4 weeks [21, 31]. Therefore, the behaviour of rats was analyzed at 3 and 4 weeks post-surgery. Our results showed that all three intervention groups (QNP+AC, QNP+MD, and QNP+NAC) exhibited different degrees of remission in compulsive behaviours. At 3 weeks post-surgery, rats in the QNP+AC, QNP+MD, and QNP+NAC groups showed different degrees of reduced compulsive behaviours. At 4 weeks post-surgery, compulsive behaviours continued to decrease in the QNP+AC and QNP+NAC groups, while they increased in the QNP+MD group. These results indicate that the damage caused by 6-OHDA to each target DA neuron or nerve fiber has an ameliorative effect on compulsive behaviours induced by QNP.
Fluorescence staining at 4 weeks post-operatively showed that staining in the corresponding target area (IC, MD, NAC, and VTA) was significantly reduced compared with the QNP+Non-S group. These results indicate that 12.5 µg 6-OHDA after 4 weeks of observation is sufficient to cause significant damage to DA neurons and nerve fibers. The behaviour of rats in each group also changed to varying degrees, also demonstrating that 6-OHDA had a qualitative effect on the brain’s DA system. This is consistent with the majority of previous studies [21]. When Healy-Stoffel et al. [21] infused adult male rats with 12.5 µg 6-OHDA in the monolateral striatum 14 days after treatment with 6-OHDA, and the number and morphology of dopaminergic cells in the brain changed significantly. Sauer et al. [31] used a unilateral 20-µg injection in the striatum. Brus et al. [32] found that in adult rats with 6-OHDA undergoing whole brain injury, endogenous striatum DA decreased by 99%, and quinpirole did not produce enhanced motor or stereotypical activity. The number of dopamine neuron-specific TH immunoreactive cells in the substantia nigra decreased by 44% at 4 weeks, and the surviving ipsilateral fluorescent marker cells showed a 63% TH immunoreactivity after injection. Blandini et al. [22] showed that dopaminergic terminal damage was caused by early injection of 6-OHDA into the striatum, followed by a slow progression of dopaminergic cell body loss in the dense part of the substantia nigra, peaking at 28 days.
Many reports confirm that the VTA region has numerous dopaminergic neuronal fibers projected into the NAC region [33, 34, 35]. TH fluorescence analysis in the QNP+NAC group suggested that the number of DA neurons in the NAC region decreased, and the n umber of DA neurons in the corresponding VTA region was also slightly reduced. This phenomenon indicates that 6-OHDA enables corresponding damage to nerve fibers associated with DA neurons. The number of TH positive cells in the QNP+MD was reduced in the MD region, however an increase in the NAC and VTA was not observed (non-significant differences compared with QNP+Non-S).
The behavioral evaluation results showed that the compulsive behaviour of rats in the QNP+MD and QNP+NAC groups was significantly reduced compared with the QNP+Non-S group, which confirmed that both targets are associated with the obsessive loop. Fluorescence analysis confirmed that the DA nerve fibers in the IC region were damaged to varying degrees when the DA neurons were damaged in the NAC and MD regions. In addition, the behavioral evaluation results showed that the improvement of compulsive behavior at 4 weeks post-operatively in the QNP+AC group was better than that of the QNP+MD and QNP+NAC groups. Therefore, we conjecture that the internal capsule might be the confluence of the two DA-forcing circuits in which the MD and the NAC are located. This may also explain to some extent why clinical studies have found that DBS stimulation of the ventral middle segment of the internal capsule forelimb was more effective than NAC and STN in treating OCD but required higher stimulation parameters.
In this study, the expression of DA neurons was analyzed by broad-spectrum TH antibody fluorescence staining, while QNP is mainly a D2R and D3R agonist. Five different receptors (D1 to D5) are known in the dopamine system. Therefore, the search for more specific D2R and D3R detection antibodies is needed for future improvement. The intervention characteristics of 6-OHDA on DA-associated neural circuits provide many possibilities for study of the OCD mechanism. Optogenetic techniques may also greatly help the study of different OCD loops and their mechanisms of interaction.
The intervention of a dopaminergic-associated target on the forced loop by 6-OHDA can somewhat alleviate compulsive behaviour. Intervention in the medial forebrain bundle OCD loop was more effective than the anterior thalamic radiation loop where the MD is located. In addition, the dopaminergic nerve fibers of the above two OCD loops may pass through specific areas of the internal capsule. Thus, the internal capsule might be the best target for the treatment of OCD.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
HZ: Conceptualization, Data curation, Formal analysis, Investigation, Writing-original draft. RH, YM and HH: Formal analysis, Sample collection, Investigation. LC, WW and FG: Conceptualization, Supervision, Project administration, Funding acquisition, Writing-review. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This study was approved by the Ethics Committee of Southwest Medical University (approval number: 20231016-011).
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.



