1 International Observatory in Hospital Pedagogy, Universitat de Barcelona, 08035 Barcelona, Spain
2 Department of Didactics and Educational Organization, Faculty of Education, Universitat de Barcelona, 08035 Barcelona, Spain
3 Research Group and Innovation in Designs (GRID), Technology, Multimedia, and Digital Application to Observational Designs, Thematic Core, Hospital Pedagogy, Universitat Autònoma de Barcelona, 08193 Barcelona, Spain
4 Now with Department of Psychiatry, Faculty of Medicine, The University of British Columbia, Vancouver, BC V6T 1Z4, Canada
5 Multidisciplinary Research Nursing Group, Vall d’Hebron Research Institute (VHIR), Vall d’Hebron Hospital Universitari, Vall d’Hebron Barcelona Hospital Campus, 08035 Barcelona, Spain
6 Education and Society Program, Faculty of Education, Universitat de Barcelona, 08035 Barcelona, Spain
7 Department Biomedical Sciences, Institute of Neurosciences, School of Medicine and Health Sciences, Universitat de Barcelona, 08035 Barcelona, Spain
8 August Pi i Sunyer Biomedical Research Institute (IDIBAPS), 08036 Barcelona, Spain
†These authors contributed equally.
Abstract
Scientific attention is increasingly being drawn to the emotional impact and neurodevelopmental difficulties experienced by children and adolescents with heart disease. Therefore, this article aimed to review the literature from the last decade on health-related quality of life (HR-QoL) and cognitive functions (CFs) in children and adolescents with heart disease, highlighting its implications for these populations.
This rapid systematic review and meta-analysis were conducted using the Web of Science (WoS) database. We used the Scale for the Assessment of Narrative Review Articles (SANRA) as a quality control check and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. Two meta-analyses were conducted to synthesize intelligence quotient (IQ) and QoL outcomes using data extracted from eligible studies. Random-effects models, Hedges’ G or mean differences, and I2 statistics derived from Cochran’s Q were applied to assess effect sizes and between-study heterogeneity.
A total of 133 articles were identified, and 23 were eligible. The main results suggested a relationship between the characteristics and consequences of heart disease and neurodevelopment, which influence QoL and functional areas. The meta-analysis revealed a significant decrease in total IQ in patients compared to controls. We also found that the psychosocial QoL of the patient was significantly lower than the physical QoL.
Neurodevelopment and QoL are fundamental aspects that must be addressed in a preventive manner.This review responds to the challenges faced by children and adolescents with congenital heart disease (CHD) who have undergone one or more surgical interventions, particularly regarding neurodevelopmental outcomes and executive function deficits, as examined through cohort and cross-sectional studies. However, a critical gap remains in the literature regarding longitudinal studies that evaluate the impact of short-, medium-, and long-term interventions specifically designed for this population.
Keywords
- heath
- pediatric heart disease
- quality of life
- surgery
- cognitive function
Pediatric populations with complex medical conditions (CMCs) require long hospitalization periods and re-admissions, associated with permanent disabilities, major frailty, and medical complexity [1]. Consequently, addressing a CMC directly challenges not only patients and caregivers but also siblings and family social relationships. Therefore, pediatric chronic disease conditions alter the roles and lifestyle of the whole family [2]. Children with heart disorders are one of the largest chronic pediatric populations, with high comorbidity and recurrent healthcare service contact [3]. Congenital cardiac disturbances are one of the most prevalent CMCs and the most predominant congenital disorders [4, 5].
The concept of health has evolved over the years. Indeed, public health, health determinants and promotion, well-being and quality of life (QoL), healthy habits, health literacy, psychoeducation in hospitals and health settings, and neurodevelopment must now be considered holistically. Concurrently, technological innovation and advances, such as medical devices, robotics, artificial intelligence, and bioethics, must be integrated.
In 1946, the World Health Organization (WHO) [6] defined health as a state of complete physical, mental, and social well-being, rather than the mere absence of disease. In 1976, the definition was expanded to include the condition of harmony, encompassing the functional, psychological, and psychic balance of an individual dynamically integrated into their natural and social environment: a way of living that is increasingly autonomous, supportive, and happy [7]. However, Gil-Roales [8] discussed illness responses, conceptualizing them as a form of illness behavior. Conversely, Bircher and Hanh [9] consider human health as an adaptive complex system that changes throughout life, adhering to a definition of health established by Boers and Cruz Jentoft [10], conceptualizing health as resilience, or the ability to cope, maintain, restore integrity, and balance a sense of well-being in physical, mental, and social domains. Hence, frailty was considered the weakening of health.
Various organizations focus on facilitating the right to health, such as the Pan American Health Organization (PAHO) [11]. Notably, the PAHO was the first of its kind and has been dedicated to ensuring health rights through public health policy work in the American region since 1902. The PAHO focuses on improving equity to ensure health accessibility and universal health coverage. Meanwhile, another example is the International Network of Health Promoting Hospitals and Health Services, which was established as an initiative of the WHO in 1988 to improve health by improving the quality of care (among hospitals, health services, the community, and the environment), as well as enhancing conditions and satisfaction of patients, families, and staff. The United Nations International Children’s Emergency Fund [12] implements health care projects focused on maternal, newborn, and child survival, as well as, child and adolescent health and well-being; meanwhile, the Global Health Council [13] advocates for global health awareness and legislation; Doctors of the World [14] states that healthcare is not a privilege but a human right are among a plethora of other non-profit international entities committed to global health rights; The Foundation for Global Community Health [15] promotes healthy schools for healthy children.
McPherson et al. [16] proposed the need for developing community service systems aimed at special health needs. This highlights the importance of developing programs to address the specific needs of pediatric populations with special healthcare needs, such as those in pediatric cardiology. Edwards and Goodman [17], in a review addressing the needs of children with severe chronic illness, determined various important concepts, such as complex chronic conditions described by Feudtner et al. [18] and Pinto et al. [19] as children with complex health conditions, with a symptom duration that exceeds 12 months (unless death occurs), involving different systems or only one, but severe enough to require specialized pediatric care and possibly a certain period of hospitalization in a highly specialized center [19, 20]. Therefore, including previously excluded diagnoses such as children with chronic critical illness (CCI; [21]) and severe neurological impairment (SNI); [22, 23]), or referring children and adolescents dependent on a medical device to compensate for the loss of a vital bodily function with substantial and ongoing nursing care to prevent death or further disability (technology dependent in children and adolescents) [24]. In this article, we adopt the term “visualized” from Muñoz-Violant et al. [25], who used it in the context of a CMC study examining well-being factors in childhood and adolescence versus the hospitalization experience. This concept evolved from the term “children with medical complexity”, coined by Cohen et al. [3] and followed by Berry et al. [26].
Recent studies about parental experiences of caring for children with CMC indicate that family function and changes are prevalent. Parental involvement in the care of the children is associated with improved family functioning; however, it also decreases the psychological health of caregivers, thereby increasing their own healthcare needs [27, 28]. Bowden et al. [29] revealed stress–emotional symptoms in both parents if one of them had psychological affectations, which could disrupt family roles. Moreover, pediatric illness may cause fearful caregiver feelings related to the uncertainty of the need for numerous pediatric healthcare services and an unpredictable or unknown situation. This lack of confidence is especially accentuated in situations unknown to the family, such as the diagnosis moment, instant health information, and hospital admission and discharge [30]. Parental stress and anxiety levels when children are undergoing surgery for congenital heart disease are significantly higher compared to other types of surgeries [31, 32, 33]. Recent research suggests that professionals should consider the roles, anticipation, and coping strategies of the parents, and that professional support addressing parental stress can be provided [34]. All of this should help to self-manage the high risk of the surgery on the child, but also to attenuate the risk of mental and emotional alterations following immediate and late postoperative heart surgery [28].
Heart disease, congenital or acquired, requires routine family changes, hospital-reiterated visits, strict medical management, heart surgeries, and invasive and non-invasive tests, and involves a real mortality risk [35]. Therefore, heart disease is associated with specialized care and early critical needs [36]. Disease severity and associated complications maintain a higher risk of morbidity and disability development, both during childhood and adulthood [37]. However, emotional and behavioral problems are higher in pediatric patients with heart disease than in other pediatric populations [38]. Therefore, anxiety and emotional disturbances may be an important factor in the effect of cardiovascular pediatric surgery. Conversely, cardiovascular pediatric surgery can evoke negative emotions in a new and stressful situation, although it can also be viewed as a healing and QoL improvement mechanism [34]. The perioperative period can be emotionally devastating for children and adolescents who suffer from anxiety and distress in the pediatric surgical field, which has a considerable number of invasive and non-invasive procedures [39, 40]. This phenomenon is associated with an event having an uncertain outcome and is frequently accompanied by fear or distress [39]. Therefore, importance must be given to reducing anxiety levels and increasing the control of a new medical event if we focus on pediatric cardiac surgery [41]. Recently, several studies have emphasized the importance of focusing attention on the neurodevelopmental difficulties shown in children and adolescents with heart disease. Specifically, Marino et al. [42] concluded that there is an increased risk of developmental disabilities or delays, as well as difficulties in cognitive function [43, 44, 45] and various other domains [42, 46, 47]. Brosig et al. [48] described a population presenting problems with mathematical operations, pronouncing words, spelling, handwriting, attention deficits, and difficulties with sequential instructions.
Therefore, this article aimed to review the literature from the last decade on health-related quality of life (HR-QoL) and cognitive functions (CFs) in children and adolescents with heart disease, highlighting its implications for these populations.
We reviewed the literature from the last decade regarding HR-QoL and CFs in children and adolescents with heart disease. The literature was reviewed in a search of the Web of Science Core Collection database. The scale for assessing narrative review articles (SANRA) [49] and the PRISMA checklist [50] were used as a quality control check of this review. The advanced search was conducted using the equation: (((TS=((“quality of life” OR “health-related quality of life”))) AND TS=((child* OR adolescent* OR youth OR teenager))) AND TS=((“Heart Disease”))) AND TS=((“Cognitive function” OR “Executive function”)). The articles reviewed were screened based on title, publication, population, and keywords (Table 1).
| Inclusion criteria | Exclusion criteria |
|---|---|
VOSviewer software (version 1.6.18, Leiden University, Leiden, The Netherlands) was used to construct and visualize the relationships among the most frequently occurring terms in the titles and abstracts of the selected articles. The maps generated displayed a network of nodes and links, with colors representing different clusters. The size of the nodes reflected the occurrence frequencies, while the thickness of the links between nodes indicated the co-occurrence frequencies. The analysis settings were as follows: the counting method was full counting, the minimum number of occurrences of a term was set to 5, and we selected 60% of the terms with the highest relevance score to build the maps.
This review includes two meta-analyses. The first one is focused on the studies included in the review that provided total intelligence quotient (IQ) scores collected using either different editions of the Wechsler Intelligence Scale for Children (WISC) or the Differential Abilities Scales-Second Edition (DAS-II) questionnaires. To standardize data to a common scale, we calculated Hedges’ g as an estimator of the standardized mean difference (SMD) [51] versus a normative population (100
The search was from 2015 to 2024. From the 133 identified articles, 85 were eligible after removing duplicates (48 articles). A two-stage screening process was applied, where all eligible studies were initially screened by title and abstract (31 studies were eligible). Then, the full text was reviewed (23 articles were eligible) (Fig. 1).
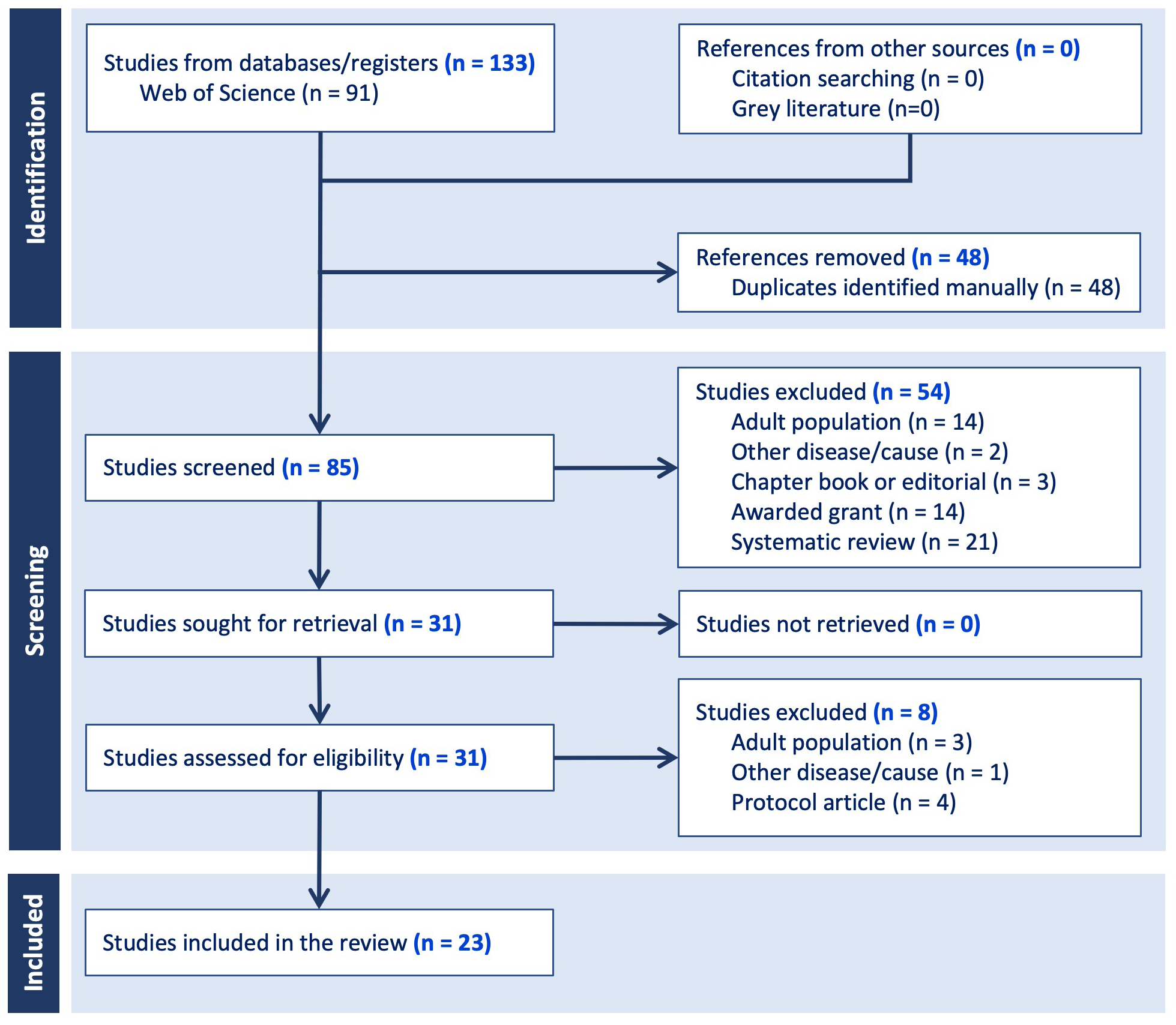 Fig. 1.
Fig. 1. Flow diagram of the study selection process.
We synthesized the principal elements of each study, including sociodemographic and medical variables, QoL and psychosocial aspects, the domains of neurodevelopmental impairments, and the main results (Table 2, Ref. [45, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74]).
| Authors | Aims | Population | Methodology | Data: | Main outcomes |
| 1. Demographic | |||||
| 2. Psychosocial and/or quality of life (QoL) | |||||
| 3. Impaired neurodevelopmental domains | |||||
| Mittnacht, 2015 [53] | To assess the effect of acute postoperative tri-iodothyronine (T3) administration after cardiac surgery in infants on their long-term cognitive performance and motor development. | 28 children were treated with tri-iodothyronine after cardiac surgery. | A prospective follow-up study that retained the original randomized, double-anonymized, placebo-controlled protocol. | 1. Sex, age, body mass index (standard deviation scores), and education (for both children and parents), as well as medical characteristics, including cardiac diagnoses. 2. Variables not considered in the study. 3. Neuropsychological functioning: intelligence quotient (IQ) (general intellectual abilities), executive functions: attention, concentration, psychomotor speed, cognitive shifting, and complex sequencing function (series of sequentially numbered and lettered circles). | The intelligence quotient for all children was located within the reference range, with no significant difference between the placebo and T3 groups. Additionally, assessments of motor and cognitive abilities, growth, as well as thyroid and cardiac functions, revealed simultaneous findings. |
| Most children, after a cardiopulmonary bypass operation, had mild–moderate impairment in executive functions. | |||||
| The gross and fine motor skills were not significantly different between groups. | |||||
| Neal, 2015 [45] | To assess the health-related quality of life (HR-QoL) of adolescents with repaired Tetralogy of Fallot (TOF) and whether impairments in HR-QoL domains are associated with neurocognitive and medical factors. | 85 parents of children and children/adolescents with TOF and healthy referents/teachers (13–16 years). | Cross-sectional study, associated and correlation variables. | 1. Age, sex, race/ethnicity, medical characteristics: birth weight, gestational age, diagnosis of pulmonary atresia, age at initial operation, first operation was an open-heart procedure, deep hypothermic circulatory arrest and total support durations at first operation, number of operative complications at first operation, number of operations, open operations, operative complications, catheterizations, catheterization complications, and neurological event. | Subjects with TOF with genenic diagnosis had significantly lower PsS scores than the control sample. Subjects with TOF without a genetic diagnosis had significantly lower PsS and PhS scores than the healthy local referent group. Adolescents with TOF had worse psychosocial and physical health status than the healthy referents, and this was strongly associated with poorer executive function and attention deficit–hyperactivity disorder. Lower PhS scores were associated with worse executive function and lower full-scale IQ. |
| 2. Psychosocial functioning (PsS): mental health, role/social-emotional/behavioral, behavior, and self-esteem, bodily pain, and physical functioning (PhS): physical functioning, role/social–physical, bodily pain, and general health perceptions. QoL variable considered indirectly in the study. | |||||
| 3. IQ: global IQ, neurocognitive testing, verbal comprehension, reading, math, perceptual reasoning, memory, visual-perceptual skills (non-motor), executive function: working memory, processing speed, and autism spectrum. | |||||
| Gerstle, 2016 [54] | To investigate the presence and severity of real-world impairments in executive functioning responsible for children’s regulatory skills (metacognition, behavioral regulation) and its potential impact on school performance among pediatric survivors of complex congenital heart disease (CHD). | 143 survivors of complex children with heart disease (8–16 years) and their parents/guardians. | Cross-sectional study; associated variables. | 1. Age, sex, race (recoded as White/non-White), and yearly family income, as well as the number of school days missed for any reason. 2. Behavioral regulation: ability to shift mindset and regulate and control emotions and behavior, and school QoL. 3. IQ, school competency, and metacognitive aspects of executive functioning, including working memory, initiating, planning, and organizing tasks, as well as monitoring performance. | Survivors with single-ventricle lesions had lower school competency and QoL compared to survivors with two-ventricle lesions; survivors with two-ventricle lesions had poorer behavioral regulation than those with single-ventricle lesions. |
| Executive functioning, intelligence quotient, school competency, and school-related quality of life results were worse in survivors of complex CHD than for the normative sample; metacognition was more severely affected than behavior regulation. Age correlated with poor metacognition but not behavioral regulation; metacognitive deficits were more often present in older children. | |||||
| Latal, 2016 [55] | To provide information about neurodevelopmental problems for parents with CHD children. | Children with congenital heart disease. | Theoretical article. | 1. Age, genetic comorbidity, clinical examination, electrocardiogram, neuroimaging | Noncardiac comorbidities and complications significantly impact long-term QoL and educational performance in children born with congenital heart defects. Impairments may occur in conjunction and significantly affect school performance, integration, and academic achievement. A considerable number of children with CHD show neurodevelopmental deficits, impacting thinking, movement, and language growth, as well as advanced cognitive functions. |
| 2. Behavioral problems: externalizing symptoms: hyperactivity, impulsivity, internalizing problems: depression or emotional problems. QoL variable considered indirectly in the study. | |||||
| 3. Neurodevelopmental: executive functions, cognitive functions (inhibitory, interference control, working memory, cognitive flexibility), verbal fluency (home, school: personal autonomy, independence, planning responsibilities). | |||||
| Laraja, 2017 [56] | To characterize neurodevelopmental outcomes after fetal aortic valvuloplasty for evolving hypoplastic left heart syndrome and determine the risk factors for adverse neurodevelopment. | 69 children and adolescents (5–18 years) with congenital heart disease. | Cohort study with cross-sectional measurement and with retrospective review; multivariable analysis. | 1. Age, sex, medical characteristics: birth characteristics, family socioeconomic status (SES), nutrition, previous Interventions, fetal cardiac intervention, cardiac surgeries, cardiac catheterizations. 2. HR-QoL: physical, emotional, social, and school functioning; adaptive functioning, conceptual, social, and practical; externalizing problems; internalizing problems; behavioral symptoms; adaptive skills; behavior regulation; problem-solving; personal social skills. 3. Global executive, cognitive, metacognition, communication, and language: verbal, non-verbal, motor: gross and fine motor development. | Children who underwent fetal cardiac intervention (FCI) had significant impairment in general adaptive functioning (difficulties to age-appropriate self-care skills and independence). When compared to healthy norms, the FCI cohort showed significantly lower mean scores in both the psychosocial and physical QoL domains. |
| The general adaptative composite mean score was lower than population norms. Children with fetal aortic valvuloplasty had a neurodevelopmental delay, similar to patients with hypoplastic left heart syndrome without fetal intervention. For all other neurodevelopmental questionnaires (BASC-II, BRIEF, ASQ-3, pedsQL), most subscale scores for patients with biventricular and single ventricle circulation were similar. | |||||
| Singh, 2018 [57] | To examine regional brain gray matter changes, using high-resolution T1-weighted images (3.0-T magnetic resonance scanner) with voxel-based morphometry procedures, as well as mood and cognitive functions in adolescents with single ventricle heart disease. | 49 adolescents with single ventricle heart disease (n = 18), without/healthy controls (n = 31); (14–18 years). | Associated and correlation variables. | 1. Age, gender, body mass index, handedness, ethnicity, magnetic resonance imaging. 2. Depression and anxiety. QoL variable considered indirectly in the study. 3. Cognitive functions: attention, concentration, executive functions, language, memory, visuo-constructional skills, conceptual thinking, calculations, orientation, memory: verbal and visual memory, attention/concentration, working memory, and visual and verbal recognition, story memory, verbal learning, design memory, picture memory, short-term memory of a visual sequential pattern, numbers/letters memory. | Adolescents with single ventricle heart disease showed significantly higher PHQ-9 and BAI scores than the control subjects. |
| There was a decreased grey matter density in multiple brain regions related to autonomic, mood, and cognitive functions. | |||||
| Several brain regions that are associated with cognitive functions showed decreased grey matter density in single ventricle heart disease adolescents. | |||||
| Farr, 2018 [58] | To examine how cognitive and motor limitations in children with heart disease are associated with education and participation in extracurricular activities. | 29,801 children and adolescents with special health care needs and heart disease (CSHCN) (n = 1416) and without (n = 28,385); (6–17 years). | Cross-sectional study; associated variables and comparison and regression analyses. | 1. Age, functional limitations, age, medical characteristics: diagnosed with a heart problem. 2. Emotional or behavioral problem in need of counseling or treatment. QoL variable considered indirectly in the study. 3. Developmental learning/concentration, communication, self-care, gross motor skills, and fine motor skills may require physical, occupational, or speech therapy. | Heart disease was associated with the lowest participation in extracurricular activities and education in all age groups. |
| CSHCN with CHD experienced greater functional limitations and educational difficulties compared to CSHCN without CHD. | |||||
| These limitations are associated with the five functional areas (learning/concentration, communication, self-care, gross motor skills, and fine motor skills). | |||||
| Those aged 14–17 years had more limitations than other age groups. | |||||
| Jackson, 2018 [59] | To examine the role of coping in accounting for the association between self-reported executive function problems and internalizing symptoms among AEAs, as well as YAs with CHD. | 172 outpatient cardiology pediatric and adult (15–25, n = 74, and 26–39, n = 98, respectively). | Associated and comparison variables. | 1. Age, sex, medical conditions: healthy, premature, neonatal hypoxic-ischemic encephalopathy, and congenital heart disease. 2. Internalizing symptoms and coping. QoL variable considered indirectly in the study. 3. General intelligence and neuropsychological domains: language, attention, memory, executive functions, and social skills. | Coping was not associated with executive function problems or internalizing symptoms for AEAs. |
| Reduced use of adaptive coping strategies and higher maladaptive coping responses were associated with both increased executive function problems and internalizing symptoms (young adults: YAs). An indirect effect of executive function problems on internalizing symptoms via secondary control coping emerged for YAs. | |||||
| Robson, 2019 [60] | To examine associations between measurements of neurodevelopment and psychosocial health status at age 8 and 16 years in patients with repaired dextro-transposition of the great arteries. | 137 patients with repaired dextro-transposition of the great arteries Boston Circulatory Arrest study at 8 and 16 years. | 1. Age, sex, social class, and medical characteristics, including medical history variables and physical health. 2. Psychosocial health, social intelligence. QoL variable considered indirectly in the study. 3. Neurodevelopment function: IQ (verbal fluency, math achievement, listening, comprehension, executive function), memory, visual perceptual skills, attention. | Adolescents with repaired dextro-transposition of the great arteries, at 16 years old, had parent-reported psychosocial and physical health status worse than that of a local referent group. | |
| Worse psychosocial health status in adolescents with CHD was predicted by deficits in attention during elementary school. | |||||
| Attention deficits at age 8 were highly predictive of worse psychosocial health in adolescence. | |||||
| Scores were significantly worse, compared with those of the local referent group, on subscale measures of emotional well-being, behavioral problems, general health, and parental impact. | |||||
| Sanz, 2018 [61] | To test a model to predict psychosocial QoL in children with CHD via executive dysfunction. | Parents of 91 children with CHD. | Associated and comparison variables. | 1. Age, gender, medical characteristic: diagnosis and classifications of the sample (single ventricle, aortic obstruction, neurologic abnormality). 2. QoL: physical, emotional functioning, social, and school functioning; behavior regulation index: inhibit, shift, and emotional control. 3. General executive composite, metacognitive index: initiate, working memory, planning/organization, organization of materials, and monitoring. | The presence of CHD indirectly impacts psychosocial QoL at school age by being associated with increased executive dysfunction. |
| Children with CHD needing surgery within their first year, executive dysfunction strongly predicts psychosocial quality of life during school age. Neurologic abnormalities and single-ventricle CHD did not significantly predict executive dysfunction or QoL. | |||||
| Medical/demographic risk factors indirectly influenced psychosocial QoL by executive dysfunction characteristics. | |||||
| Ilardi, 2020 [62] | To provide an expanded set of neurodevelopmental evaluation strategies and considerations for professionals working with school-age children with CHD. | Children and adolescents (5–18 years) with congenital heart disease. | Theoretical article. | 1. Age, medical risk factors. 2. Clinical interview with the family, including emotional and behavioral, adaptive, and social aspects. QoL variable considered indirectly in the study. 3. Neurodevelopmental evaluation: intellectual functioning, language, memory, attention, executive function, inhibitory control, working memory, cognitive flexibility (shifting), speed of processing, academic skills, and motor skills. | It is essential to consider the referral process, the initial family interview, access to evaluation, and medical risk factors. |
| The neurodevelopmental evaluation should consider both family and patient factors. It includes the child/family’s primary language, cultural factors, as well as critical stages in development; a table is proposed for evaluating domains and tests for each age group. | |||||
| Svensson, 2020 [63] | To comprehensively describe their HR-QoL and to assess the agreement in this regard between children and parents. | 97 children with various diagnoses concerning right ventricular outflow tract anomalies and parents (8–18 years). | Cross-sectional study with a descriptive design and associated variables. | 1. Age, medical characteristics: number of catheterizations, age at first surgery, age of last surgery, type of cardiac defect. 2. QoL: physical, emotional, social, and school functioning, psychosocial, heart problems, physical appearance, and treatment anxiety. 3. Cognitive problems and communication. | More than 20% of the patients reported problems regarding limited physical capacity and cognitive function; nearly half of the children reported problems with breathlessness when participating in sports, and a quarter reported cognitive and communication problems when people saw their scars. |
| Ten percent of children considered that their heart disease caused them “different kinds of troubles or hard feelings”. | |||||
| Tester, 2021 [64] | To assess executive and socio-emotional/behavioral functioning in pediatric supraventricular tachycardia patients. | 30 children and adolescents (7–17 ages) with supraventricular tachycardia (SVT) who had not undergone catheter ablation. | Descriptive analysis. | 1. Age, education plan, extra school assistance, medical characteristics: supraventricular tachycardia burden history and treatment history, medication, intensive acute and/or chronic therapy. | They have an elevated risk of developing internalizing problems compared to the general population. However, for this population, the behavioral monitoring scale showed improved performance. |
| 2. Behavioral regulation, inhibition, shift, emotional control, affective problems, anxiety, withdrawal/depression, somatic complaints, social problems, thought problems, rule-breaking, aggressive, internalizing problems, externalizing, oppositional defiant problems, and conduct problems. QoL variable considered indirectly in the study. | The development of psychological morbidities in the pediatric population who experience SVT may be affected by anxiety and avoidant behavior. | ||||
| 3. Executive functioning and metacognition: global executive composite, initiate, working memory, plan/organize, organization of materials, monitor, and attention-deficit–hyperactivity problems. | |||||
| Wotherspoon, 2020 [65] | To assess outcomes in adolescence after surgery for CHD in infancy. | 21 adolescents (14–17 years) with CHD. | Associated and comparison variables. | 1. Sex, medical characteristics: diagnosis, gestational age, birth weight, age at repair, congenital abnormalities, total number of cardiac surgeries, bypass time. 2. HR-QoL, adaptive behavior, behavior, social and emotional well-being. 3. IQ: cognitive ability; memory, attention, and executive function: verbal comprehension, perceptual reasoning, working memory, processing and learning (academic achievement), visual perception, visual construction, and motor abilities. | Adolescents reported significantly decreased HR-QoL compared to the healthy adolescent population. |
| The cognitive ability of the participants was lower than that of the general population, without significant differences. | |||||
| Participants displayed difficulties in cognitive functioning, academic achievement, attention, organization, emotional and behavioral functioning, and HR-QoL. However, no significant difference in social functioning was reported. | |||||
| Gaudet, 2021 [66] | (1) To characterize the neuropsychological outcome of children with CHD. (2) To identify early neurodevelopmental markers of neuropsychological outcomes in these children. | 55 children with congenital heart disease (at 5 years). | Cohort study. | 1. Sex, maternal education, family income, perinatal characteristics, surgical characteristics. | Five-year-old children with congenital heart disease had significantly poorer performance and an increased prevalence of impairments than the normative sample. Immediate and sustained attention, as well as working memory, among other higher-order cognitive domains, were the most affected. |
| 2. Variables not considered in the study. | |||||
| 3. Intelligence, receptive language, expressive language, global language, phonological awareness, pre-mathematics, concentration, executive function: numbers forward and backward. | |||||
| Spillmann, 2023 [67] | (1) To describe the IQ and executive function profile, the type and level of education and educational support, and the participation in leisure activities in a contemporary cohort of children with CHD who underwent CPB. (2) To investigate whether cognitive deficits are associated with education and participation. | 134 children with CHD who underwent CPB (10 years). | Prospective cohort (2004–2009); associated variables. | 1. Age, sex, socioeconomic status, race, medical characteristics: prenatal diagnostic, gestational age, weight, head circumference, length, cardiac class, cyanotic heart defect, univentricular heart defect, and pre-, intra-, and postoperative characteristics. 2. Type and level of education, educational support, and participation in leisure activities. QoL variable considered indirectly in the study. 3. IQ (perceptual reasoning, processing speed, verbal comprehension, working memory) and executive functions (global executive function, metacognition, behavior regulation). | The vast majority of the children with CHD attended regular school but less than the general population. Some CHD children needed extra educational support, including more time enrolled in the school. It is associated with a lower IQ and impaired executive functions. Sports and music, or other leisure activities, were less engaged to children with CHD than norms. It was associated with lower IQ. Metacognitive abilities, processing speed, IQ values, and working memory were all below the corresponding norms. |
| Cainelli, 2022 [68] | To analyze the impact of early insults from an evolutionary perspective by performing unsupervised cluster analysis. | 114 children with different adverse medical conditions: healthy (n = 30), premature (n = 28), neonatal hypoxic-ischemic encephalopathy (n = 28), and congenital heart disease (n = 28) (5–10 years). | Associated and comparison variables - unsupervised, nonparametric, and very conservative clustering analysis. | 1. Age, sex, medical conditions: healthy, premature, neonatal hypoxic-ischemic encephalopathy, and congenital heart disease. 2. Variables not considered in the study. 3. General intelligence and neuropsychological domains: language, attention, memory, executive functions, and social skills. | Three emerging clusters were identified: children with adequate profiles and good performance in IQ and executive function tests (cluster 1), children with neuropsychological profiles that were variable but in the average normal range (cluster 2), and children with multiple impairments (cluster 3). The clusters did not differ by medical status, with the exception of the pathological group, which comprised only one healthy child. |
| Semantic fluency, auditory attention, visual memory for neuropsychology and thought problems, anxiety/ depression, aggressive behavior, and attention problems for the symptoms of psychopathology were the greatest differences variables. | |||||
| The causative mechanisms for adverse neuropsychological outcomes are multifactorial, interrelated, cumulative, and likely synergistic over time. | |||||
| Jassal, 2023 [69] | (1) To describe attention and executive function in youth with Fontan population, measured via standardized performance-based tests and caregiver rating scales. (2) To examine how weaknesses in attention and EF were related to outcomes in other neurobehavioral domains, including adaptive behavior and academic achievement. | 93 children and adolescents with a history of Fontan underwent a clinical neuropsychological evaluation (5–18 years). | Retrospective chart review (2011–2022). | 1. Age, sex, race, ethnicity, medical characteristics: cardiac diagnosis, and available neuroimaging. | Adaptive behavior, inattention, anxiety, hyperactivity, and depression were higher compared to normative means (caregiver-reported). No differences in academic or adaptive skills by type of single ventricle physiology. Domains of attention, executive functions, academic achievement, and intellectual ability were lower than normative means. Academic outcomes were differentially affected by demographic and attention or executive functioning variables. |
| 2. Behavioral/emotional diagnoses, anxiety and depression, neurological comorbidities, attention-deficit–hyperactivity disorder, autism. QoL variable considered indirectly in the study. | |||||
| 3. IQ: general ability index, intelligence scale, neuropsychological information: word reading, numerical operations, and spelling. Performance-based attention and executive function: working memory, processing speed, categorical and phonemic verbal fluency. | |||||
| Sahel, 2023 [70] | To investigate whether alterations in connectivity between the prefrontal and cerebellar brain structures exist between CHD and control cohorts and if these alterations could predict cognitive or motor impairment among youths with CHD. | 126 children and adolescents (53 with congenital heart disease and 73 healthy controls). | Exploratory probabilistic analysis. | 1. Age, maternal education, mean household income. 2. Variables not considered in the study. 3. Cognition and motor loop: crystallized cognition composite, fluid cognition composite, dimensional card change sort, flanker inhibitory control and attention, picture sequence memory, oral reading, picture vocabulary, pattern comparison, and dexterity. | Compared to controls in similar social settings, the CHD patient cohort showed lower cognitive performance in working and episodic memory, language, and executive function. |
| . | In the CHD group, fractional anisotropy (FA) was increased in the cognitive loop connectivity pathways compared with the healthy control group. However, there were no differences in motor loop connectivity pathways between the CHD patient cohort and the controls. Selective alteration of the cerebellum–cerebral connectivity circuitry within the cognitive loops predicts cognitive dysfunction in CHD youths. | ||||
| Zampi, 2023 [71] | To evaluate and compare baseline patient characteristics, including neurocognitive function and HR-QoL in patients with complex CHD who required cardiac surgery as infants and underwent surgical or transcatheter re-intervention on the pulmonary outflow tract. | 68 with severe congenital heart disease referred for surgical or transcatheter pulmonary valve replacement were enrolled (open-heart operation) (13–30 years). | Prospective longitudinal multi-institutional study. | 1. Age, sex, weight, body mass index, level of education, medical history (including cardiac diagnosis, prior cardiac operations with cardiopulmonary bypass, and prior cardiac catheterization procedures), heart problems, and treatment score. | HR-QoL was lower compared to normative sample data (healthy patients); QoL (all) was significantly lower across all domains compared to a healthy pediatric population. More than 31% had clinically meaningful deficits in at least one of the behavior rating inventory of executive function scales (used to assess executive function). Surgical and transcatheter patients did not differ in executive function measures and HR-QoL results. |
| 2. QoL: physical, psychosocial, emotional, social, and school functioning, behavioral regulatory, depression symptoms, treatment anxiety. | |||||
| 3. Neurocognition: global executive function, metacognition, cognitive problems, and communication. | |||||
| Dardas, 2024 [72] | To investigate how CHD characteristics and interventions affect cognitive and verbal skills in Arab children while also uncovering previously unexplored connections between these skills and the QoL scores as perceived by children and parents. | 62 children with congenital heart disease (6–16 years). | Cross-sectional study; associated variables. | 1. Age, sex, primary diagnosis, cyanosis experience, disease severity, defect status, number of operations, type of intervention, and admission to Neonatology Intensive Care Unit (NICU) status. 2. Pediatric QoL (physical functioning and psychosocial functioning). 3. Cognitive ability, abstract reasoning, and problem-solving abilities. | Parental-reported child QoL scores are notably stronger than those reported by children. |
| Cognitive scores were not significantly influenced by congenital heart disease defect status or related disease characteristics, such as disease severity, cyanosis, or types of interventions, neither for sex nor conducted operations. | |||||
| A significant positive correlation between verbal skills and QoL reported by parents highlights the importance of effective communication in assessing a child’s overall well-being. | |||||
| Pimenta, 2024 [73] | To investigate the cognitive profile of patients with one typically approximate to a 3 Mb 22q11.2 deletion, considering intellectual, adaptive, and neuropsychological functioning. | 25 patients with 22q11.2DS (7–32 years). | Descriptive and associated analysis and exploratory linear regression models. | 1. Age, years caretaker of years of schooling, gender, type of school, language delay, specialized support, familial social class, medical characteristics: pregnancy problems, birth problems, poor health conditions, heart defects, use of psychotropic medications, de novo deletion. 2. Behavioral, communication, daily living skills, socialization: adaptive behavior composite. QoL variable considered indirectly in the study. 3. IQ: intellectual, performance IQ, verbal IQ, neuropsychological functioning: attentional functioning, omissions, perseverations, visuoconstructive skills, visual short-term memory, verbal episodic memory, verbal comprehension, recognition, executive function: inhibition, flexibility, perceptual organization, working memory, processing speed. | The communication index showed deficits, and participants were able to fluctuate their attention when activities demanded a higher ability to resist distraction and control automatic responses. |
| The neuropsychological profile of the sample was characterized | |||||
| by extensive deficits in attentional functioning, including a distracted and impulsive behavioral profile and difficulties in sustaining attention and vigilance. | |||||
| Communication, executive functions, attention, and visuoconstructive skills were the most impaired. | |||||
| Family income, educational level of the main caretaker, and access to quality education were significantly associated with intelligence quotient. | |||||
| Age at diagnosis and language delay were associated with outcomes in adaptive behavior. | |||||
| Roy, 2024 [74] | To investigate the impact of congenital heart disease on functional brain network connectivity and cognitive function. | 125 children and adolescents with CHD (n = 77) and without (n = 48). | Graph theory metrics, resting-state functional magnetic resonance imaging (fMRI) data, network metrics, weighted networks, and binarized networks, as well as regression models. | 1. Age, sex, medical characteristics: presence of congenital heart disease, regional network metric, health toolbox. | Results reveal variations in network connectivity patterns, especially in temporal, occipital, and subcortical areas, in both weighted and binarized networks. Interactions between CHD and regional network metrics demonstrated impacts on cognitive function, highlighting potential compensatory mechanisms. |
| 2. Variables not considered in the study. | |||||
| 3. IQ: digit span test, executive function: inhibitory, control, attention and shift, and network connectivity: fluid composite score and crystalized composite score. |
BASC-II, Behavior Assessment System for Children second edition; BRIEF, Behavior Rating Inventory of Executive Function; ASQ-3, Ages & States Questionnaires; PedsQL, Pediatric Quality of Life Inventory; PHQ-9, Patient Health Questionnaire-9; BAI, Beck Anxiety Inventory.
The 23 reviewed articles examine QoL and psychosocial aspects, as well as domains of neurodevelopmental impairments, involving children and adolescents with heart disease. Collectively, these studies analyze, compare, and establish associations between sex/gender, race, and medical characteristics, including the type of cardiopathy and variables related to surgical intervention.
A significant number of the included studies (65.21%) analyzed this population in relation to different types of heart diseases [54, 59, 63, 69, 73] or about different types and/or numbers of surgical interventions [53, 56, 60, 61, 64, 65, 66, 67, 71, 72]. Few studies included a control group of children without heart disease [45, 57, 58, 70, 74]; however, Cainelli et al. [68] included other pediatric medical conditions. Meanwhile, two studies were theoretical/reports [55, 62]. It is important to note that some studies include adults or young adults in their sample [59, 71, 73]. Additionally, some authors present results on the use of psychometric tests and neuroimaging [55, 57, 70, 74].
In some articles, parents or legal guardians played a significant role in detecting and assessing the situations and QoL of the children and adolescents. For example, Wotherspoon et al. [65] indicated that adolescents with congenital heart disease (CHD) had better family relations than the standardized sample. Nine articles evaluated the QoL or the situation from the point of view of the parents for the daughters and sons [45, 54, 58, 60, 63, 65, 69, 72, 73]. According to Svensson et al. [63], this assessment demonstrated strong agreement in the physical, social, and school function domains of the PedsQL 4.0 test, as well as a large correlation in all domains.
Seven of the selected articles contained several direct references to QoL [54, 56, 61, 63, 65, 71, 72], whereas 11 articles mentioned QoL indirectly [45, 55, 57, 58, 59, 60, 62, 64, 67, 69, 73]. Some authors analyzed the relationship between QoL and cognitive functions, including verbal skills. Dardas et al. [72] revealed different results depending on the evaluation scale. On the one hand, a positive correlation between IQ and QoL was found between Wechsler’s scores and parent-reported QoL scores, especially in the social and educational dimensions, but not in Raven’s scores.
Spillmann et al. [67] described the education and leisure activities situation of children with congenital heart disease, focusing on children who underwent cardiopulmonary bypass surgery. Spillmann et al. [67] determined that educational support, including additional years of schooling, grade retention, transition/introductory classes, and extra tutoring, was necessary for 26.4% of the children with CHD who received education in regular schools. Leisure activities were defined as sports (72%), musical activities (46%), and other social activities (20.8%). Finally, Spillmann et al. [67] concluded that lower IQ and less participation in leisure activities were associated. In line with this, Gerstle et al. [54] found that survivors with single-ventricle lesions had significantly lower school QoL compared with those with two-ventricle lesions. Moreover, Gerstle et al. [54] found that metacognition was the strongest predictor of school-related problems, compared to IQ and sociodemographic variables.
Finally, some studies assessed depression and/or anxiety variables [55, 57, 63, 64, 69]. Adolescents with single ventricle heart disease had higher anxiety scores than the control subjects [57], and caregivers reported elevated scores in children and adolescents for depression and anxiety if these individuals had a history of Fontan disease [69]. Somewhat similarly, Tester et al. [64] affirmed that anxiety and avoidant behavior could be related to psychological mobilities in supraventricular tachycardia (SVT) experience in a pediatric sample. Otherwise, Latal [55] analyzed the behavioral problems and concluded that clinical assessment could be necessary with the most complex CHD.
Jackson et al. [59] explained the relationship between executive problems and internalizing symptoms with primary, secondary, and disengagement control coping. The sample included adolescents and emerging adults (AEAs), as well as young adults (YAs). However, Jackson et al. [59] did not find a relationship between the AEA results and coping; meanwhile, the authors suggested that low coping strategies in YAs were associated with more executive function problems and internalizing symptoms. According to Sanz et al. [61], executive dysfunction, defined as weaknesses in cognitive processes, was a strong predictor of childhood psychosocial QoL. This was especially important to CHD children with injury or related factors that could affect brain maturation. Additionally, Farr et al. [58] conducted a cross-sectional study with a sample of 1416 children and adolescents with special healthcare needs and heart disease (CSHCN), comparing their functional limitations and educational difficulties with those in a standardized group.
The results were heterogeneous in the use of different tests to assess the cognitive and metacognitive elements that influence neurodevelopment (Table 2). Therefore, an effort was made to maintain the various concepts used by the authors in this classification. Overall, the findings can be grouped into three main categories: (1) IQ, (2) executive functions and metacognition, and (3) academic performance (as a consequence of the development of the previous two categories). The most relevant results for each group are presented in Table 2.
We presented two types of results. On the one hand, we presented the bibliometric analysis using VOSviewer. After applying the term-selection criteria, the initial number of 894 terms in the titles and abstracts of the 23 selected articles was reduced to 36 items in the network map. For instance, terms such as “score”, “heart disease”, “quality”, and “life” represent the most used terms, with more than 25 occurrences each (Fig. 2A). The analysis also revealed a map of 276 links and five main clusters. One of the clusters had the term score as the most common, and the terms “adolescent” and “neurodevelopment” also presented high occurrences. This cluster also presented many strong links within terms (Fig. 2B). A central cluster, with heart disease as the main term, showed a high number of links with terms in the other clusters (Fig. 2C). These included terms related to adolescence, attention, and executive functions, as well as QoL. A third cluster with 11 terms exhibited a more dispersed structure with attention as the most occurrent term and risk as the central term (Fig. 2D). The fourth cluster had quality and life as the main terms (Fig. 2E) and was strongly connected with the fifth small cluster that presented the terms executive function and QoL as the only terms.
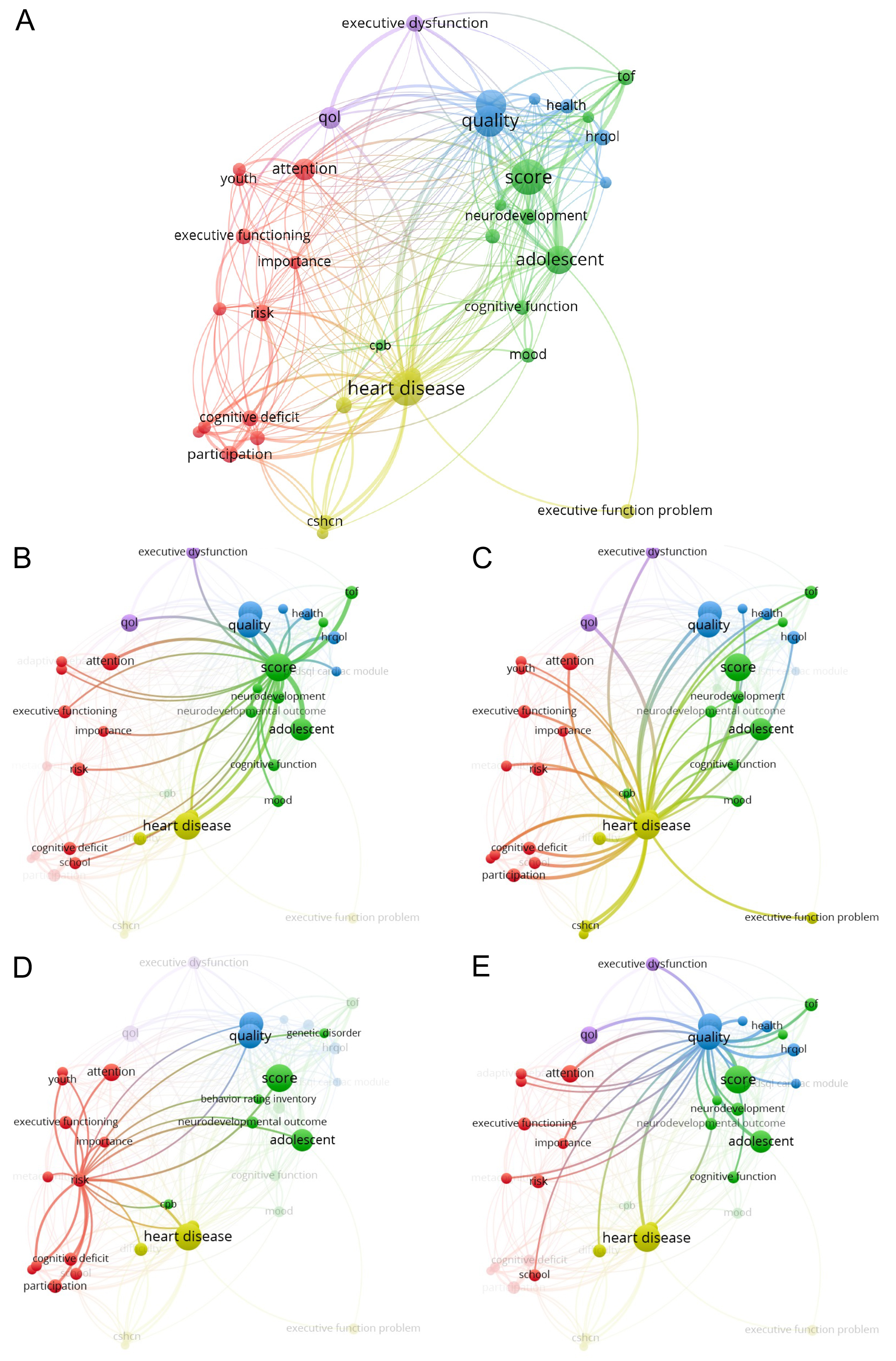 Fig. 2.
Fig. 2. Network maps of term co-occurrences in the selected articles. (A) Network map of terms in the title and abstract; nodes and links of every cluster of terms are represented in different colors. Details of clusters: score (B), heart disease (C), attention (D), quality (E). CSHCN, children and adolescents with special healthcare needs and heart disease; HRQOL, health-related quality of life; QOL, quality of life.
Alternatively, we performed a meta-analysis of the effects of CHD on the total IQ of each patient. Nine articles reported data regarding the total IQ of patients using the WISC (8 studies) or the DAS-II (1 study) questionnaires. The combined sample size was 689, and we found a significant total IQ decrease in patients (SMD = –0.38, 95% CI [–0.51; –0.25], t = –6.71, p = 0.0002; Fig. 3). We observed moderate heterogeneity (I2 = 42.3%, p = 0.0855) in the random effects model. Meanwhile, the sensitivity analysis showed that SMD remains stable when removing any study from the model (z = –6.71; p
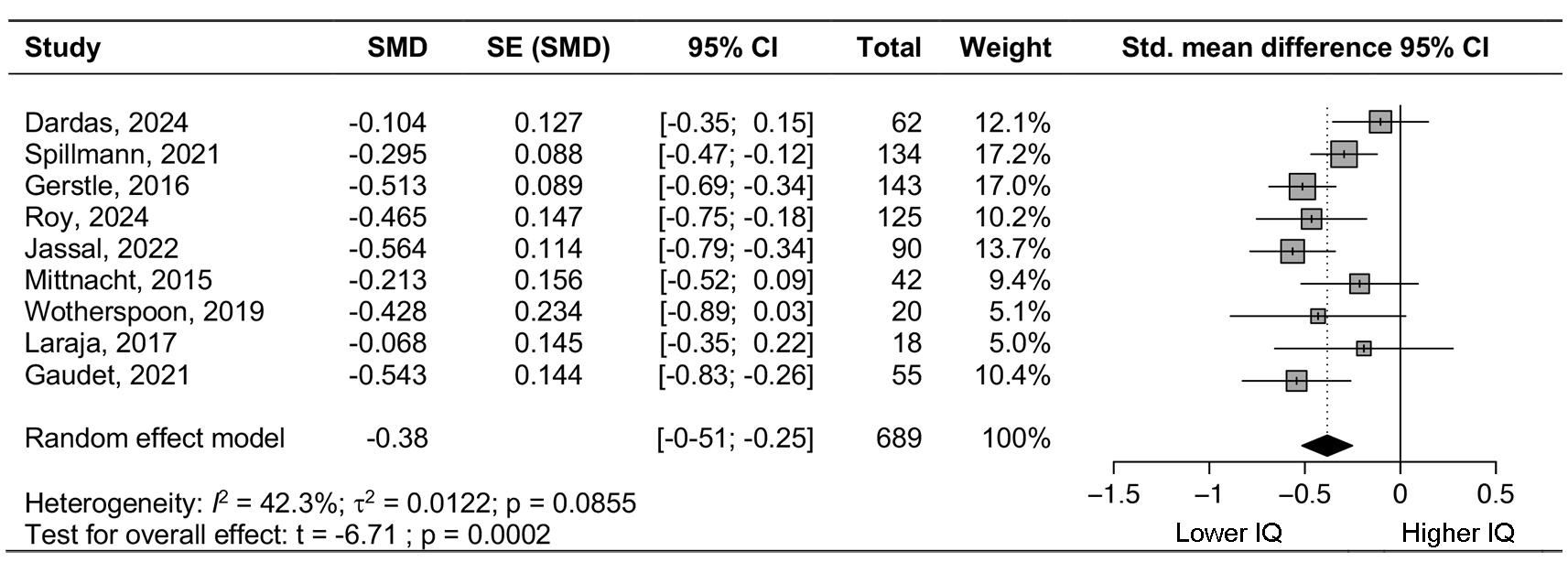 Fig. 3.
Fig. 3. Forest plot total IQ. IQ, intelligence quotient; SMD, standardized mean difference; CI, confidence interval; SE, standard error.
The second meta-analysis evaluated the QoL of the patients. Only four articles reported complete data regarding the QoL assessment. We found that the combined sample size was 220 for both the physical and psychosocial QoL dimensions of the questionnaire, and the combined effect was not statistically significant, although a tendency could be inferred (mean difference [MD] = 4.57, 95% CI [–0.71; 9.86], z = 1.69, p = 0.0904; Fig. 4). The small diamond-shaped square falls to the right of the null line, which implies that the physical QoL is higher than the psychosocial one. Moderate heterogeneity was observed in this study (I2 = 53.3%, p = 0.0926), as determined by a random-effects model. This heterogeneity was primarily based on the article by Zampi et al. [71], whose study is the only one to provide physical QoL values lower than those of the psychosocial QoL. Thus, after removing this study in the sensitivity analysis, the combined effect of the remaining studies was statistically significant (MD = 6.49; 95% CI [2.47; 10.51]; z = 3.16; p = 0.0016; Supplementary Figs. 3,4), and the study observed very low heterogeneity (I2
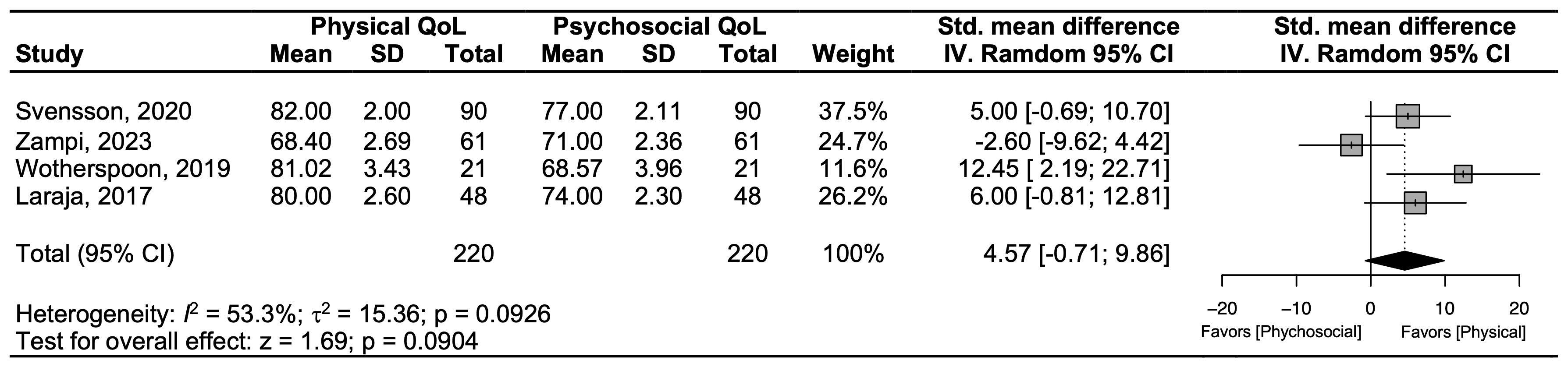 Fig. 4.
Fig. 4. Forest plot of physical and psychosocial quality of life values. QoL, quality of life; SD, standard deviation; IV, inverse variance.
This article aimed to review the literature on HR-QoL and CFs in children and adolescents with heart disease, highlighting the implications. This review emphasizes the importance of assessing and addressing the neurodevelopmental needs of children and adolescents with CHD, aligning with the guidelines of the American Heart Association and the American Academy of Pediatrics [42]. Meanwhile, emerging interventions [75, 76] and executive function assessment protocols [43, 77] continue to highlight that executive function impairments are among the most prevalent neurodevelopmental morbidities in this population. These results align with numerous studies in the field that document these same phenomena [61, 78].
Children with heart disease report higher levels of depressive and anxiety symptomatology than their healthy counterparts, particularly during periods of hospitalization [79]. Therefore, addressing this aspect as poor mental health, which has detrimental effects on both the short- and long-term physical and psychological health and QoL of this population, is of paramount importance [80]. Progress in personalized multidisciplinary medical interventions has substantially enhanced the survival rate and QoL of the pediatric population with CMC, especially those with cardiopathy/heart disease. However, psychological interventions for this population are limited; nonetheless, these remain crucial to the well-being of the child and involve patient rights and shared duties and responsibilities of the healthcare systems [81]. Intervention programs focused on psychological support and suitable information should be implemented, programs that not only impact the care that parents should provide to their children, but also enhance self-care in children and adolescents.
Numerous studies have explored the outcomes of these children from the perspectives of the parents. However, limited research exists comparing these perspectives with those reported by the children. Muñoz-Violant et al. [25] found that the perception of disease in youth with complex health conditions, including CHD, was significantly lower than that detected in caregivers. This is important as the perceptions of parents toward their children may act as a self-fulfilling prophecy.
The meta-analysis revealed substantial variability in the presentation and analysis of cognitive function data in children with CHD. This heterogeneity precluded a meta-analysis that would enable direct comparisons of cognitive function between children with CHD and the general population, as well as assessments of correlations with cardiomyopathy severity or socioeconomic status. However, further analysis showed that all included studies reported similar outcomes, with none contributing disproportionately to heterogeneity or displaying significant bias. We examined the potential influence of age and the type of cognitive assessment used (WISC or DAS-II), but neither factor had a significant effect on the results. This suggests that the moderate heterogeneity observed in the study (42.3%; p = 0.0855—borderline significance) is likely related to differences in the severity or type of heart disease or variations in patient cultural and socioeconomic backgrounds.
Four studies were identified that reported comparable HR-QoL data using the same measurement instrument. Based on these studies, our meta-analysis compared physical and psychosocial QoL assessments in children with CHD. The results demonstrated a consistent trend toward higher physical QoL relative to psychosocial QoL. Nevertheless, statistical significance was not reached due to data heterogeneity, primarily driven by the Zampi et al. study [71]. This study focused on patients with severe CHD who had recently undergone open-heart surgery and pulmonary valve replacement. Sensitivity analysis excluding this study revealed a significant reduction in psychosocial QoL compared to physical QoL, underscoring the importance of addressing psychosocial health in the management of children with CHD.
This study has several limitations. First, the literature review is limited to the past decade (2015–2024). While this timeframe was considered adequate for capturing the current state of research on the QoL and CF of children and adolescents with heart disease, it may have led to the exclusion of relevant studies published before 2015. Second, this review does not account for long-term outcomes of cardiac interventions, as it focuses on studies involving pediatric and adolescent populations. As a result, research examining the health consequences and potential psychosocial comorbidities during the transition to adulthood was not included. Finally, the substantial heterogeneity of congenital and acquired heart diseases in childhood poses a challenge to generalizability. The conclusions drawn from this study may be influenced by the conditions most represented in the selected literature, introducing a potential bias and limiting their applicability to less frequently studied cardiac disorders.
Caring for children and adolescents with heart disease involves going beyond the disease itself and the surgical interventions that may be performed. Neurodevelopment and QoL are fundamental aspects that must be addressed in a preventive manner. Indeed, implementing specific intervention programs is essential for improving the QoL and cognitive functions of young CHD patients. This requires the integration of psychometric data with functional magnetic resonance imaging procedures. In recent decades, it should be noted that there has been an advance in diagnostic, therapeutic, and repair techniques, giving rise to a population that reaches adulthood with a cardiovascular disease.
This review responds to the challenges faced by children and adolescents with CHD who have undergone one or more surgical interventions, particularly regarding neurodevelopmental outcomes and executive function deficits, as examined through cohort and cross-sectional studies. However, there remains a critical gap in the literature regarding longitudinal studies that evaluate the impact of short-, medium-, and long-term interventions specifically designed for this population.
All data points generated or analyzed during this study are included in this published article.
VVH: Conceptualization, Supervision, Data curation and analysis, Methodology. SMV: Conceptualization, Data analysis, Methodology. CSM: Data analysis. MJR: Data analysis, Methodology. All authors, VVH, SMV, CSM & MJR: Writing-original draft, and Writing-review & editing and have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have final approval of the version to be published.
Not applicable.
The authors are grateful for the support of the Department of Research and Universities of the Generalitat de Catalunya to the Research Group and Innovation in Designs (GRID). Technology and multimedia and digital application to observational designs (Code: 2021 SGR 00718).
This research was funded by Next Generation EU (Generalitat de Catalunya) grant number, DDS008/22/000524.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/HSF46932.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.




