1 Department of Gynaecology and Obstetrics, Graduate School of Bengbu Medical University and Wuhu Hospital affiliated to East China Normal University (Wuhu Second People’s Hospital), 233030 Bengbu, Anhui, China
2 Department of Gynaecology, Graduate School of Bengbu Medical University and Wuhu Hospital affiliated to East China Normal University (Wuhu Second People’s Hospital), 241000 Wuhu, Anhui, China
3 Department of Gynaecology and Obstetrics, Graduate School of WanNan Medical College and Wuhu Hospital affiliated to East China Normal University (Wuhu Second People’s Hospital), 241000 Wuhu, Anhui, China
Abstract
To evaluate the efficacy of laparoscopic para-aortic lymphadenectomy in the treatment of gynecologic malignancies through a literature review comparing the extraperitoneal and transperitoneal approaches.
A comprehensive computerized search of PubMed, Embase, the Cochrane Library, Medline, Web of Science, and other relevant databases was conducted, covering the period from January 2010 to January 2025, to collect studies that compared the transperitoneal and extraperitoneal approaches to laparoscopic para-aortic lymphadenectomy in the treatment of gynecologic malignancies. Relevant data were extracted and analyzed using the Review Manager (RevMan) version 5.4.1 statistical software. Outcome indexes included operation time, intraoperative blood loss, number of para-aortic lymph nodes dissected, hospitalization days, and incidence of surgical complications.
A total of 525 manuscripts were retrieved, of which 8 were included. Our analysis showed no statistically significant differences between the extraperitoneal and transperitoneal groups in terms of operative time, intraoperative bleeding, and hospitalization days. However, the complication rate was significantly lower in the extraperitoneal group than in the transperitoneal group. Additionally, the number of para-aortic lymph nodes (PAL) retrieved was significantly higher in the extraperitoneal group compared to the transperitoneal group [mean difference (MD) = 0.43, 95% confidence intervals (CI) (0.13 to 0.72, p = 0.004)].
Laparoscopic para-aortic lymphadenectomy for gynecologic malignancies offers several advantages when performed via the extraperitoneal route. This approach reduces surgical trauma, shortens hospital stay, lowers the rate of complication, and increases the number of lymph nodes that can be resected compared to the transperitoneal route.
The study has been registered on https://www.crd.york.ac.uk/prospero/ (registration number: CRD420251033897; registration link: https://www.crd.york.ac.uk/PROSPERO/view/CRD420251033897).
Keywords
- gynecologic malignancies
- laparoscopy
- single-port laparoscopy
- extraperitoneal
- transperitoneal
- meta-analysis
Gynecologic Malignant tumors, including Cervical, Endometrial, and Ovarian Cancers are a serious threat to women’s health. According to the World Health Organization (WHO), these tumors account for approximately 19.9% of cancer mortality among women, with incidence and mortality rates rising each year. Cervical cancer rates are notably higher in low- and middle-income countries, while ovarian and endometrial cancer is more prevalent in high-income countries [1]. Despite recent advances in treatment, surgery remains the mainstay of therapy. Lymph node dissection plays a crucial role in the process; particularly, para-abdominal aortic lymph node dissection, which is essential for assessing disease spread. This procedure enhances treatment precision and improves patient prognosis, as the para-aortic lymph nodes are important lymph node areas in the abdominal cavity for tumor cell metastasis to other body parts. They are often regarded as indicators of distant metastasis for gynecological malignancies, suggesting a poor prognosis and representing a key factor in patient survival and outcomes [2]. In recent years, para-aortic lymph node dissection has been widely adopted in the surgical treatment of gynecologic malignancies. This procedure helps reduce the tumor load, complete the surgical staging guide the follow-up treatment (such as chemotherapy, radiotherapy, and targeted therapy), and improve the survival rate and quality of life of patients [3]. At present, the guidelines of the International Gynecologic Cancer Society (IGCS) and the European Society of Gynecologic Oncology (ESGO) [4, 5] recommend the necessity of systematic lymph node dissection during surgery for some early and locally advanced gynecologic malignancies, especially the para-aortic lymph node dissection, which can effectively evaluate the metastatic status of the tumor and provide a more accurate basis for the development of subsequent treatment methods.
Laparoscopic techniques have been increasingly used in gynecologic malignancies for their advantages related to less trauma and faster recovery, and laparoscopic para-aortic lymph node dissection, as a more complex surgical operation, consists of two main modalities: transperitoneal and extraperitoneal approach [6]. Although both methods are minimally invasive and widely used, their surgical technique, efficacy, and safety remain topics of debate. This study aims to reveal the differences in the outcomes of different surgical approaches for laparoscopic para-aortic lymph node dissection by including relevant literature for meta-analysis, in addition to further describing the single-port laparoscopic technique, which can provide some guidance for clinical practice.
This meta-analysis was done according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines and the review protocol was registered on PROSPERO CRD420251033897.
The literature search was conducted according to the Participants Intervention Control Outcome Study (PICOS) design principle. The databases PubMed, Embase, the Cochrane Library, Medline, and Web of Science and other relevant databases were searched from January 2010 to January 2025. Journal catalogs and references were searched. There was no restriction on the type of publication or language. The search terms were laparoscopy, extraperitoneal, transperitoneal, cervical cancer, endometrial carcinoma, ovarian cancer, lymphadenectomy, and the search strategy was (Laparoscopy) AND (extraperitoneal) AND (transperitoneal) AND (Uterine Cervical Neoplasms) OR (Endometrial Neoplasms) OR (Ovarian Neoplasms) AND (para-aortic Lymph Node Excision).
Participants: Pathologically confirmed gynecologic malignancies, including cervical, endometrial, and ovarian cancers undergoing laparoscopic para-aortic lymphadenectomy, regardless of tumor stage, provided that the surgical access method and the extent of lymph node dissection are reported.
Intervention/Exposure and Comparison/Control: Studies were included only if they compared para-aortic lymph node dissection using the extraperitoneal and transperitoneal access routes, and the procedures were performed by surgeons qualified in gynecologic oncology.
Outcomes: The number of para-aortic lymph node dissections and one or more of the following efficacy and safety indicators need to be assessed and reported in the study: operative time, intra-operative bleeding, days in hospital, incidence of surgical complications, and overall survival rate.
Study Design: Comparison of randomized controlled studies, prospective cohort studies, and retrospective cohort studies on laparoscopic extraperitoneal versus transperitoneal approaches to para-aortic lymph node dissection.
Exclusion Criteria: ① The study did not design a control group; ② Lack of original data and unavailability of full text; ③ Repeatedly published literature; ④ Not reporting surgical time, intraoperative bleeding rate, number of para-aortic lymph nodes dissected, number of hospitalization days, incidence of surgical complications, and overall survival rate as the indexes of the study; ⑤ There was no comparison of the number of para-aortic lymph node dissection in the literature, while there were other relevant indexes.
The literature obtained from the search was independently screened, and data was extracted by two researchers according to the inclusion and exclusion criteria. These findings were then cross-checked to ensure consistency and accuracy of the data, and any disagreements were resolved through discussion or negotiation with a third researcher. The extracted information included: (1) Basic information: first author, publication time, number of cases, age; (2) Analysis indices: operation time, intraoperative bleeding, postoperative hospitalization time, number of lymph node dissection, complication rate.
The quality of the literature was assessed using the Newcastle-Ottawa Scale (NOS), which evaluates three domains: selection (0–4 points), comparability (0–2 points), and outcome assessment (0–3 points), with a maximum score of 9. Studies scoring 7 or higher were considered high quality. The results of the NOS assessment are summarized in Table 1 (Ref. [7, 8, 9, 10, 11, 12, 13, 14]).
| First author (year) | Study design | Selection (0–4) | Comparability (0–2) | Outcome (0–3) | Total score | Quality |
| Díaz-Feijoo B (2016) [7] | Randomized trial | 4 | 2 | 3 | 9 | High |
| O’Hanlan KA (2015) [8] | Prospective cohort | 3 | 2 | 2 | 7 | High |
| Akladios C (2015) [9] | Retrospective cohort | 3 | 2 | 3 | 8 | High |
| Morales S (2013) [10] | Retrospective cohort | 3 | 2 | 2 | 7 | High |
| Pakish J (2014) [11] | Prospective cohort | 3 | 2 | 3 | 8 | High |
| Zhang W (2021) [12] | Retrospective cohort | 3 | 2 | 2 | 7 | High |
| Naoura I (2016) [13] | Retrospective cohort | 3 | 2 | 2 | 7 | High |
| Salhi Y (2021) [14] | Prospective cohort | 3 | 2 | 3 | 8 | High |
Meta-analysis of the extracted data was performed using Review Manager 5.4.1 (The Cochrane Collaboration, Oxford, UK). Continuous variables were expressed as mean difference (MD) with 95% confidence intervals (CI), while dichotomous variables were expressed as odds ratios (OR) with 95% CIs. Heterogeneity among studies was assessed using the I2 statistic [15]. When I2
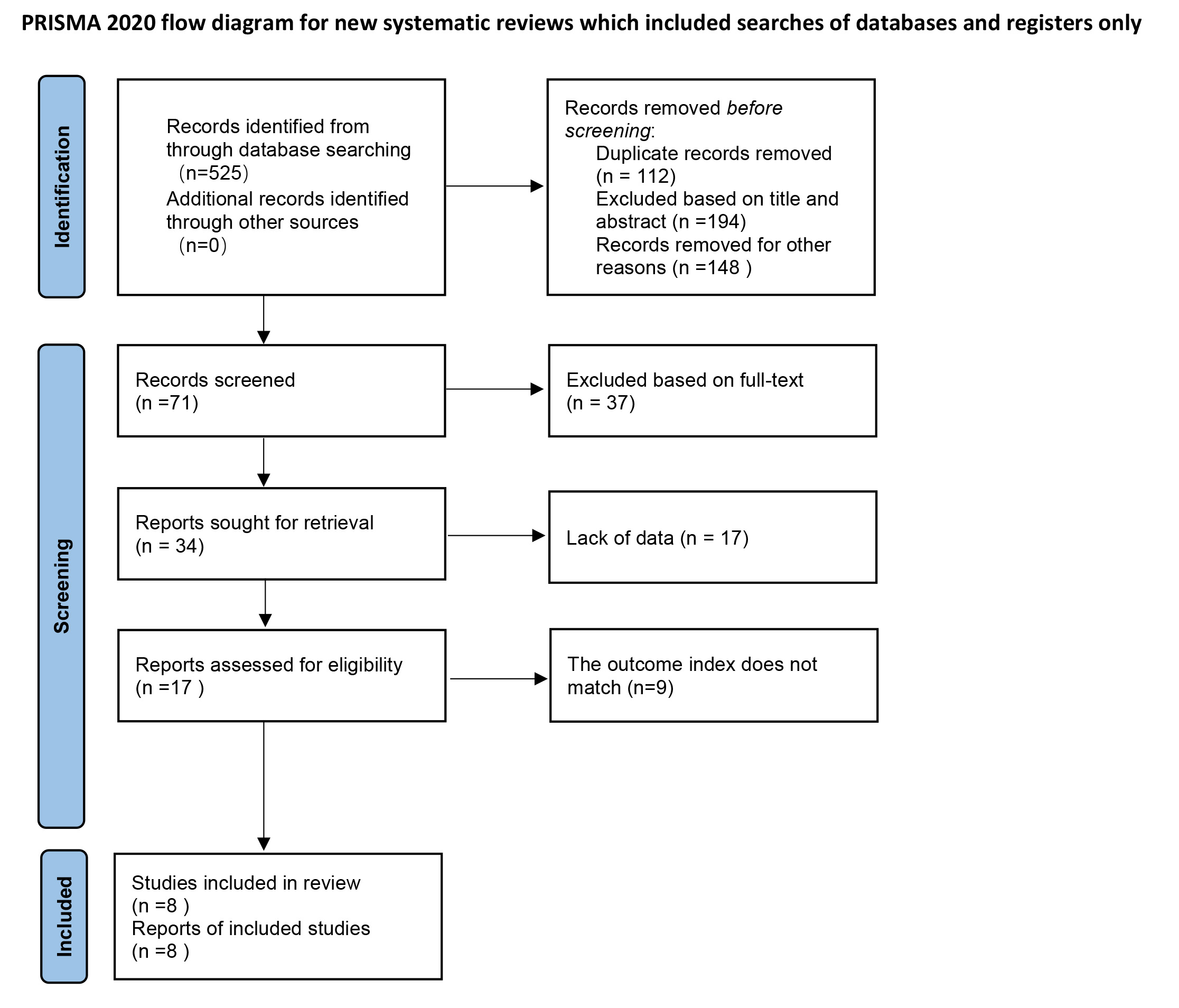
According to the search results, a total of 525 pieces of relevant literature were retrieved. Based on the inclusion and exclusion criteria, non-compliant articles were excluded, and finally, eight articles were included. The detailed steps and flowchart of the literature search are shown in Fig. 1. The basic characteristics and quality evaluation of the included literature are shown in Table 2 (Ref. [7, 8, 9, 10, 11, 12, 13, 14]).
| First author (year) | Group | N | Type of gynecological tumors | Age (years) | BMI (kg/m2) | Outcome | NOS score | ||
| Cervical cancer | Endometrial carcinoma | Ovarian cancer | |||||||
| Díaz-Feijoo B [7] | T | 29 | 0 | 22 | 7 | 65.0 (33–84) | 26.4 (20.2–40.43) | 1, 2, 3, 4, 5 | 9 |
| E | 31 | 0 | 26 | 5 | 65.0 (27–79) | 29 (18.1–42.7) | |||
| O’Hanlan KA [8] | T | 36 | 0 | 22 | 16 | 57.0 (29–80) | 26 (18–38) | 1, 2, 4, 3, 5 | 7 |
| E | 79 | 4 | 53 | 20 | 58.0 (31–77) | 26 (19–41) | |||
| Akladios C [9] | T | 51 | 22 | 8 | 20 | 53.3 (19–78) | 23.5 (16–35) | 1, 3, 4, 5 | 8 |
| E | 21 | 16 | 1 | 3 | 55.2 (38–75) | 26.9 (19–48) | |||
| Morales S [10] | T | 19 | 3 | 9 | 7 | 60.5 | 25.1 | 1, 3, 4 | 7 |
| E | 28 | 19 | 6 | 3 | 52.4 | 28.6 | |||
| Pakish J [11] | T | 108 | 0 | 108 | 0 | 61.0 (24–92) | 28.4 (17.5–53.8) | 1, 3, 5 | 8 |
| E | 34 | 0 | 34 | 0 | 62.0 (32–76) | 35.1 (20.6–47.4) | |||
| Zhang W [12] | T | 21 | 0 | 21 | 0 | 52.0 (39–70) | 24.35 (16.9–32.51) | 1, 2, 3, 4, 5 | 7 |
| E | 20 | 0 | 20 | 0 | 55.0 (41–69) | 25.45 (21.19–32.51) | |||
| Naoura I [13] | T | 62 | 22 | 29 | 11 | 54.0 | 24 | 3, 4, 5 | 7 |
| E | 67 | 41 | 22 | 1 | 56.0 | 26 | |||
| Salhi Y [14] | T | 74 | 29 | 38 | 7 | 56.4 | 25.6 | 1, 2, 3, 4, 5 | 8 |
| E | 69 | 63 | 5 | 1 | 52.9 | 25.2 | |||
Note: T, transperitoneal; E, extraperitoneal; NOS, Newcastle-Ottawa Scale; BMI, body mass index. 1. operative time; 2. intraoperative bleeding; 3. number of para-aortic lymph node dissection; 4. number of days in hospital; 5. complication rate.
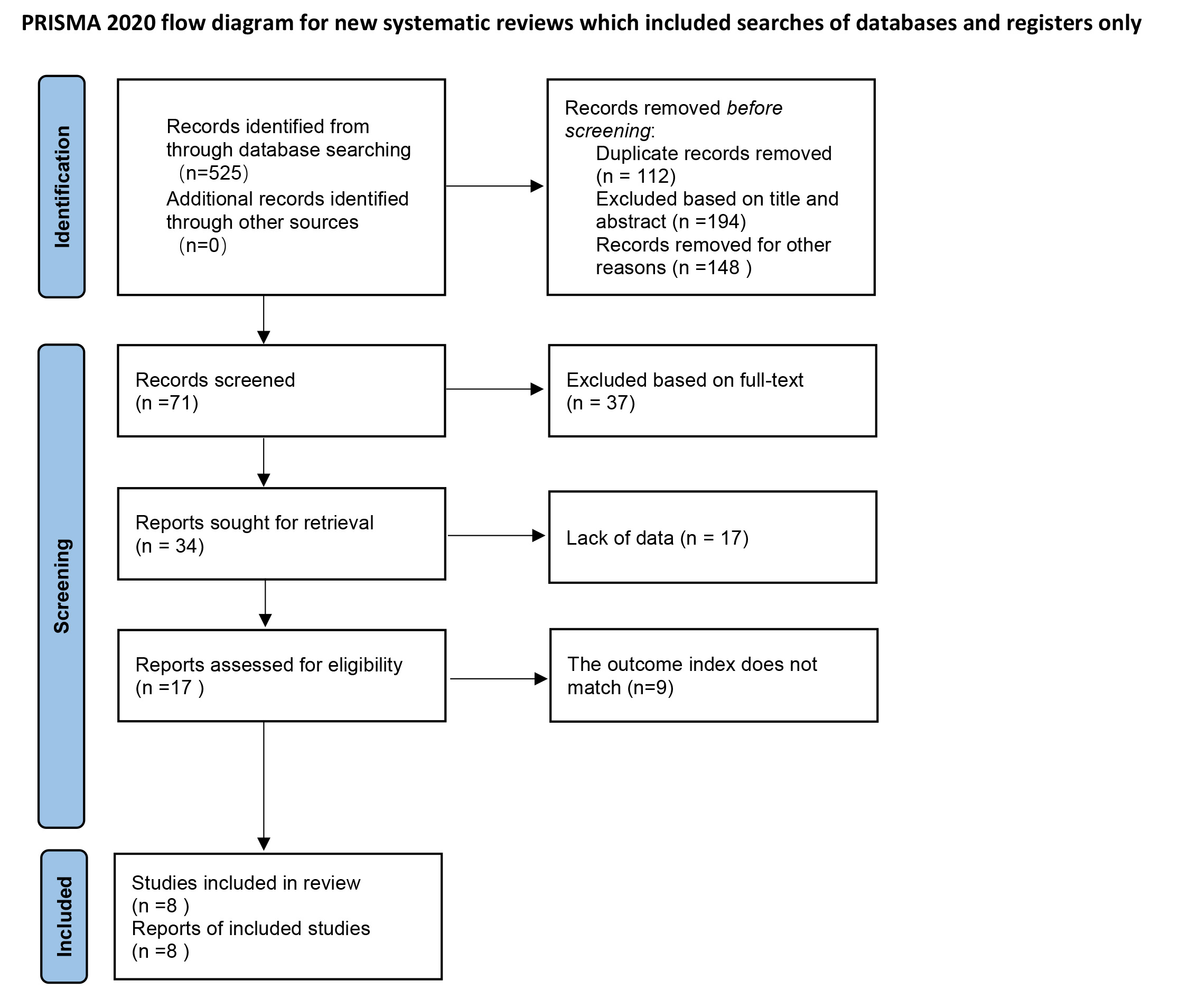 Fig. 1.
Fig. 1. Literature screening flowchart.
A total of seven papers compared the operation time, 282 cases in the extraperitoneal approach group and 338 cases in the transperitoneal approach group, and the test results suggested that I2 = 94%, with a large heterogeneity between the study groups, which was analyzed by using a random-effects model. The results of the meta-analysis showed that there was no significant difference in the operation time of the extraperitoneal approach group compared with that of the transperitoneal approach group (MD = –2.49, 95% CI: –40.39 to 35.40, p = 0.90), and the difference was not statistically significant (Fig. 2).
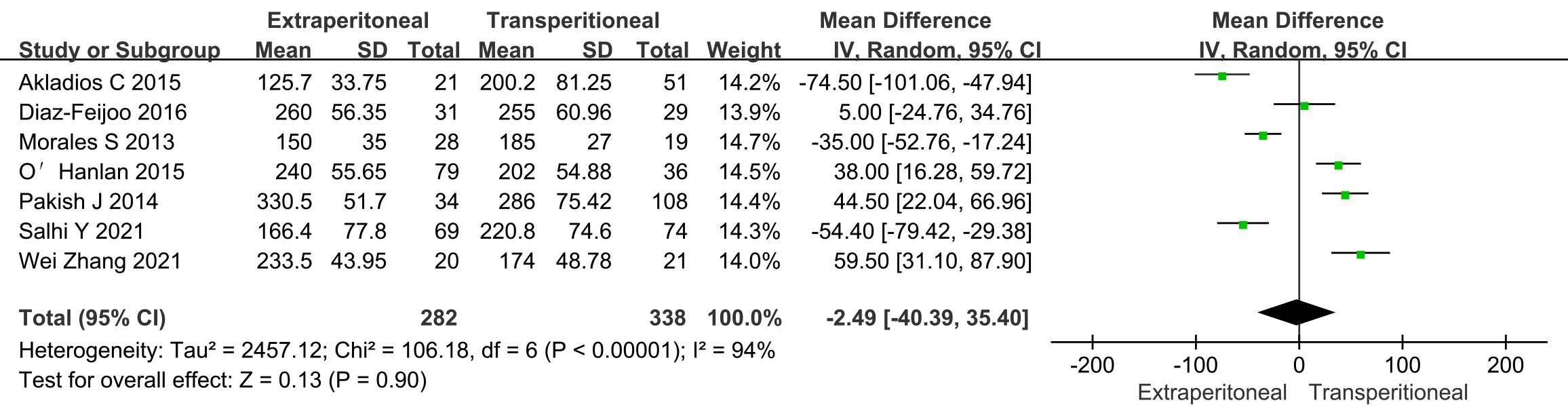 Fig. 2.
Fig. 2. Meta-analysis of operative time in extraperitoneal and transperitoneal groups. SD, standard deviation; CI, confidence interval; IV, inverse variance.
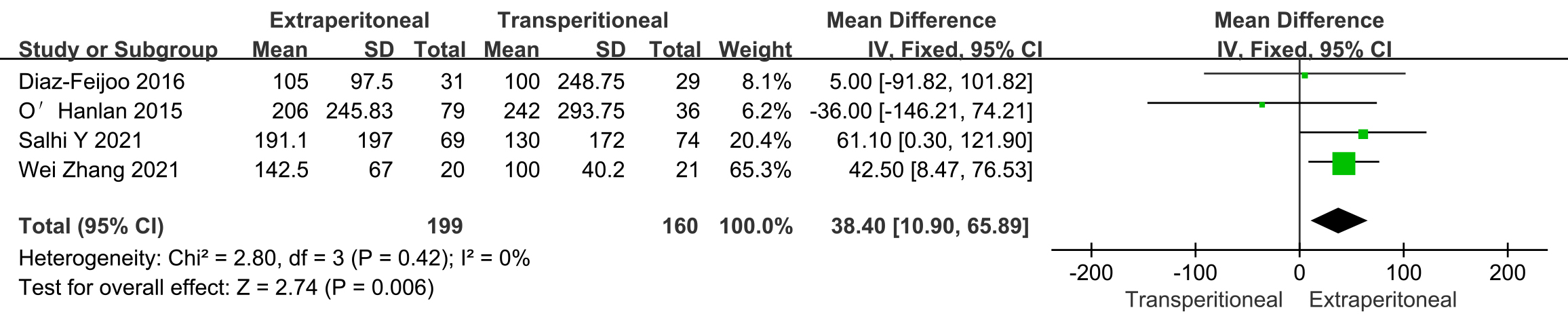
A total of four papers compared intraoperative bleeding, 199 cases in the extraperitoneal approach group and 160 cases in the transperitoneal approach group, and the test results suggested that I2 = 0%, there was no significant heterogeneity between the study groups, analyzed by using a fixed-effects model. The results of the meta-analysis showed that there were fewer cases of bleeding in the extraperitoneal compared to the transperitoneal approach group (MD = 38.40, 95% CI: 10.90 to 65.89, p = 0.006), and the difference was statistically significant (Fig. 3).
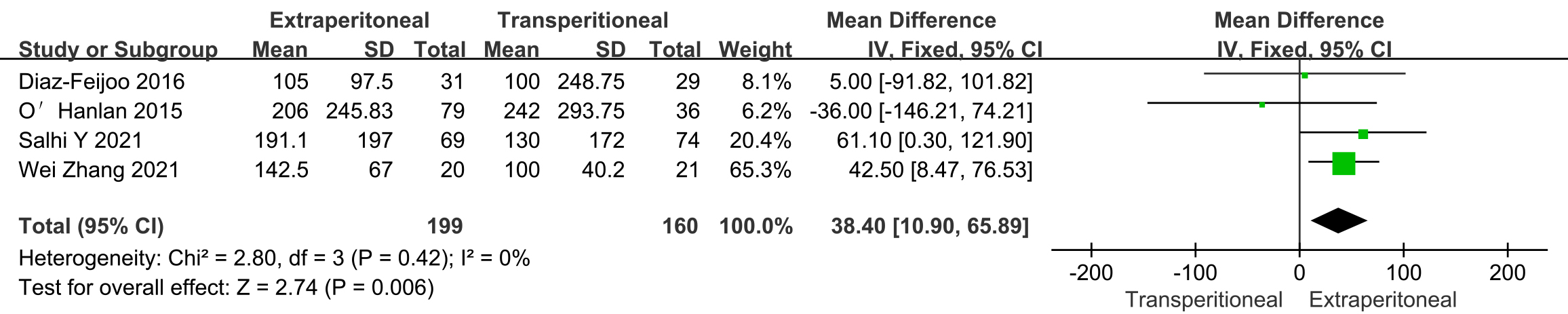 Fig. 3.
Fig. 3. Meta-analysis of bleeding in extraperitoneal and transperitoneal groups.
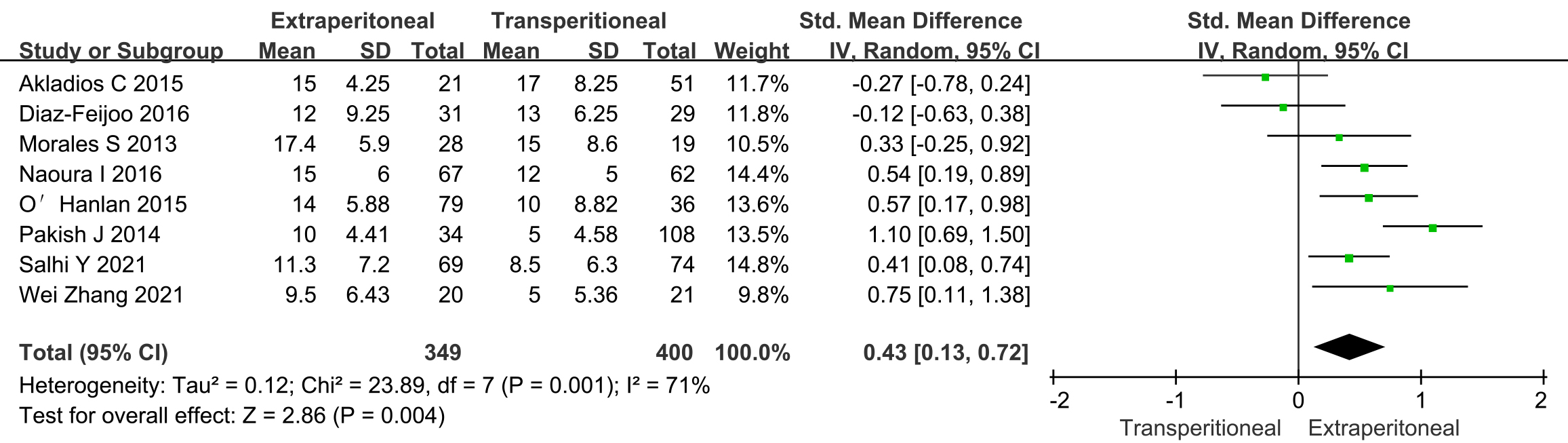
A total of eight papers compared the number of para-aortic lymph node dissection, 349 cases in the extraperitoneal approach group and 400 cases in the transperitoneal approach group, and the test results suggested that I2 = 71%, with a large heterogeneity between study groups, were analyzed using a random-effects model. The results of the meta-analysis showed that the number of para-abdominal aortic lymph node dissection was higher in the extraperitoneal than in the transperitoneal approach group (MD = 0.43, 95% CI: 0.13 to 0.72, p = 0.004), and the difference was statistically significant (Fig. 4).
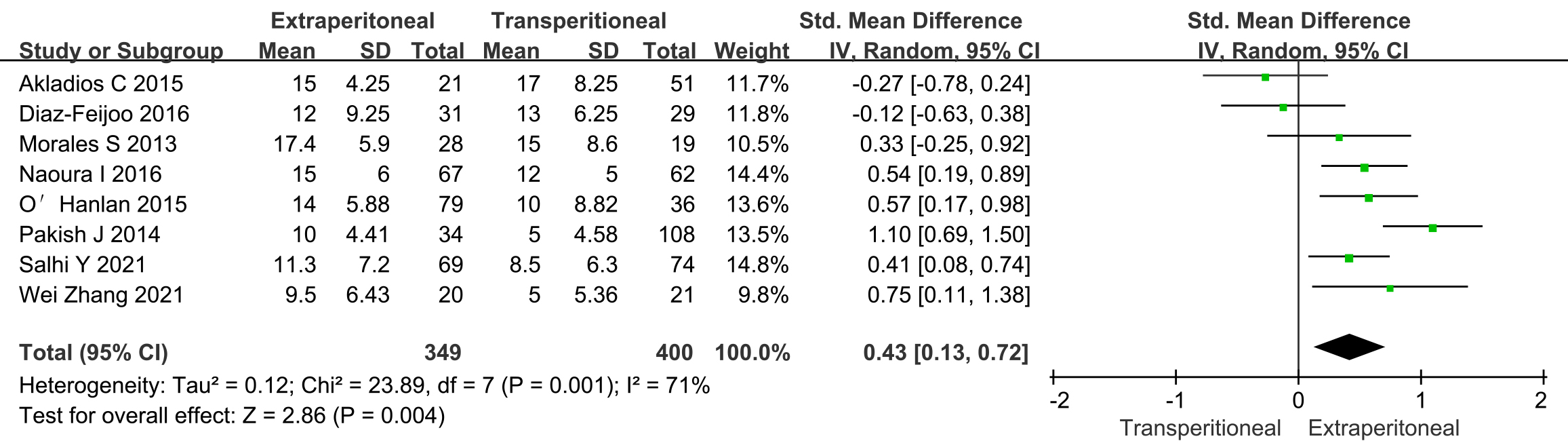 Fig. 4.
Fig. 4. Meta-analysis of resection of para-abdominal aortic lymph node number in extraperitoneal and transperitoneal groups.
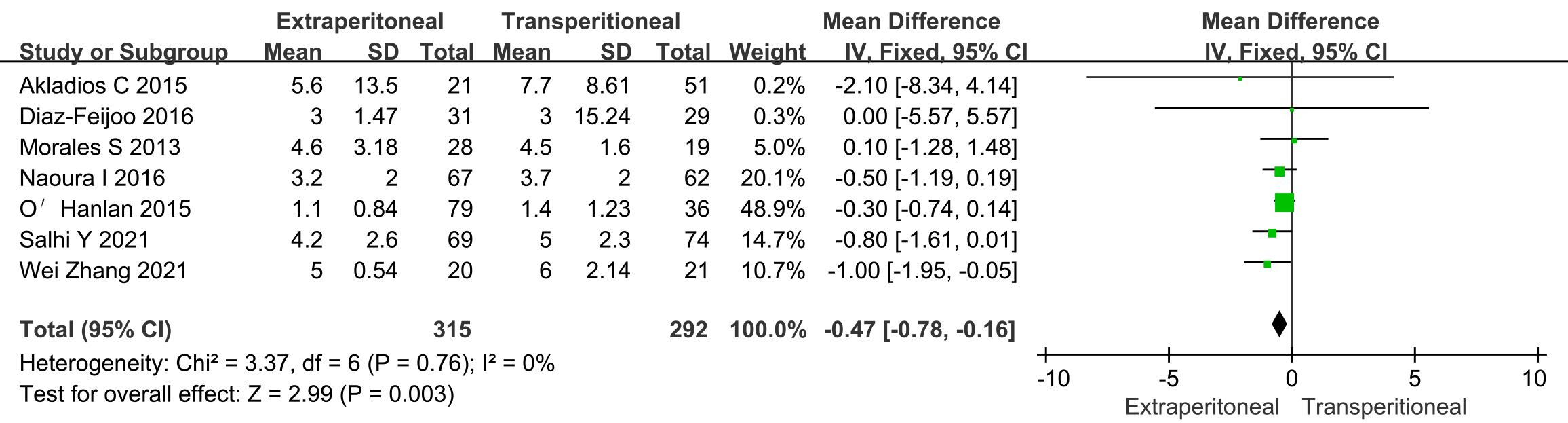
A total of seven studies compared the number of hospitalization days between 315 cases in the extraperitoneal access group and 292 cases in the transperitoneal access group. The analysis revealed I2 = 0%, indicating no significant heterogeneity between the study groups, and a fixed-effects model was employed. The results of the meta-analysis showed that the number of hospitalization days was shorter in the extraperitoneal compared to the transperitoneal access group [MD = –0.47, 95% CI: –0.78 to –0.16, p = 0.003], and the difference was statistically significant (Fig. 5).
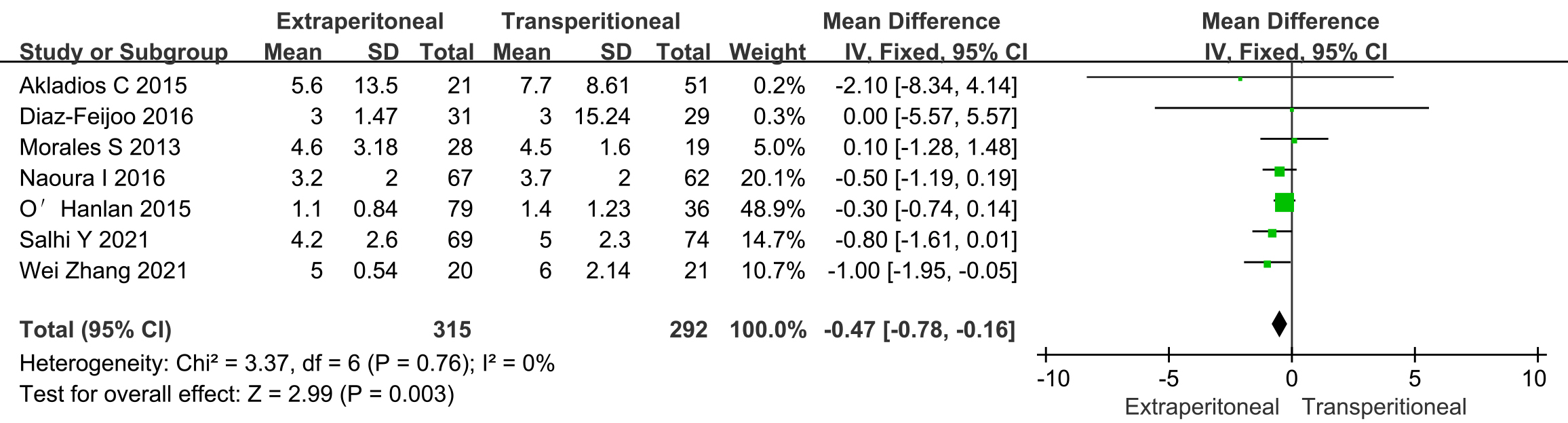 Fig. 5.
Fig. 5. Meta-analysis of in-hospital stay in extraperitoneal and transperitoneal groups.
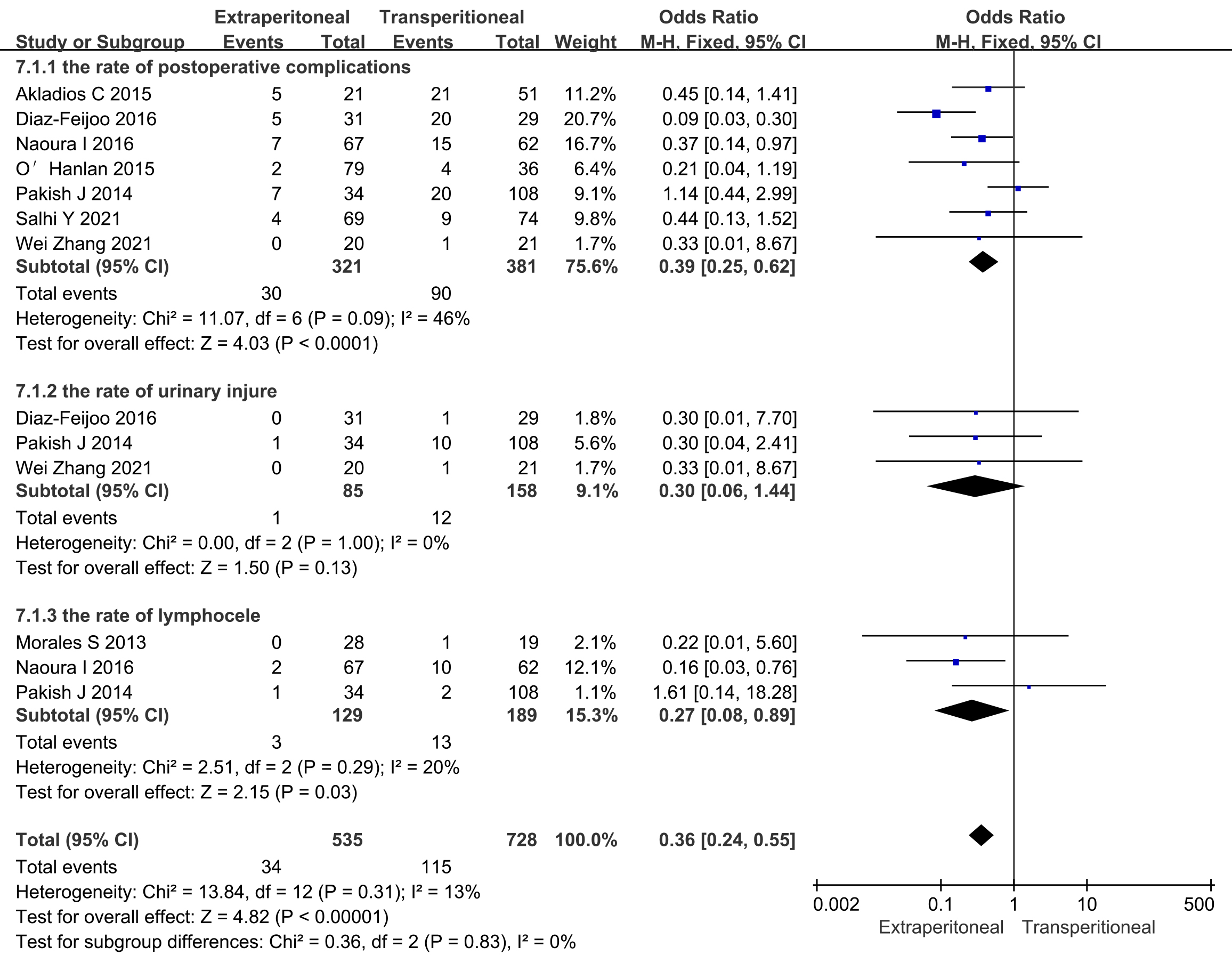
Additionally, seven studies compared the incidence of surgical complications, which were analyzed using a fixed-effects model due to the small heterogeneity among the study groups. Meta-analysis showed that the overall incidence of surgical complications was less in the extraperitoneal than in the transperitoneal approach group (OR = 0.39, 95% CI: 0.25 to 0.62, p
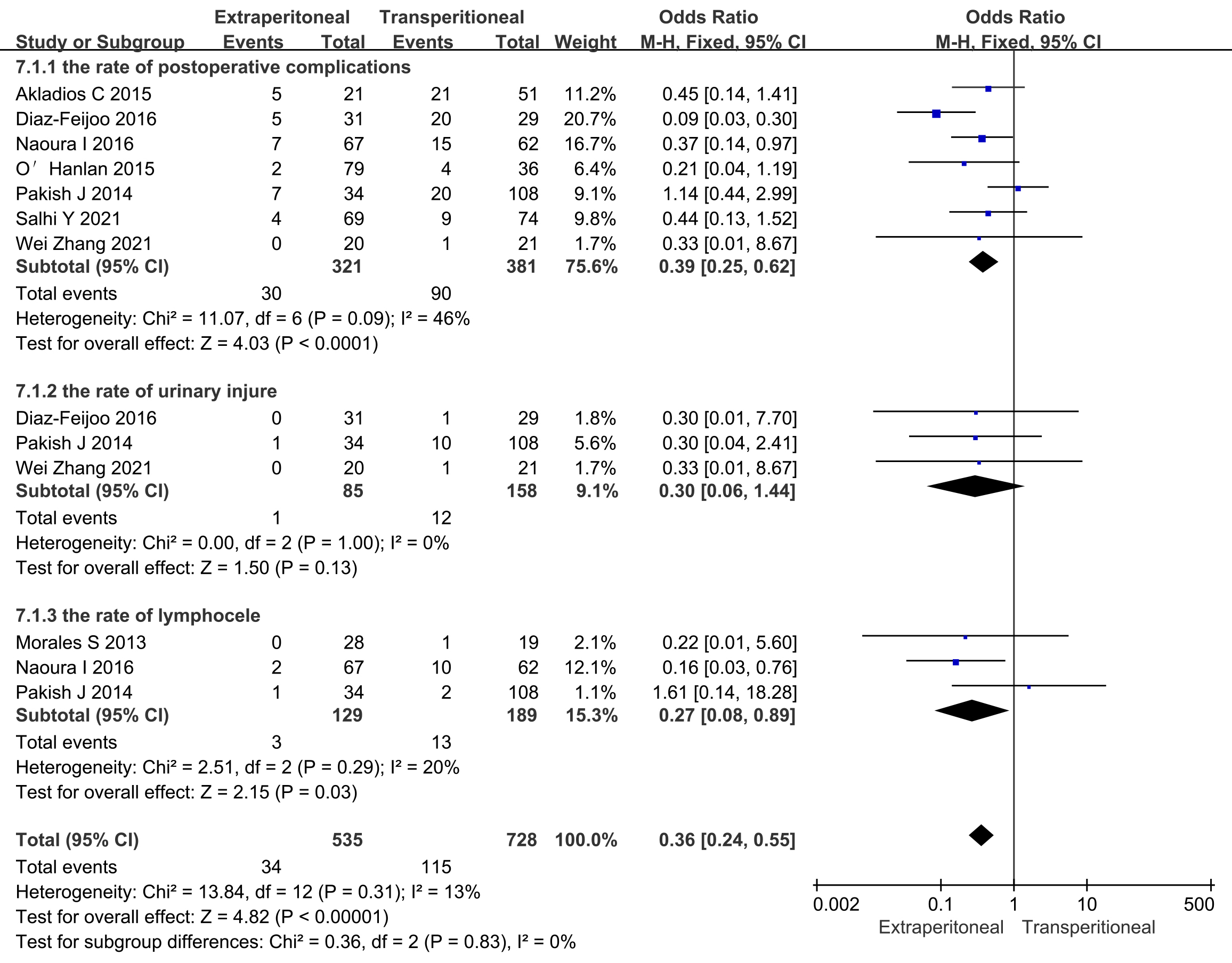 Fig. 6.
Fig. 6. Meta-analysis of surgical complication in extraperitoneal and transperitoneal groups. M-H, Mantel-Haenszel.
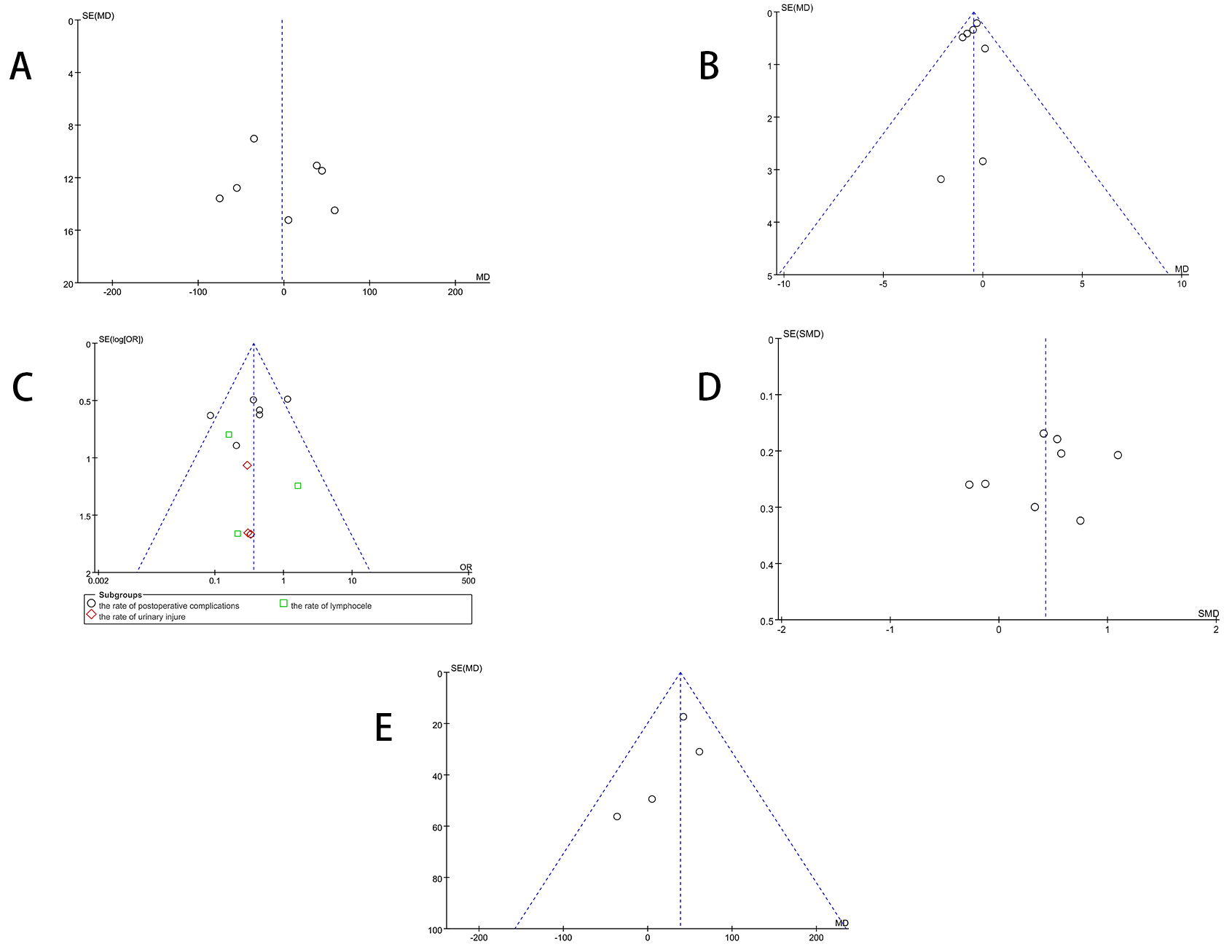
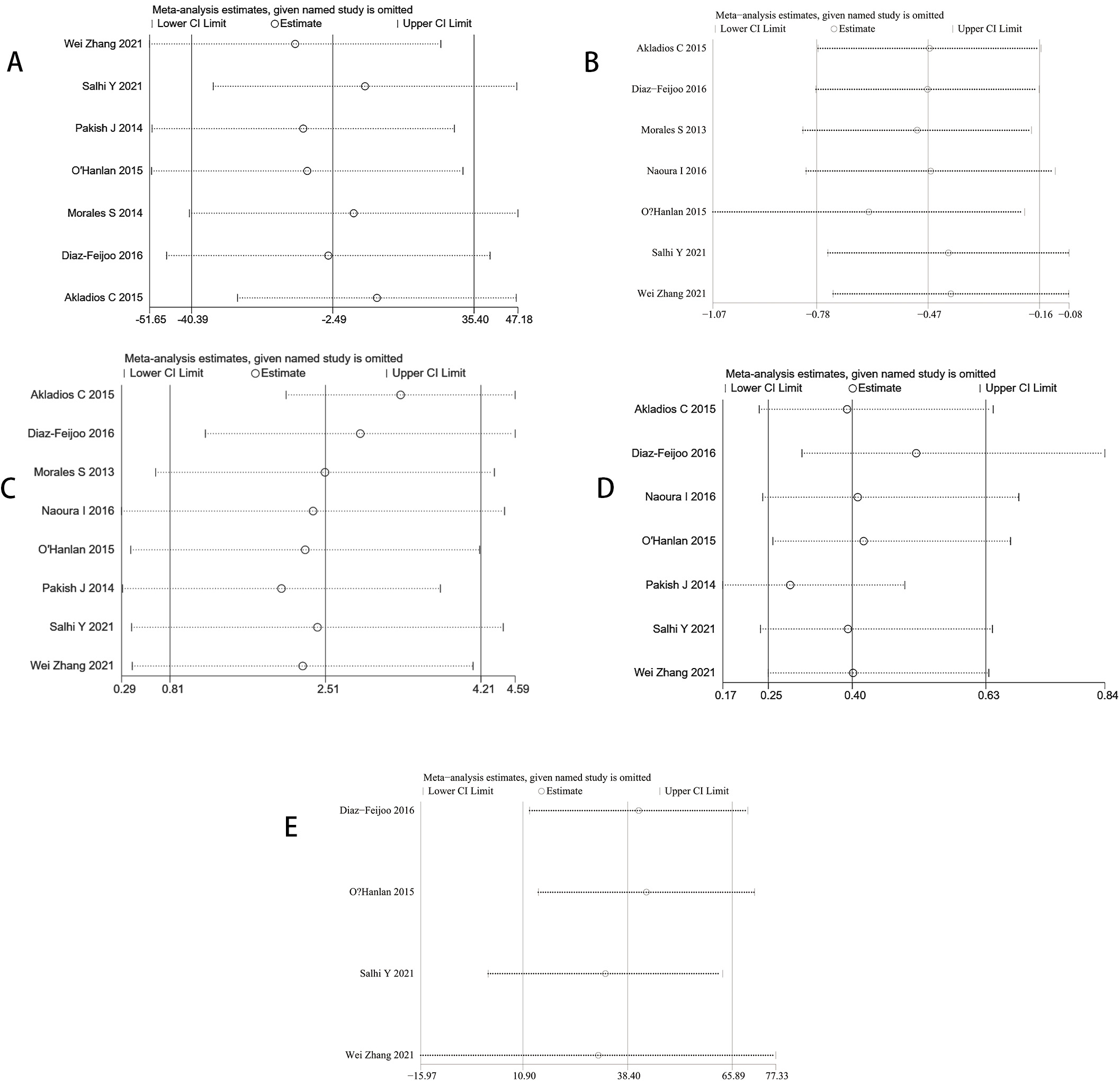
A funnel plot of relevant indicators was observed (Fig. 7). A leave-one-out sensitivity analysis was conducted (Fig. 8), to reassess the combined effect size of the included studies by excluding each study one at a time. If the results changed significantly after excluding a study, it indicated that the study had a greater impact on the overall analysis results. Conversely, if the results did not change significantly, it indicated that the analysis was highly robust to the selection of studies. Notably, when the study by Zhang et al. [12] was excluded, a significant change was observed when comparing the extraperitoneal group with the transperitoneal group in terms of intraoperative bleeding. Subsequent exclusions of other studies in turn resulted in little change in the number of abdominal aortic lymph node resections, operative time, hospitalization days, and complication rates. Furthermore, The operative time sensitivity analysis findings (e.g., Fig. 8A) demonstrated that the aggregated effect size remained stable throughout the exclusion of individual studies, underscoring the robustness of the study outcomes. Notably, even upon removal of studies with total sample sizes
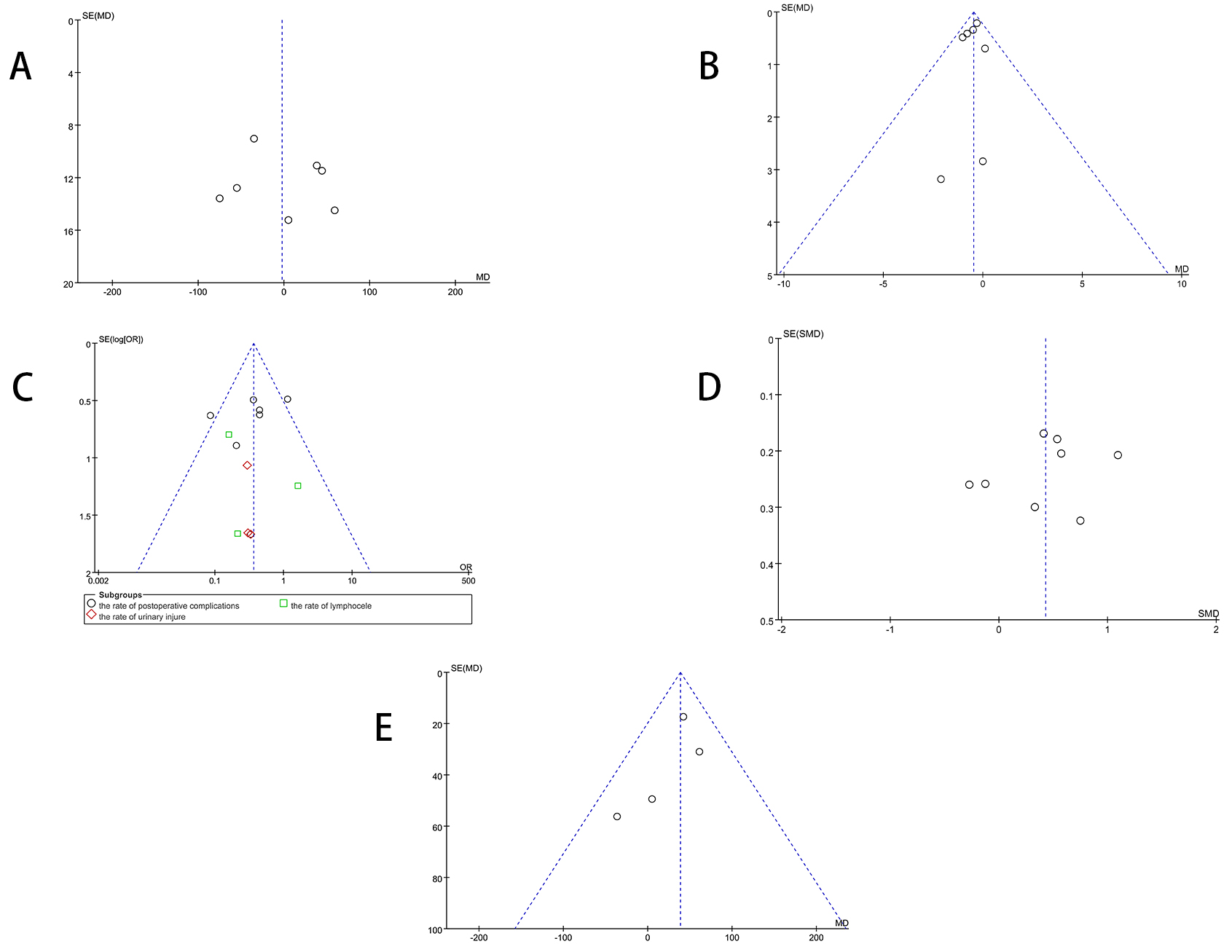 Fig. 7.
Fig. 7. Funnel plot. (A) Operative time. (B) Days of hospitalization. (C) Complications. (D) Number of para-aortic lymph nodes. (E) Bleeding. OR, odds ratio
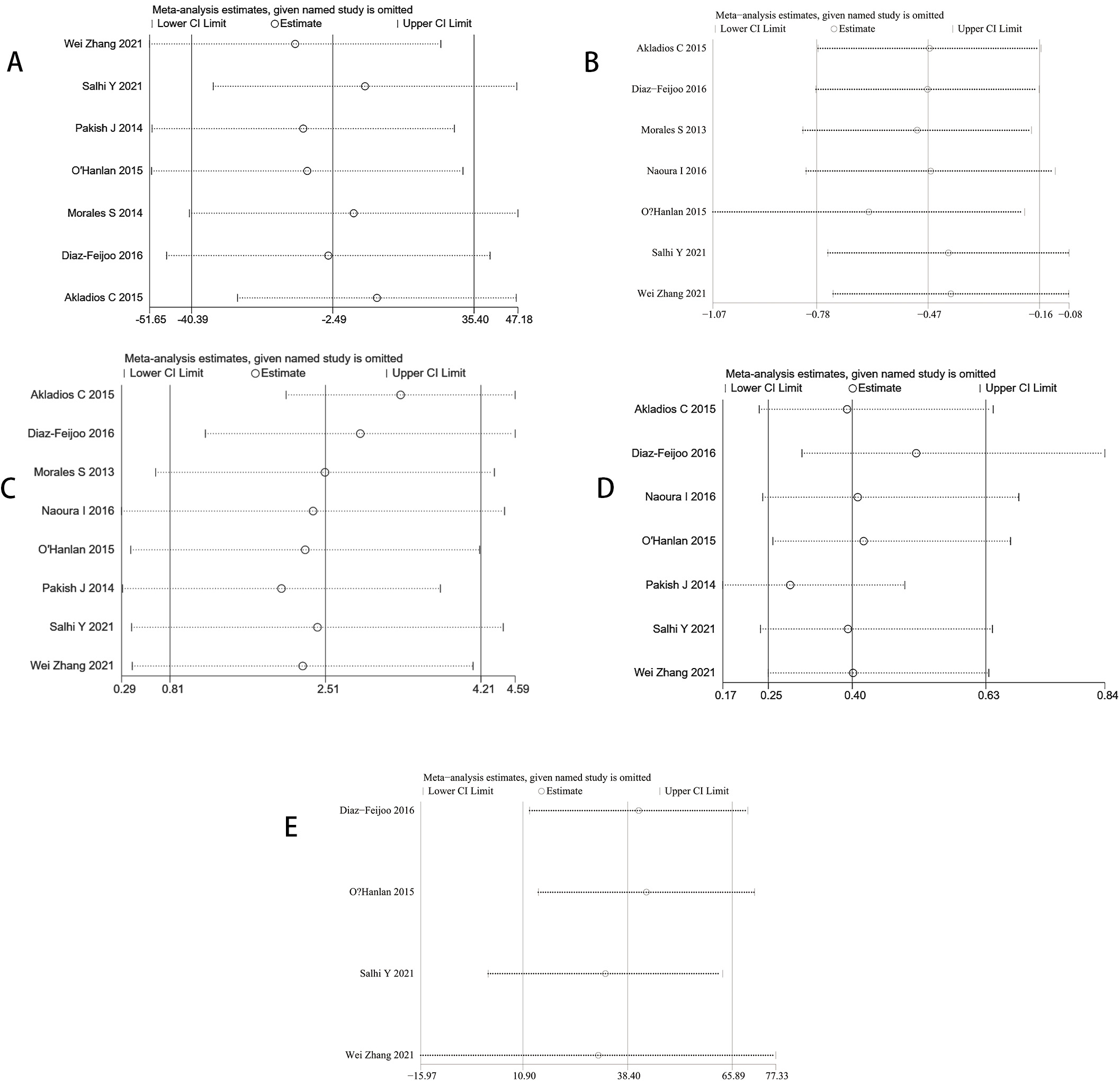 Fig. 8.
Fig. 8. Sensitivity analysis graph. (A) Operation time. (B) Hospitalization days. (C) Number of para-aortic lymph nodes. (D) Complications. (E) Bleeding.
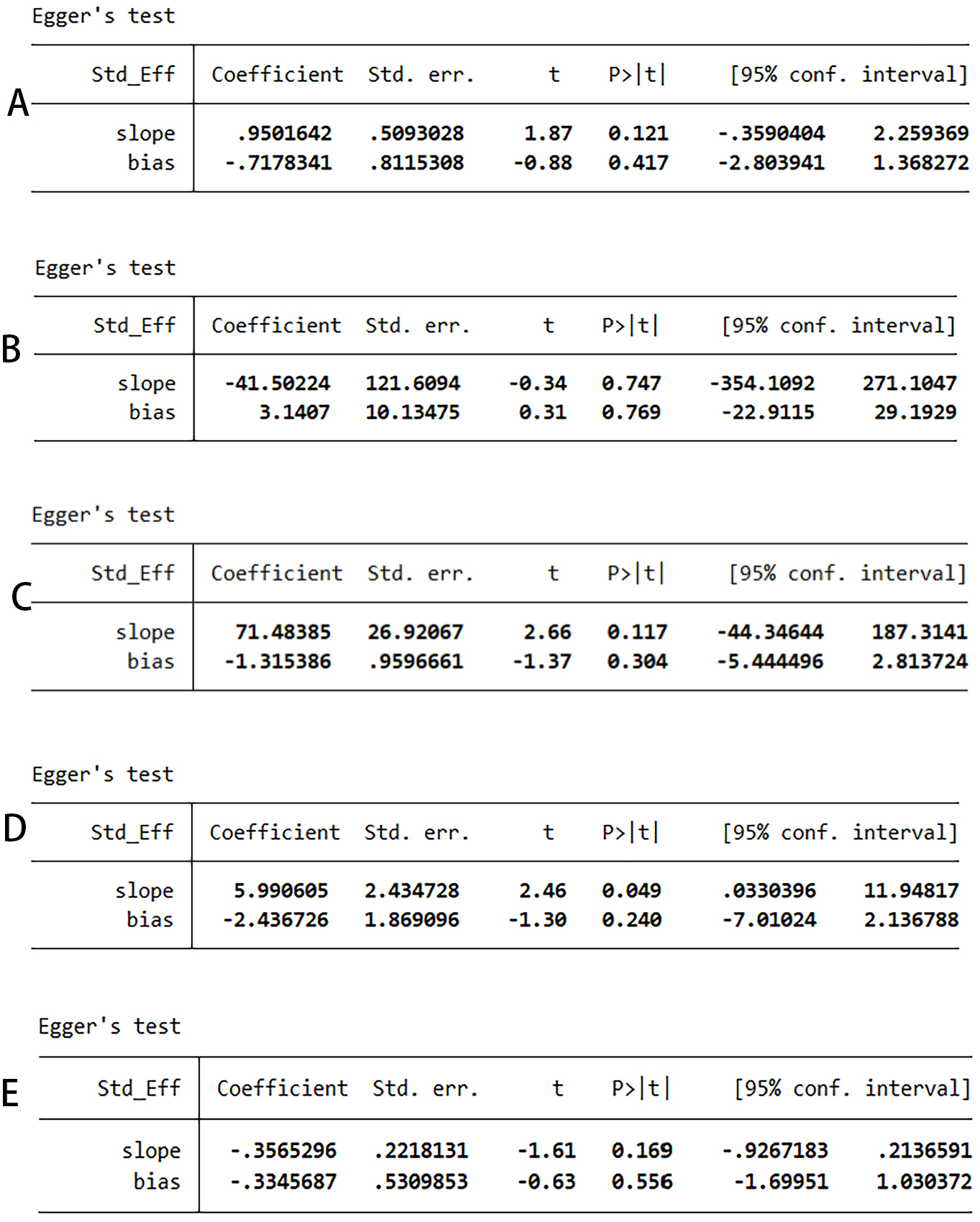
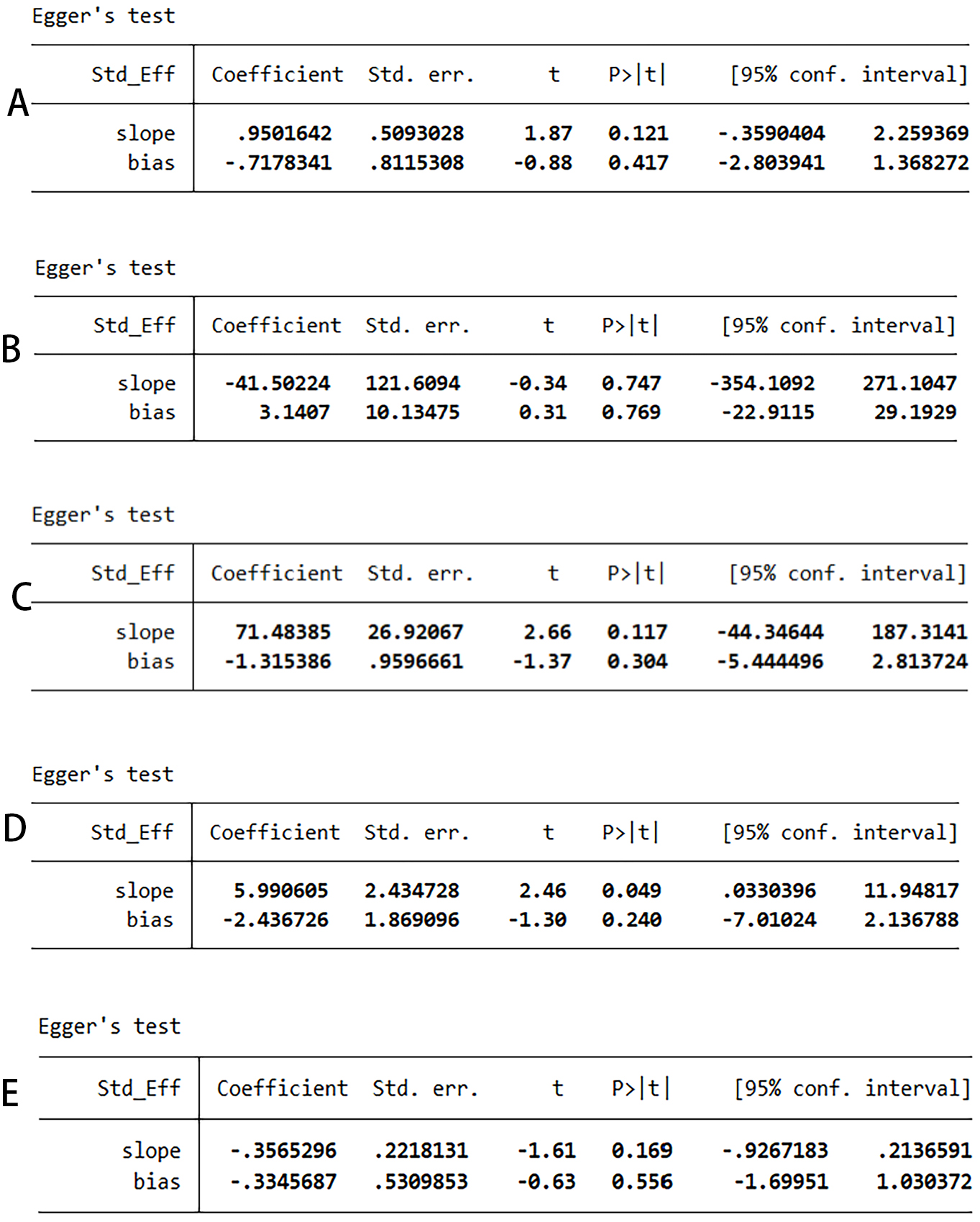 Fig. 9.
Fig. 9. Egger test. (A) Complications. (B) Operation time. (C) Bleeding. (D) Number of para-aortic lymph nodes. (E) Hospitalization days.
Surgery remains the standard of care for the treatment of gynecologic malignancies, with the para-aortic lymph nodes representing an important route of metastatic spread [16]. The resection of para-aortic lymph nodes is an accurate indicator for determining lymph node involvement, which plays a critical role in disease evaluation, formulation of subsequent treatment strategies, and prognosis [17]. In laparoscopy, the choice of surgical route—whether transperitoneal or extraperitoneal—has a significant impact on surgical outcomes. In this study, the surgical time, intraoperative bleeding, hospitalization time, and surgical complication rate were used as indicators of surgical safety, and the number of para-aortic lymph node dissections was used as an indicator of surgical effectiveness.
Laparoscopic techniques began to develop rapidly in the late 1980s and early 1990s. In recent years, laparoscopic para-aortic lymph node dissection has become increasingly proficient, establishing it as the preferred surgical approach among gynecologic oncologists [18].
There are two main routes for laparoscopic surgery: the transabdominal and the extraperitoneal routes. The first laparoscopic extraperitoneal approach for pelvic lymph node dissection for gynecologic oncology in 1987 was performed by Dr. Dargent [19]. The first para-abdominal lymph node dissection using the extraperitoneal approach was performed in 1996 by Vasilev and McGonigle [20]. This study showed that intraoperative bleeding, hospitalization days, and the surgical complication rate of parietal abdominal aortic lymph node dissection by the extraperitoneal route were superior to those of the transperitoneal route, while there was no significant difference in operative time in both groups. The extraperitoneal approach to para-aortic lymphadenectomy has limited operating space and complex anatomy of the posterior peritoneum, which involves numerous large vessels and peripheral nerves, and it takes time to enter the retroperitoneal space [17]; however, the transperitoneal route is susceptible to the influence of body position and intestinal canal, and the patient’s history of previous abdominal surgery will lead to surgical difficulties and an increase in the incidence of pelvic-abdominal adhesion in the postoperative period, which will affect the operation time, bleeding volume, and lead to postoperative complications of transperitoneal the route [17]. Transperitoneal surgery can be more challenging for obese patients (body mass index
The number of para-aortic lymphadenectomies is an important index of effectiveness, and the results of this study showed that the number of lymph nodes removed by the laparoscopic extraperitoneal route was more than that of the transperitoneal route, [MD = 0.43, 95% CI: 0.13 to 0.72, p = 0.004], and the difference was statistically significant, see Fig. 4. Akladios et al. [9] found that the extraperitoneal route had a significant advantage in patients with body mass index (BMI)
In addition, different patient groups, different surgical teams, and different levels of experience also affect the number of lymph node dissections. For gynecologic malignant tumors undergoing abdominal para-aortic lymph node dissection, the long-term survival rate to evaluate the effect of surgical treatment is still the focus of attention [27]. Due to the relatively small sample size of the relevant literature included in the study and the limitation of the follow-up time, there is still no definitive conclusion on the impact of different surgical approaches on long-term survival. Further studies on the long-term survival rate and postoperative quality of life are still needed.
The status of lymph node has increasingly been recognized as one of the most critical prognostic indicators of gynecologic malignancies [28]. Lymphatic metastasis remains one of the most independent and significant predictors of poor prognosis in both endometrial and cervical cancers. In recent years, sentinel lymph node (SLN) mapping has emerged as a widely adopted, minimally invasive alternative in the clinical management of gynecologic cancers. A study by Bogani et al. [29] demonstrated that SLN mapping in endometrial cancer achieves a sensitivity exceeding 95%, while significantly reducing postoperative complications such as lymphedema. Furthermore, Cuccu et al. [30] through a five-year follow-up, confirmed that SLN mapping combined with selective lymphadenectomy achieves tumor control rates comparable to traditional full lymphadenectomy in high-risk patients, supporting its feasibility as a standard staging strategy.
Treatment paradigms for cervical cancer have also undergone substantial changes in recent years. With the widespread implementation of human papillom avirus (HPV) vaccination and HPV-DNA screening, early detection rates have improved, allowing more patients to be eligible for fertility-sparing surgical options [31]. The Early-sTage cERvical caNcer scheduled for fertilItY-sparing approach (ETERNITY) project led by Bogani et al. [32] demonstrated that SLN evaluation could effectively replace systematic lymphadenectomy in patients with International Federation of Gynecology ang Obsterics (FIGO) stage IB1 cervical cancer without compromising oncologic outcomes, particularly benefiting those undergoing fertility-preserving procedures. Another study by Bogani et al. [33] evaluated a combined approach of neoadjuvant chemotherapy and cervical conization with concurrent SLN assessment for patients with tumors larger than 2 cm. The results indicated favorable outcomes in both local disease control and fertility preservation. Additionally, recent multicenter studies [32, 33] further confirmed that SLN evaluation, in combination with minimally invasive techniques, is becoming an integral component of personalized treatment in early-stage cervical cancer.
Although this study did not include data on single-port extraperitoneal laparoscopic techniques, this field has developed rapidly in recent years and shows promising clinical potential. Single-port laparoscopy has been increasingly applied in gynecologic oncology due to its minimal invasiveness, faster postoperative recovery, and favorable cosmetic outcomes [34]. The single-port extraperitoneal approach for para-aortic lymphadenectomy was introduced, demonstrating potential advantages in reducing intraoperative blood loss, shortening hospital stay, and lowering postoperative complications [35]. Subsequent studies by Lambaudie et al. [36] and Beytout et al. [37] further confirmed its benefits in terms of improved postoperative recovery and fewer complication rates. However, conventional single-port techniques are limited by restricted operative space and suboptimal surgical exposure, which may compromise the completeness of lymph node dissection. To overcome these limitations, “Zheng’s trans umbilical single-port laparoscopic technique” was proposed in 2022 [38]. This approach utilizes a midline umbilical incision to access the extraperitoneal space, effectively resolving spatial and instrument interference issues without the need for additional auxiliary ports. It enables systematic pelvic and para-aortic lymphadenectomy, even up to the level of the renal vessels. Theoretically, this technique minimizes peritoneal disturbance, reduces the risk of postoperative adhesions, and offers advantages for obese patients and those seeking fertility preservation [39]. Nevertheless, current evidence is limited to small-sample, single-center retrospective studies. High-quality prospective, multicenter trials with large sample sizes are needed to validate its actual performance in terms of intraoperative feasibility, completeness of lymphadenectomy, perioperative complication rates, and long-term disease-free survival. Although this technique requires high surgical expertise and has a steep learning curve, its clinical potential is expected to grow with the ongoing refinement of surgical instruments, improved surgeon proficiency, and the integration of novel assistance technologies such as robotic systems.
This meta-analysis incorporated eight articles into its two-group analysis. The quality of the literature varied appreciably, introducing potential bias risk. Additionally, variability in trial designs among the included studies might influence the reliability of the results and the generalizability of the conclusions. Furthermore, this study did not evaluate long-term outcomes such as recurrence rate, survival rate, or similar outcomes; these aspects warrant further investigation. Thus, there is a pressing need for multicenter, large-sample, high-quality randomized controlled studies to validate these conclusions and provide further evidence-based insights into long-term prognosis and survival metrics.
In summary, both surgical approaches are safe and effective when laparoscopic para-aortic lymph node dissection is performed for gynecologic malignancies. Compared with the transperitoneal route, the extraperitoneal route showed certain advantages in reducing surgical trauma, shortening hospitalization time, decreasing the complication rate, and increasing the number of lymph node dissection. Future studies need to further explore the effects of different surgical routes on the long-term prognosis of gynecologic malignant tumor patients and optimize the surgical techniques to improve the therapeutic effect. Meanwhile, with the continuous development of minimally invasive techniques, the application of new techniques such as single-port laparoscopy in gynecologic malignant tumor surgery also deserves further attention and research.
The original contributions presented in the study are included in the article. Publicly available datasets were analyzed in this study. This data can be found in: PubMed, Embase, Cochrane Library, Medline, and Web of Science databases from January 2010 to January 2025 for relevant publications.
HX and ML conceived and designed the study. JS, XL and QW were involved in literature search and data collection. HX and ML analyzed the data. ML wrote the article, XL reviewed and edited the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Not applicable.
We would like to express our gratitude to all those who helped us during the writing of this manuscript. Thanks to all the peer reviewers for their opinions and suggestions.
This study was supported by the scientific research project of Wuhu Municipal Health Commission, the project number was WHWJ2021y033.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/CEOG40053.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.