1 Faculty of Medicine, University Montpellier, 34295 Montpellier, France
2 Faculty of Medicine, Université Laval, Quebec, QC 2G3, Canada
3 Faculty of Nursing, Université Laval, Quebec, QC 2G3, Canada
4 CERVO Brain Research Center, Quebec, QC 2G3, Canada
5 Institute for Neurosciences of Montpellier (INM), University Montpellier, INSERM, 34295 Montpellier, France
6 Department of ENT and Head and Neck Surgery, University Hospital of Montpellier, 34295 Montpellier, France
Academic Editor: Yoshihiro Noda
Abstract
Depression is a major public health issue in numerous countries, with around 300 million people worldwide suffering from it. Typically, depressed patients are treated with antidepressants or psychological therapy or a combination of both. However, there are some limitations associated with these therapies and as a result, over the past decades a number of alternative or complementary therapies have been developed. Exercise is one such option that is supported by published extensive basic and clinical research data. The aim of this review was to examine the beneficial effects of exercise in depression. Physical activity and exercise have been shown to be effective in treating mild-to-moderate depression and in reducing mortality and symptoms of major depression. However, physical activity and exercise are still underused in clinical practice. This review attempts to propose a framework to help clinicians in their decision-making process, how to incorporate physical activity in their toolkit of potential therapeutic responses for depressed patients. We first summarize the interactions between depression and physical activities, with a particular focus on the potential antidepressant physiological effects of physical activity. We then identify some of the barriers blocking physical activity from being used to fight depression. Finally, we present several perspectives and ideas that can help in optimizing mitigation strategies to challenge these barriers, including actions on physical activity representations, ways to increase the accessibility of physical activity, and the potential of technology to help both clinicians and patients.
Keywords
- depression
- exercise
- first-line interventions
- mental health
- physical activity
Depression is one of the most common mental illnesses that has a serious impact on the quality of life. It can affect anyone at any age. It is estimated that worldwide, 300 million people suffer from depression [1], with 4.4% of the global population affected, of which 5.0% are adults and 5.7% of people aged over 60 [2]. Depression is characterized by persistent symptoms of sadness, lack of interest or pleasure, disturbed appetite or sleep, lack of energy and self-esteem, anxiety and feelings of worthlessness [3]. At worst, depression can lead to suicide, which is the fourth leading cause of death among 15–29-year-olds [2]. In addition to mental-health problems, people suffering from depression are often affected by behavioral and biological characteristics that are deleterious to physical health, especially in the cardiovascular system [4]. When depression occurs as a result of pre-existing issues, it may exacerbate them, and even increase the related mortality of these pre-existing conditions [5, 6, 7].
The etiology of depression is complex, partly unknown and influenced by multiple factors, including genetic susceptibility, socioeconomic factors (e.g., economic instability and unemployment, poor nutrition), environmental factors (i.e., noise and chemical pollution) [8, 9, 10, 11, 12], other lifestyle factors and events (e.g., stress and emotional trauma, drugs and alcohol) [13, 14, 15], and dysregulation of pertinent homeostatic systems (e.g., immune system, hypothalamic–pituitary–adrenal axis and autonomic nervous system, and altered levels of pro-inflammatory markers) [16, 17, 18]. In addition, physical health problems such as sleep disorder, chronic pain, diabetes, and cancer can also contribute to depression [19].
Although depression can be diagnosed in primary care and can be treated with pharmacological agents and psychotherapy with a success rate of ~72% and 50% for antidepressants and psychotherapy, respectively [20, 21, 22], only 10 to 25% of those affected by depression receive treatment for their depression symptoms [23]. This situation might be due either to a lack of resources and/or the social stigma associated with the depression [20]. There is, therefore, an urgent need for cost-effective ways to reach a larger number of people to treat the symptoms of depression and improve the physical and mental health of those affected [24]. One of these interventions is physical activity. Physical activity is defined as any bodily movement produced by skeletal muscles and that requires energy expenditure [25]. It encompasses various types of movements motivated by transport or leisure that have different impacts on depression, and more broadly on health. Exercise is one type of physical activity defined as a planned, structured, and repetitive movement of the body designed to enhance or maintain physical fitness [26]. Physical activity through exercise is increasingly recognized as both a preventive intervention, from universal to targeted prevention [27], and as an antidepressant agent [28], and could even, to some extent, delay mortality [29]. Indeed, physical activity through exercise has been associated with lowered depression levels in several clinical and general populations, with physically active individuals reporting lower levels of depression than individuals that do not engage in daily exercises [30]. However, although much evidence supports the beneficial impacts of physical activity on depression, integrating physical activity as a therapeutic tool in first-line clinical settings remains a challenge.
This review aims to provide a broad overview of the research involving the integration of physical exercises into the prevention and first-line treatment of depression in clinical settings, on the barriers limiting the use of exercise as a clinical tool, and on how to implement strategies to mitigate these barriers. We first describe the beneficial effects of physical exercises on the prevention and treatment of depression, and present guidelines regarding the types of exercises that can be translated into first-line clinical settings. Then, we address the factors impacting the patients’ engagement in physical exercise intervention programs. Finally, we propose mitigating strategies to enhance the integration of physical exercises into the prevention and treatment of depression in first-line clinical settings.
The interactions between biological and psychosocial processes and depression have been covered elsewhere, and a negative association between regular physical activity and depressive and anxiety disorders was established using several meta-analyses [30, 31, 32].
Beneficial effects of physical exercises in preventing and in treating depression are well documented [33, 34]. Prevention relying on physical activity shows potential both non-specifically and specifically, by acting upon the causes of depressive symptoms among the general population, as well as in vulnerable individuals [35]. Indeed, evidence shows that exercise can act as a protective factor against the development of depression [36]. In some studies, exercise was shown to be associated with a decreased risk of depression, with a 30% smaller risk than in populations which did not engage in exercise programs [19, 37, 38]. A recent study using a large population cohort that was prospectively followed for 11 years (33,908 adults without symptoms of common mental disorder or limiting physical health problems) demonstrated that regular exercise was associated with a reduced incidence of future depression, but not of anxiety. This observed protective effect was seen regardless of the intensity of the exercise undertaken, the sex, or the age of the participants. Assuming that the observed relationship is causal, their results suggest that if all participants had exercised for at least 1 hour each week, 12% of depression cases at the follow-up could have been avoided [39]. Physical activity could also be effective for targeted prevention. For instance, those elderly who remain physically active over time demonstrated lower levels of symptoms of depression compared to those adopting inactive lifestyles as they aged [40].
Physical activity could be used as preventive interventions that act through improving sedentary lifestyles, physical health, boosting confidence, promoting social interactions, and increasing release of neurotransmitters like endorphins, dopamine, and serotonin that boost mood [31, 41]. Acting on the causes of depression reduces the risk of developing depressive symptoms that necessitate treatment. Regular exercise is now recognized as an important lifestyle activity that can mitigate the negative impact of chronic diseases on physical health [42] as well as on depression [32, 33, 38, 43].
Conventional treatments for depression (e.g., medications and psychotherapy) reduce depression, but not the morbidity/mortality in cardiac patients [44, 45]. In contrast, in patients with coronary heart disease, cerebral stroke, heart failure and diabetes, physical activity reduces mortality to a similar extent as medications [46]. Even if the beneficial effects of exercise and physical activity on cardiovascular morbidity/mortality may be independent of their effects on depression, both effects (on mental and on physical health) are positive for the patients’ quality of life, if not simply for their survival. Furthermore, exercise contributes to reducing and managing weight [47, 48, 49] and to improving the quality and duration of sleep [50].
Interestingly, physical activity could contribute to decreasing the adoption of lifestyles associated with depression. For instance, although the evidence supporting the effectiveness of exercise in promoting abstinence from some consumption behaviors, such as tobacco [51] or alcohol [52], is scarce and inconclusive, the effect on reducing consumption of illegal substances is more conclusive [53].
While in clinical settings depression is commonly treated with medication and psychological therapy [54, 55], interventions based on physical exercises are increasingly recognized as an affordable, non-invasive, and easily accessible therapeutic means for the treatment of depression and of other mental health disorders [5, 56]. Randomized and crossover clinical trials showed that exercise programs are efficient as a treatment for depression in both young and older individuals [57, 58]. Specifically, exercises are effective for treating mild-to-moderate depression [59, 60, 61] and for reducing the mortality, while improving clinical outcomes of major depression [62]. Benefits from treatment programs relying on exercises could even be similar to those achieved with antidepressants [57]. Combining medication treatment with exercise also showed clear effects on depressive symptoms. Indeed, adding exercise to antidepressants primarily affected the main symptoms of depression rather than somatic symptoms [62]. Patients receiving aerobic exercise and antidepressants had greater improvements in cognition and autonomic balance compared to those only receiving antidepressants [63, 64]. Interestingly, these types of combined interventions were well received by both patients and physicians [65].
Several studies have shown the effectiveness of exercise interventions to reduce the symptoms of depression in specific populations. Exercise alone, or in combination with drugs, was also effective in treating patients with treatment-resistant depression [66, 67]. Exercise may be effective for treating patients who have contraindications for drug therapy (e.g., adolescents or pregnant women or women with postpartum depression [68, 69, 70]. For elderly patients, exercise interventions are very promising at mitigating the symptoms of depression without causing significant side effects [71, 72]. Enhancing physical activity through exercise also effectively reduced depressive symptoms among patients with physical comorbidities, such as hypertension, cardiovascular disease, or Alzheimer disease [73, 74, 75]. Indeed, aerobic exercise was beneficial in improving symptoms of depression and the quality of life of patients recovering from a heart attack [76].
Taken together, physical activity may present beneficial effects both in treating and in challenging the causes of depressive symptoms. However, evidence for a beneficial effect of exercise interventions on the prevention and treatment of depression differs substantially across different studies. Indeed, some systematic reviews found that exercise is only moderately more effective than a control intervention for reducing symptoms of depression [55] or may only have small, short-term effects in mitigating symptoms of depression [77], while others recognized that physical activity and exercise have evident antidepressant effects [78, 79, 80, 81, 82]. These differences may be explained by inclusion criteria, heterogeneity in study population and type of exercise intervention, and different degrees of bias in the study design [83]. Indeed, when only high-quality trials were considered, the effect size for exercise benefit became smaller [55, 78, 81]. Finally, Schuch et al. [84], showed that compared to control conditions, exercise had a large and significant effect on depression when they included only randomized, controlled trials of exercise interventions in people with either a diagnosis of major depressive disorder or ratings on depressive symptoms.
The UK’s National Institute for Health and Clinical Excellence (NICE) has guidelines for the treatment of mild-to-moderate depression and persistent subthreshold depression [85]. These guidelines recommend that people with persistent subthreshold depressive symptoms or mild-to-moderate depression should: (i) be handled in groups with support from a competent practitioner; and (ii) therapies should consist typically of three sessions per week of moderate duration (45 minutes to 1 hour) over 10 to 14 weeks (average 12 weeks) [85]. The easiest and safest way to exercise is by walking — at least 10,000 steps/day or 6000 steps/day in addition to other daily activities [86]. However, offering patients several types of exercises to choose from according to their own preferences could improve compliance [85, 87], especially for depressed older adults [88]. The clinician’s final recommendation of an activity program will need to consider the patients’ preferences as well as the factors that might hinder their engagement in the proposed program. These will be discussed in the following section.
In addition, in 2021 an independent NICE guidelines committee developed the first recommendation in 12 years based on the review of evidence on the treatment of new depressive episodes, chronic depression, prevention relapses, patient choice, organization, and access to mental health services. The committee created a menu of treatment options to allow patients in a shared decision-making discussion between them and their healthcare professional to choose the right one for them. Indeed, patients with less severe depression could choose from the menu as first-line treatment options: e.g., cognitive behavioral therapy (CBT), exercise, counseling, or psychotherapy. A similar range of psychological interventions, along with the option of antidepressant medication, is available for those choosing first-line treatment for more severe depression [89]. The Canadian Network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder has recommended that exercise may be used as a first-line monotherapy for mild to moderate major depressive disorder and a second-line adjunctive treatment for moderate-to-severe major depressive disorder, based on the lack of long-term data and feasibility issues [90]. The Swedish National Institute of Public Health recommended prescriptions for physical activity and exercise in a group or individual setting, to reduce the risk of developing depression and treat clinical depressive disorders. This document estimated that physical activity and exercise may have similar effects that differ from other classical antidepression treatments such as medication and/or psychotherapy [91]. Finally, the Physical Activity Guidelines for Americans 2nd edition, 2019 conducted a multifaceted, robust analysis of the available scientific literature in the fields of physical activity, health, and medicine to provide recommendations to the Federal Government on physical activity, sedentary behavior, and health. This report recognized that regular moderate-to-vigorous physical activity reduces feelings of anxiety and depression and improves sleep and quality of life. Even a single episode of physical activity provides temporary improvements in cognitive function and state anxiety. Adults who are more physically active are better able to perform daily tasks without excessive fatigue [92]. However, these guidelines have potential weaknesses. Indeed, not all of them are based on up-to-date literature, and most lack evidence from meta-analyses, including relevant control conditions and the adequacy of blinding. This might impact the recommendation power of these guidelines, since when only high quality trials were considered, the effect size for exercise benefit became smaller [55, 78, 81]. There is also evidence that exercise has better adherence when supervised by trained practitioners, so applicability may be an issue [93].
From a first-line health-professional perspective, helping patients suffering from depression to initiate and maintain the practice of physical activity is no small undertaking. Exercise programs are generally heterogeneous, with different features that influence their effects on depressive symptoms. Yet, research offers some insights regarding the exercises programs that can be suggested. Four factors need to be considered when designing an exercise program for depressed patients: exercise type, intensity, frequency, and context (Fig. 1).
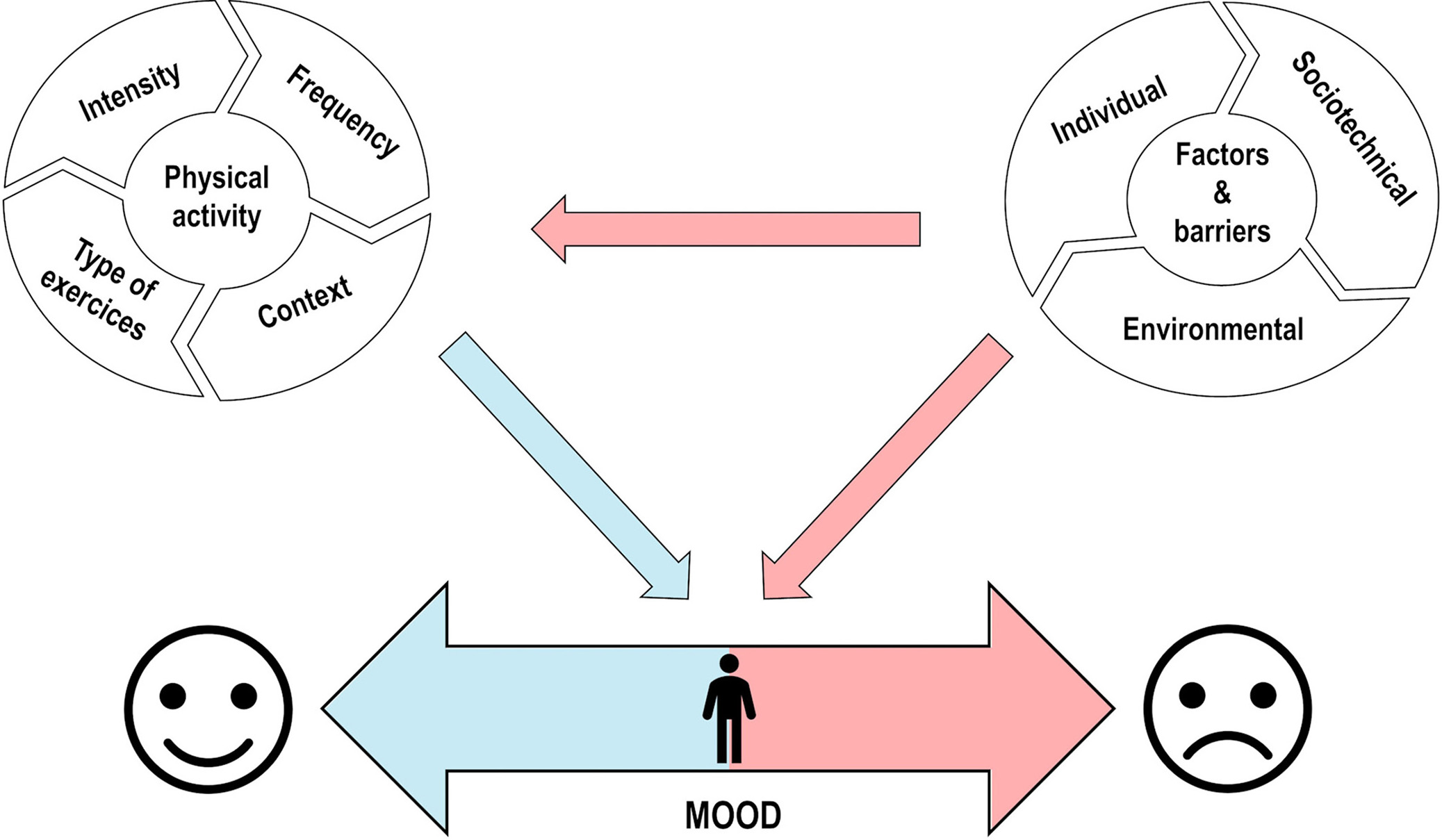 Fig. 1.
Fig. 1.Interplay between physical activity and external factors on mood. This schematic figure represents the interplay between the effects of physical activity and factors and barriers on mood. The bottom line presents a continuum of mood on which individuals can move to positive affect (left side) or to negative affect (right side). The left circle displays the four factors to consider when designing an exercise program for depressed patients. The blue arrow represents the positive effects that physical activity has on mood. The right circle represents the factors and barriers affecting the engagement of depressed patients in physical activity and exercise (horizontal red arrow) as well as affecting patients’ mood (diagonal red arrow).
The first factor is the type of exercise that is proposed in the intervention program. Exercise regimens are broadly categorized into three major types that have all been found to have positive effects on depression: aerobic, resistance, or mind-body exercise types [60, 94, 95]. It is well established that independent aerobic or resistance exercise regimens only elicit different metabolic and phenotypic adaptations, whereas mind-physical exercise is unique as a low impact form of exercise [96]. Any individual exercise program may include several combinations of these exercises [96]. Aerobic exercise consists of any type of cardiovascular conditioning. This category includes activities like walking, jogging, running, swimming, or cycling. Aerobic exercises imply an increase in metabolism (which require increased breathing), heart rate, and blood flow [97]. Resistance exercises consist of any exercise that causes the muscles to contract against an external resistance with the expectation of increases in strength, and inducing a stronger connection between the musculature and nervous system [98]. Mind-body exercises are a form of exercise that combines body movement, mental focus, and controlled breathing to improve strength, balance, flexibility, and overall health [99]. Yoga, tai chi, and qigong are well-known forms of mind-body exercise. Aerobic, resistance, and mind-body exercises have shown beneficial effects on the mental health of young people [100]. A systematic review and network meta-analysis of randomized controlled trials demonstrated that such exercises are all effective treatments for depression symptoms in elderly patients [88]. However, some studies show that the effectiveness of various types of exercise might also depend on the type and severity of the symptoms. In clinically depressed older adults, aerobic exercise might show a more favorable antidepressant effect than resistance exercise [101]. The mind-body exercise program could be more efficient than aerobic programs alone, suggesting that exercises incorporating both mind and body components might be more effective for older adults with mild- and moderate depressive symptoms [102].
There are three main types of exercise, all of which have been shown to have positive effects on depression: aerobics, muscle strengthening, and mind-body exercises [57, 58, 59]. Aerobic exercise is any type of cardiovascular conditioning. This category includes activities such as walking, jogging, running, swimming or cycling. Aerobic exercise involves an increase in metabolism, heart rate, and blood flow [60]. Muscle-strengthening exercises are any exercise that causes muscles to contract against external resistance with the goal of increasing muscle strength and inducing a stronger connection between the musculature and the nervous system [61]. Finally, mind-body exercises are a form of exercise that combines body movement, mental focus, and controlled breathing to improve strength, balance, flexibility, and overall health [59]. Yoga, tai chi and qigong are well-known forms of mind-body exercises.
The second factor is the intensity of the prescribed exercises. Exercises do not need to be of a great intensity to improve mood, as beneficial effects are observed in recreational exercisers as well as in marathon runners [103]. Therefore, improving mood states through exercise could be beneficial for non-exercisers as well as for recreational and expert ones. However, other studies show that moderate and high-intensity exercise programs are often considered to have a greater antidepressant effect [58, 94, 104]. Nonetheless, higher-intensity programs often have higher dropout rates [93], which would limit their large-scale use. Finally, studies also showed significant associations between the intensity and duration of physical activity interventions and their antidepressant effect [105, 106], albeit such a relation is likely to follow nonlinear models [107].
The third factor is the frequency at which the patient is expected to perform the exercises. The frequency of exercise is inversely associated with depression symptoms and overall well-being [38, 108]. High-frequency (3 to 5 exercise sessions per week) aerobic exercise interventions for 8 weeks have been shown to be more effective in reducing symptoms of depression than low-frequency interventions (one session per week) [109]. Evidence shows that adults receive the maximal benefits of exercise by regularly performing 150 to 300 minutes per week of moderate intensity, 75 to 150 minutes per week of vigorous-intensity activity, or an equivalent combination of moderate and vigorous aerobic activity [110].
The fourth and remaining factor is the context in which the exercises are to be performed. The beneficial effects of physical activity could be influenced by the context in which it takes place, in terms of settings and social connectedness [111]. The settings depend, at least partially, on the type of activity proposed. Aerobic activity can be performed outside in the open air, while resistance activity is typically performed inside in adapted settings. Furthermore, the efficiency of an exercise intervention on reducing depressive symptoms could differ according to the modalities through which it is delivered. Interventions delivered in groups and supervised by an instructor showed greater effect in reducing depression than solitary, unsupervised activity [28, 112, 113]. Clinicians’ advice and follow-up are very important to improve compliance and maintain adherence over time. The follow-up can be done through consultation, telephone calls [114], or telemedicine and/or eHealth strategies to increase compliance with exercise programs [115].
Although much evidence supports the use of physical activity and, more specifically, of exercise-based interventions for depressed patients, this type of intervention is still dramatically underused as a clinical tool, both for the treatment and the prevention of depression [62]. Although clinical awareness of such interventions could contribute to this situation, there are also numerous impediments that can limit the capability of depressed patients or patients who risk developing depression to engage in the programs proposed above. Several factors can act as a potential barrier affecting the engagement of depressed patients in physical activity and exercise — whether occurring in the context of spontaneous practice, or being part of clinical intervention programs (Fig. 1).
Clinical manifestations of depression include symptoms that interact with the capacity to engage in physical activities. Indeed, fatigue, low motivation, and energy levels are associated with depression and are known side effects of psychotropic drug use [116, 117]. Depressed patients identify their low personal physical activity behavior as an obstacle to engaging in physical activity treatment [118]. They also often express concerns about a lack of time [116, 119], physical illness, and poor health [119] limiting their engagement in physical activity programs. Health literacy, defined as the degree to which individuals have the capacity to obtain, process, and understand health information and services needed to make appropriate health decisions [120], should also be considered. Indeed, depressed patients are less inclined to engage in physical activity when they lack knowledge about the benefits of physical activity on mood [121, 122].
While there is evidence documenting the perceived barriers for patients, the barriers expressed by the clinicians to the prescription of exercise have received considerably less attention. However, earlier work suggested that clinicians do not primarily prescribe exercise to depressed patients because they lack the knowledge and training, have time constraints, or prefer to rely on more traditional psychotherapeutic methods to treat mental illness [123]. Recent work suggests that a clinician’s own positive experiences with exercises and physical activity behaviors have a significant impact on exercise prescription rates and willingness to advocate for the use of exercise to treat depression [124, 125]. Therefore, the clinician’s own experience is a factor to consider that can act both as a barrier and a facilitator.
Importantly, these barriers are not solely under the control of the individual, as some reside in the social determinants that conditioned the appearance of depressive symptoms in the first place — or that increased the risk of developing depression — and which contributed to maintaining depressive states. By barely considering the context in which the person evolves and the constraints imposed by their living environments, the person could experience additional failures, which can do more harm to vulnerable populations [126].
While the individual person does play a role in behavior change, this is not the only factor that influences health. Indeed, health in general — and mental health particularly — is deeply embedded in the environment in which we live. Environmental aspects, both social and physical, are necessarily deeply associated with socioeconomic considerations. Regarding the physical environment, the location or the place where the exercises are supposed to be performed is important. Although several situations could have been developed here, we will discuss the two that are more relevant in the context of an individual undertaking an exercise program for depression prevention or treatment. They can be summarized in two categories: home and neighborhood (including accessibility to public facilities and private structures such as gyms). Access to these places can vary from one individual to another, depending on socioeconomic considerations.
The question of whether the patient has access to equipment at home is critical. This notion of “equipment” encompasses various elements, from the physical space to perform the exercises to the specific home gymnastic equipment (e.g., yoga mat, resistance bands, weight bench, weights and dumbbells, treadmill, cross-trainer, etc.). The possibility — and probability — of possessing home equipment depends heavily on the socioeconomic status of the patient, as people with higher income can more easily afford to allocate home space to a home gym and to purchase basic or expensive equipment. While performing aerobic activities outside of the home might seem like a solution, the relation between physical activity and the neighborhood features might suggest otherwise.
Neighborhoods constitute locations that offer multiple opportunities to practice physical activities. While the mechanisms through which neighborhood features influences health are complex and multidimensional [127], studies suggest that they have direct impacts on depressive symptoms and on physical activity [128, 129, 130, 131]. These features arise both from the built environment and the social environment. Several characteristics of the built environment of the neighborhood have been associated with physical activity. The presence of equipment to support the practice of aerobic or resistance exercises in public parks and recreational environments is positively associated with a higher level of physical activity among the residents of the area [132]. Having sidewalks in the neighborhood offers the opportunity for older adults to practice walking, which is the physical activity mostly performed by this population [133]. The facilities in which patients can practice the prescribed exercises include, but are not limited to, fitness centers or gyms, community centers, and schools. Access to those different facilities may be challenging for socially and economically disadvantage individuals (e.g., fees for gym membership). Of note, neighborhoods housing economically disadvantaged populations present fewer characteristics or resources in the built environment that promote and support physical activity [134, 135]. Besides socioeconomic considerations, inequalities in the access to physical activity settings vary between different neighborhoods due to macrosocial considerations. For instance, weather and season constitute a barrier to engagement in open-air physical activity [136].
While the physical environment can have a major impact on the patient’s engagement in physical activity programs for depression, the social environment is also important to consider. While exposition to violence in the neighborhood is associated with depressive symptoms [131], the safety of the neighborhood is associated with increased chances of performing physical activity [134]. Safer environments may encourage outdoor aerobic activities, such as walking or running in the neighborhood. Furthermore, access to human resources is identified as a concern by depressed patients engaging in physical activity treatment [119, 137]. While the prescription might be provided by the physician, the professional who is most qualified to accompany the patient in the program might be someone specialized in movement science (e.g., physiotherapists, ergotherapists, and kinesiologists), if not an actual sports specialist (either trainer or coach). However, these professionals are not equally accessible in certain neighborhoods, with disadvantaged ones having less access to those resources.
Sociotechnical factors include opportunities and challenges coming from the interplay between social, economical, cultural, and global contexts resulting from the digitalization of society. Indeed, the ubiquity of technologies in all aspects of social and societal lives — especially in the COVID-19 aftermath — is currently undeniable [138, 139]. However, differences exist between individuals with regards both to access to technology and digital literacy — defined as the degree to which individual has the capacity, knowledge, motivation, and competence to access, process, engage in, and understand the information and the series of actions needed to obtain benefits from the use of digital technologies [139, 140, 141].
Digital technologies offer multiple opportunities in supporting the engagement of depressed patients in practicing physical activity exercises. However, these opportunities translate into challenges for digitally disadvantaged individuals. One of the basic challenges brought about by digital inequalities is related to the clinician’s use of technology as a follow-up tool. In a global context in which resources are scarce, clinicians will likely choose technologies to support follow-up contact with patients or with the professionals that accompany their practice of physical activity, instead of having to frequently meet in person. The choice of the modality used will depend both on the clinicians’ and their patients’ access to technology and digital literacy.
Depressed patients — and the population in general — can search online for information about physical-activity options that are available for them. As for health, services, or civic information [142, 143], one can seek complementary information about the prescribed exercises. Indeed, as for various health conditions, patients might not clearly understand the clinician’s recommendation in the first place and could subsequently look further for more precise information online [144]. This could take the form of online written content or video tutorials shared on social media. However, as physical activity is not strictly disseminated by health specialists, information — especially content created and shared on social media — is mostly uncontrolled, and carries the risk of misleading depressed patients. Also, patients could use a search engine to seek facilities and programs in their surroundings where they could practice the program prescribed by the clinicians. Digital inequalities interfere in all these online behaviors, as people with more digital skills also tend to have higher health literacy [145], meaning that they will likely have fewer difficulties in finding useful information and making informed choices that will be beneficial for them.
Another important aspect to consider, especially in the aftermath of the COVID-19 pandemic, is the possibility of following exercises classes live, or broadcast online. Indeed, at the peak of the pandemic, physical activity opportunities were limited. Individuals and communities needed to redefine how to practice physical activity, constantly keeping in mind — and being in line with — the sanitary measures in place at any given time. The result of this process was often to rely on digital technologies to provide physical activity services. However, the benefits that can be obtained from these reinvented physical activity practices rely heavily on the digital access and skills of the patients undertaking them, as well as on the home settings, e.g., place at home that makes it possible at the same time to hold the technological and the exercise equipment, and provide sufficient space to perform the exercises, while not restricting the potential activities of other family members.
While multiple factors contribute to the possibility for depressed or at-risk patients to engage in physical activity, clinicians are not responsible for challenging all of them. Indeed, their potential depends strongly on societal representations of both mental health and physical activity. Acting on these representations is critical to increasing the wide-scale adoption of physical activity as a clinical tool to help depressed or at-risk patients. Changing societal representations is something extremely complex. From a clinical sciences perspective, this must involve disciplines such as public health and health promotion [146]. Clinicians in first-line settings need to consider the numerous factors that impact the patients’ engagement in physical activity interventions programs. In particular, systematically including a health-promotion lens to their prescription of exercise should be taken into consideration.
Adopting such a perspective implies casting an eye on and considering the upstream factors and determinants that influence the patient’s engagement in physical activity, as well as promoting empowerment and participation. Fatigue and low motivation top the list of patient-reported barriers to exercise, and are also the hardest barriers to overcome, because they are integral to both depression and antidepressant medications [147]. Therefore, clinicians should be aware of the interplay between symptoms and treatment side effects. Potential mitigating strategies have to include actions to promote health literacy, notably by reminding their patients that physical activity and exercise can both improve depressive symptoms, increase energy levels, and combat fatigue in general [112]. By giving greater emphasis to the importance of exercise in a patient’s quality of life, and outlining both the physical and mental benefits they can get from regularly engaging in a prescribed exercise regimen, clinicians can support the development of the patient’s health literacy. However, to fully promote health literacy, the clinicians must not content themselves with reminders; they need to engage patients in the process of integrating physical activity and exercises in their everyday life. This implies promoting the empowerment and participation of the patients by involving them in determining which type of exercise they prefer and the context in which they want to do it. In an empowerment process, it is critical to ensure that patients have positive experiences while engaging in the creation and the realization of the programs that will be conceived specifically to answer their needs. This process might involve a discussion not only on the type of exercise to be performed, but also on its function. For instance, although recreational walking and useful walking both hold benefits for health in various ways, they serve different functions, which might be better suited for different patients.
To increase the likelihood of patient adherence, clinicians should always consider the overall health of patients and take any mobility-related complications into account when accompanying patients in the elaboration of individualized and specified exercise regimen [148]. They should not recommend an exercise modality that exceeds both the physical capacity and comfort of patients. This perspective helps to simultaneously challenge the barriers related to individual characteristics, such as the lack of time or availability [149]. The results from this process could be quite different from the program the clinician would have envisioned. Although physical activity could be beneficial for all depressed persons, the beneficial effects could be higher among individuals who already practice some physical activity [103], thus making empowering strategies quite profitable.
The transformation in physical activity representation could simultaneously contribute to increasing the accessibility of the practice of physical activity. The elements discussed above focused mainly on individual characteristics, or on the effect of the structural factors on individual capacities to engage in physical activity. However, clinicians also play a role — albeit limited — in challenging the structural barriers that constrain the patients’ engagement in physical-activity treatments and the prevention of depression. As influential members of most occidental societies, clinicians’ advocacy for environmental transformation can contribute to the decision processes of politicians, civil servants, and other decision makers [150]. This general strategy requires continuous information and exchanges with other health professionals, so that clinicians can increasingly adopt a conception of health that goes beyond the scope of in situ care within healthcare services.
In an integrated perspective, one of the keys to increase the accessibility of physical activity for depressed patients will be to enhance the inter-professional dialog in scope, in range, and in magnitude. First, the inter-professional dialog between medical doctors and other health professions will have to be increased. While this necessity for enhanced inter-professional dialog between health professionals has already been identified as a central aspect of modern clinical practice, this is a continuous process [151]. Furthermore, most efforts so far have been to increase cooperation between medical doctors and the professions generally encountered in hospital settings, i.e., pharmacists, nurses, and psychologists. Although these interactions are obviously highly valuable in the context of depression, interactions will have to be deepened with health professionals specializing in movement sciences, such as physiotherapists, ergotherapists, and kinesiologists, to name a few. However, there is another, broader kind of inter-professional dialog that needs to be furthered to increase the accessibility of physical activity for depressed patients. Beside the dialog among health professions, there is a need to further that between health professions on the one hand, and recreational professionals — including sports trainers and coaches, leisure specialists, managers of recreational facilities, etc. — on the other hand. In a modern, leisure-oriented society, recreational sciences have a responsibility for issues related to the health of the population. Academic curricula dedicated to training recreational professionals should include concepts on health, or at least on health promotion at a level sufficient to provide fruitful interaction with public healthcare systems.
As for many things in a post-COVID-19 context, technology is part of the solution [138]. However, one must keep in mind that, due to inequalities, digital technologies are not a universal solution to increase adherence to physical activity treatments. Indeed, digital inequalities affect disadvantaged populations to a greater extent, and technology should not be considered as a panacea to increase adherence to physical activity treatment in populations that do not have access to physical activity equipment at home or in the neighborhood. However, these solutions can offer powerful tools contributing to reduce the load on clinicians and on the health systems overall. One example of such an application of technology is the use of digital communication to follow up on depressed patients.
New communication technologies offer plenty of new tools and possibilities to equip both clinicians and patients trying to use physical activity. For instance, in the health and fitness category for Android devices, more than 91,000 apps, with 85,000 apps free of charge [152], are available for clinicians to recommend. As they are addressed to all individuals, and not only those who are at high risk, they could be used in a preventive or health-promotion approach rather than a treatment one. Although such apps do not systematically rely on research evidence or public-health recommendations [153, 154], literature reviews addressing app use in medicine and health promotion nonetheless show modest, but promising, results on physical activity and weight lost [155, 156]. Also, multiple devices exist to support and enhance the positive aspects of practicing physical activity, ranging from watches to various kinds of detectors [157, 158].
Finally, beside the direct use of specific applications, technology also provides new ways for patients to access information relevant to their health. The availability of online health information and its quality is, however, highly heterogeneous [159, 160]. First-line clinical institutions should contribute to the preparation and dissemination of hybrid documents — accessible online or printed for those patients having less physical or cognitive accessibility to technology — that patients could refer to subsequent to the initial consultation.
In the fight against depression, physical exercise represents an underused tool that could uniquely address several problems at the same time, as well as complement other conventional therapeutic strategies. Exercise provides many physical benefits, which can counteract several mechanisms postulated to increase mortality risk in depressed people. If prescribed and administered correctly, exercise can be as effective as other first-line treatments, while generally being free from unwanted side effects. Research demonstrated that exercise and physical activity can be used efficiently in the context either of acute or chronic depression, with or without the co-occurrence of other health issues. In this light, this review not only presented evidence supporting the use of physical activity to prevent and fight depression, but also clearly advocated for the need for primary-care physicians to complement exercise scientists and mental-health specialists to successfully tackle the symptoms and episodes of depression.
In the end, patient adhesion is central to the implementation of any change in clinical culture. If one wants patients to do something, especially when it comes to practicing physical activity, it is important to make sure that these activities are perceived as being enjoyable by the patients themselves. Health promotion will be a key to reach this point, as physical activity has very positive and cumulative effects on general health. Yet even if both clinicians and patients are aware of the benefits of physical activity, clinicians will have to take into consideration that the adoption of this behavior for the patients is not solely dependent on the person’s will. Here, the societal advocacy role of clinicians in promoting the inclusion of facilities favoring healthy lifestyles in modern urban areas will be essential.
Recent years have demonstrated how critical mental health can become. The COVID-19 pandemic has been accompanied by a clear increase in the occurrence of depression. The difficulties of accessing healthcare system during this crisis exemplify the potential that hybrid approaches, combining conventional therapeutic approaches with physical activity, could have to fight depression. Yet the COVID-19 pandemic is just the first of what might become more common in the near future, especially with the impact of climate changes on human populations. Enhancing mental health in an age where such challenges will become increasingly prominent is of critical importance. Capitalizing on physical activity to help prevent and fight depression should be considered as a path for clinicians to explore in the coming decades, as such strategies might represent important assets for public health and the well-being of the population.
CC, JW and MJG conceptualized, wrote, and edited the manuscript. CC and EB performed the literature survey, drafted and edited the manuscript. EB and MJG performed art work. All authors contributed to the article and approved the submitted version.
Not applicable.
We would like to thanks the senior management of Faculty of Medicine, University Montpellier for their constant support and encouragement. The manuscript has been checked by an independent scientific English language editing service (Stels-ol.de.).
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

