1 Department of Ultrasound, Department of Obstetrics and Gynecology, Women and Children’s Hospital, School of Medicine, Xiamen University, 361102 Xiamen, Fujian, China
†These authors contributed equally.
Abstract
To elucidate the prenatal ultrasonographic characteristics and clinical prognosis of fetal intestinal volvulus in the absence of malrotation, a rare and potentially life-threatening condition.
A retrospective analysis was conducted on seven cases of fetal intestinal volvulus diagnosed prenatally using ultrasound at the Women and Children’s Hospital, School of Medicine, Xiamen University, between July 2021 and December 2024. Ultrasonographic findings, including the whirlpool and vascular spiral signs, were correlated with postnatal surgical or autopsy outcomes, operative reports, intraoperative findings, postoperative pathology, and clinical recovery data.
Maternal age ranged from 24 to 34 years, with initial diagnoses made at 23–33 weeks of gestation. All seven cases exhibited whirlpool and vascular spiral signs, with additional findings including bowel dilation (7/7), ascites (6/7), abdominal pseudocysts (2/7), and coffee bean sign (2/7). A total of 27 ultrasound examinations were performed, with whirlpool and vascular spiral signs detected in 20 of the 27 examinations. Six fetuses were born alive (five preterm) and underwent neonatal surgery, confirming volvulus with necrosis and intestinal atresia (four type III) in five cases. One pregnancy was terminated because of parental concerns about severe complications, with an autopsy confirming volvulus and necrosis.
Fetal intestinal volvulus exhibits distinct ultrasonographic features, including whirlpool and vascular spiral signs, which enable early and precise prenatal diagnosis. This provides a critical foundation for timely intervention decisions and improved perinatal outcomes. Prenatal ultrasound is instrumental in identifying volvulus early, facilitating multidisciplinary perinatal collaboration, optimizing prenatal counseling, and enhancing fetal outcomes through timely postnatal management.
Keywords
- fetal intestinal volvulus
- prenatal ultrasound
- whirlpool sign
- vascular spiral sign
- intestinal atresia
Fetal intestinal volvulus, an uncommon yet potentially devastating anomaly characterized by the aberrant rotation of the intestinal tract around the mesenteric axis, poses a formidable challenge in prenatal diagnostics due to the rarity and propensity of the condition for severe complications. With an estimated incidence of symptomatic neonatal malrotation of approximately 1 in 6000 live births [1, 2, 3], volvulus without malrotation constitutes an even rarer subset, rendering the prenatal identification of the condition both critical and elusive. The pathophysiology of the condition, driven by mechanical torsion of the mesentery, precipitates a cascade of adverse sequelae, including intestinal necrosis, atresia, perforation, meconium peritonitis, and ascites, each of which significantly elevates the risk of fetal and neonatal morbidity or mortality [4, 5]. The absence of specific antenatal clinical manifestations further complicates timely diagnosis, often delaying intervention until irreversible damage has occurred, underscoring the imperative for advanced imaging modalities to facilitate early detection and inform clinical management.
Prenatal ultrasound has emerged as a crucial tool in elucidating the characteristic features of fetal intestinal volvulus, notably the whirlpool sign—a spiral configuration of dilated bowel loops—and the vascular spiral sign, wherein the mesenteric vein encircles the mesenteric artery on Doppler imaging [6, 7]. These ultrasonographic hallmarks enable early diagnosis, thereby informing intervention strategies and enhancing neonatal prognosis. These ultrasonographic hallmarks, complemented by nonspecific findings such as bowel dilation and ascites, can allow clinicians to differentiate volvulus from other causes of fetal abdominal pathology, thereby guiding critical decisions regarding prenatal counseling and postnatal surgical planning. Recent studies have further refined the diagnostic utility of these signs, highlighting the specificity of these signs in identifying volvulus and their prognostic implications in complications such as atresia and necrosis [8, 9]. Larger case series, such as those reported by Taşdemir et al. [10] and Montironi et al. [1], have further underscored the heterogeneity of volvulus presentations and the pivotal role of ultrasound in optimizing outcomes; however, the literature remains sparse in cases without malrotation, a distinct entity that may arise from alternative etiological mechanisms, such as localized ischemia or transient intrauterine obstructions [11].
The rarity of fetal intestinal volvulus without malrotation, coupled with its diagnostic complexity, necessitates detailed characterization of the ultrasonographic and clinical profiles involved to enhance prenatal management strategies. The absence of malrotation, typically associated with aberrant mesenteric vessel positioning, suggests that mechanical or vascular insults may independently precipitate volvulus, a hypothesis warranting further investigation. Moreover, the frequent association with intestinal atresia, as reported in prior studies, underscores the need to elucidate the interplay between volvulus-induced ischemia and developmental anomalies, which may inform risk stratification and therapeutic approaches [4, 12]. Despite the challenges posed by the low incidence of the condition, which limits large-scale studies, case series, such as the present investigation, offer valuable insights into its diagnostic and prognostic nuances, contributing to the evolving landscape of fetal medicine.
This study aimed to delineate the prenatal ultrasonographic characteristics and clinical outcomes of seven cases of fetal intestinal volvulus without malrotation diagnosed at a tertiary care center between July 2021 and December 2024. By correlating ultrasonographic findings, including whirlpool and vascular spiral signs, with postnatal surgical or autopsy results, this study sought to elucidate the diagnostic reliability of ultrasound and its impact on clinical decision-making. Through a detailed analysis of these rare cases, we aimed to provide a robust evidence base for prenatal counseling, enhance early detection, and inform strategies to mitigate the severe complications associated with this condition, thereby addressing a critical gap in the literature and advancing the field of prenatal diagnostics.
A total of 31,764 pregnant women underwent routine ultrasound examination at the Department of Ultrasound, Women and Children’s Hospital, School of Medicine, Xiamen University between July 2021 and December 2024. Seven fetuses were diagnosed with intestinal volvulus via prenatal ultrasound, with diagnoses confirmed by postnatal surgery or autopsy. Written informed consent was obtained from all participants, and the study was approved by the Institutional Ethics Committee (KY-2024-079-K01), adhering to established ethical standards.
Examinations were performed using GE (General Electric Company, Waukesha, WI, USA) Voluson E8 or E10 color Doppler ultrasound systems equipped with a 3.5–5.0 MHz convex array probe. A standardized protocol was employed, involving systematic obstetric screening followed by detailed fetal bowel assessment when abnormalities, such as bowel dilation, were detected. To ensure diagnostic consistency, all examinations were conducted by ultrasonographers with specialized training in fetal anomaly detection, with consultation from a chief physician for suspected volvulus cases to minimize operator-dependent variability. A 1–2-week follow-up interval was employed to capture dynamic changes across gestational ages, minimizing the impact of timing variability.
The diagnosis of fetal intestinal volvulus was established based on the identification of the whirlpool sign, a spiral-shaped mass of dilated bowel loops observed on two-dimensional (2D) ultrasound [8]. The vascular spiral sign, characterized by the mesenteric vein swirling around the mesenteric artery on 2D and three-dimensional (3D) color Doppler imaging, served as a direct diagnostic indicator [12]. Secondary findings, including ascites, meconium peritonitis, and coffee bean sign, were evaluated to confirm the diagnosis [9].
Patients diagnosed with volvulus underwent ultrasound examinations every 1–2 weeks to monitor disease progression, given the potential for rapid deterioration into complications, such as necrosis or perforation [7]. This interval was chosen to balance the timely detection of dynamic changes, while minimizing the maternal burden. Each follow-up assessment evaluated key ultrasonographic features, including the whirlpool sign, vascular spiral sign, coffee bean sign, intestinal peristalsis, and ascites. Outcomes were correlated with postnatal surgical or autopsy findings to evaluate the diagnostic and prognostic utility of prenatal ultrasound [13, 14].
Seven fetuses were diagnosed with intestinal volvulus without malrotation via prenatal ultrasound at the Women and Children’s Hospital, School of Medicine, Xiamen University, between July 2021 and December 2024. All diagnoses were confirmed based on postnatal surgical or autopsy findings, ensuring diagnostic accuracy and reliability. Maternal age ranged from 24 to 34 years, with initial ultrasound diagnoses made between 23 and 33 weeks of gestation (Table 1). A total of 27 ultrasound examinations were performed, with follow-up assessments conducted every 1–2 weeks to monitor disease progression, as justified by the potential for rapid deterioration [7]. All examinations utilized the GE Voluson E8 or E10 systems, with a standardized protocol and validation by a chief physician to minimize operator-dependent variability and information bias.
| Case no. | GA at diagnosis | Whirlpool sign | Coffee bean sign | Bowel dilation | Vascular spiral sign | Meconium peritonitis | Hydramnios |
| 1 | 32 w, 1 d | Yes | No | Yes | Yes | Yes | No |
| 2 | 25 w, 4 d | Yes | Yes | Yes | Yes | Yes | Yes |
| 3 | 28 w, 0 d | Yes | No | Yes | Yes | Yes | No |
| 4 | 23 w, 3 d | Yes | No | Yes | Yes | No | No |
| 5 | 23 w, 4 d | Yes | No | Yes | Yes | Yes | No |
| 6 | 33 w, 6 d | Yes | No | Yes | Yes | Yes | No |
| 7 | 25 w, 3 d | Yes | Yes | Yes | Yes | Yes | No |
Note: GA, gestational age; w, weeks; d, days.
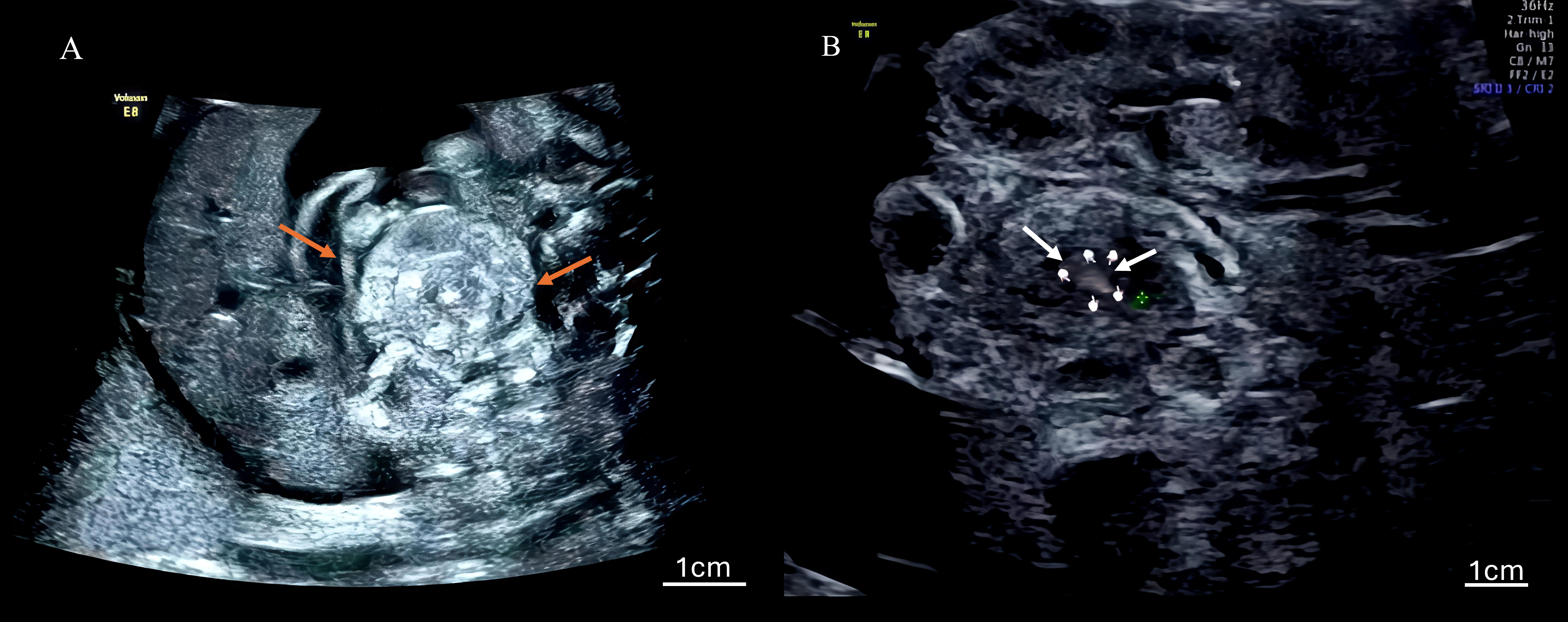
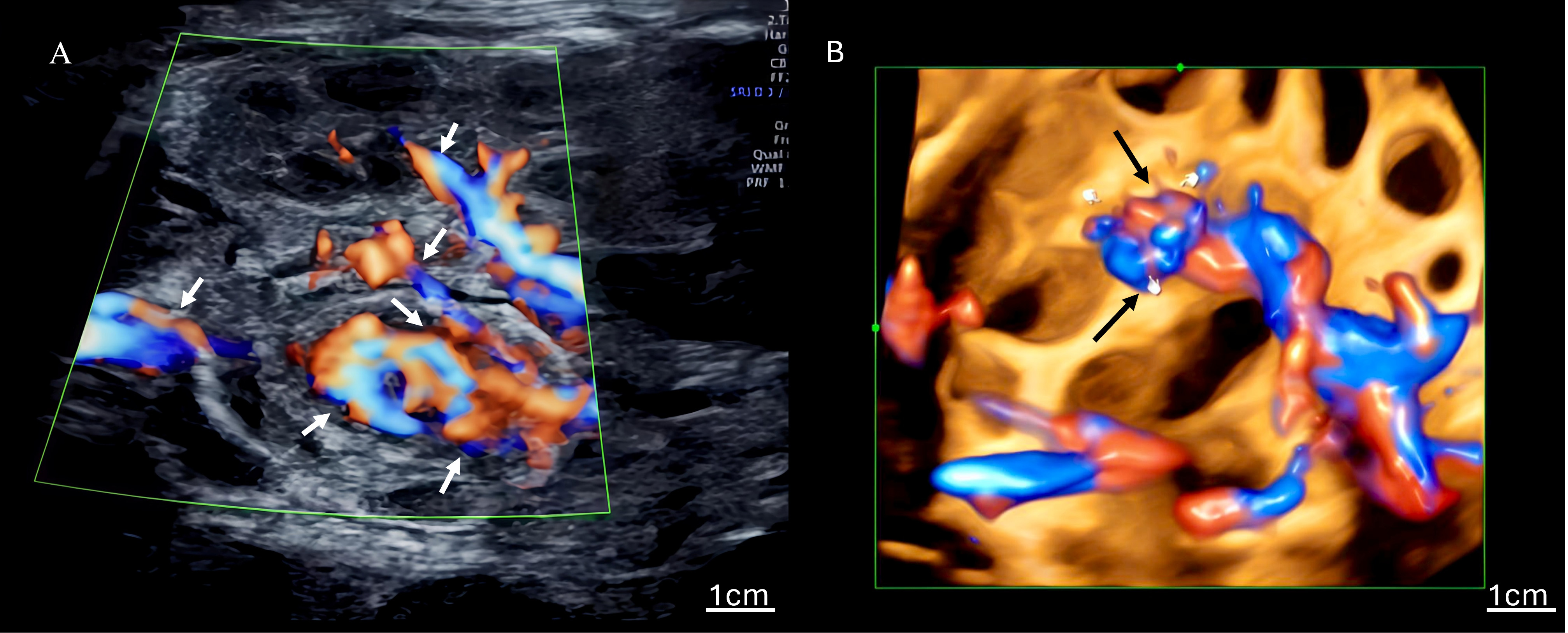
The ultrasonographic findings for all seven cases are summarized in Table 1, which details the gestational age at diagnosis and the presence of key signs. Table 2 quantifies the frequency of findings across all 27 examinations. Characteristic signs included the whirlpool sign (Fig. 1), annotated with arrows to highlight the spiral-shaped mass of dilated bowel loops), a spiral-shaped mass of dilated bowel loops, and the vascular spiral sign (Fig. 2A: 2D ultrasound; Fig. 2B: 3D ultrasound, with arrows indicating the mesenteric vein swirling around the mesenteric artery), observed in all cases (7/7). Nonspecific findings included bowel dilation (7/7), ascites (6/7), abdominal pseudocysts (2/7), coffee bean sign (2/7), hydramnios (1/7), and increased middle cerebral artery flow velocity (1/7). Among the 27 examinations, the detection rates were as follows: whirlpool sign, 20/27 (74.1%); vascular spiral sign, 20/27 (74.1%); bowel dilation, 23/27 (85.2%); ascites, 18/27 (66.7%); cystic abdominal masses, 5/27 (18.5%); coffee bean sign, 2/27 (7.4%); hydramnios, 3/27 (11.1%). Detailed case descriptions are provided below:
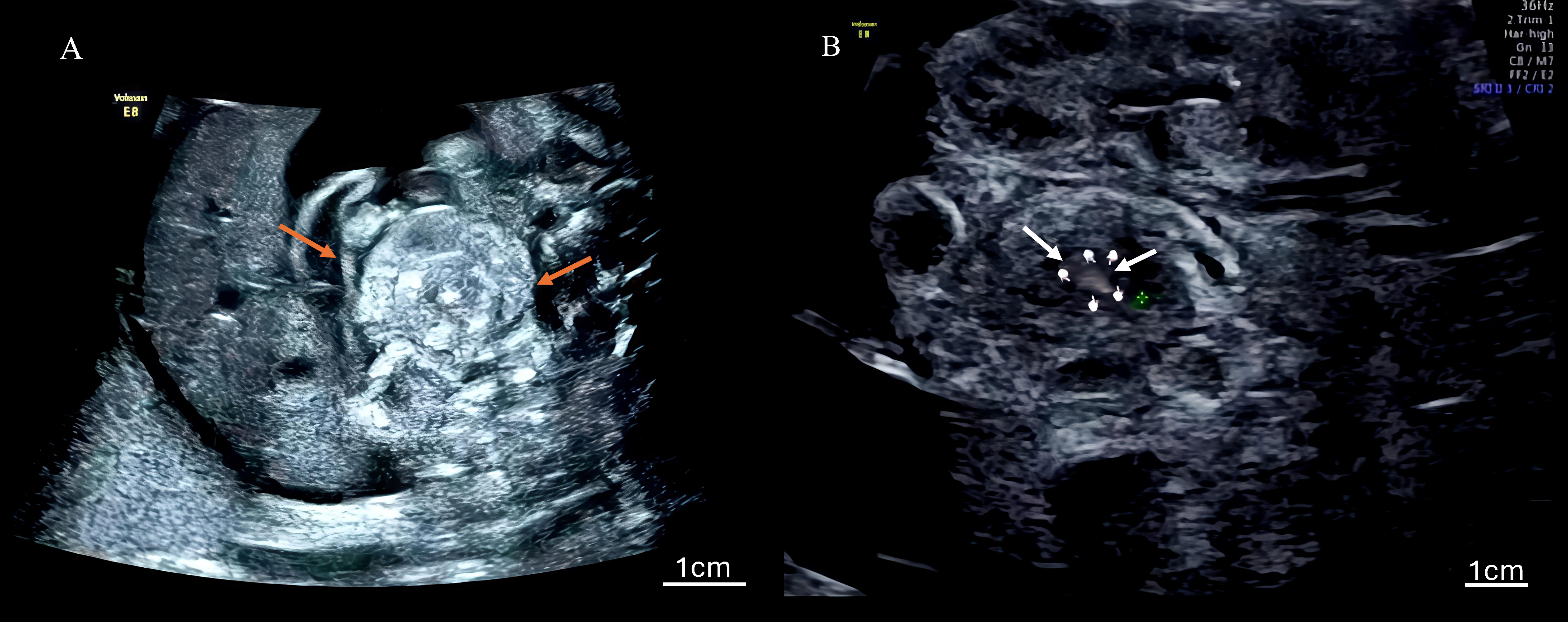 Fig. 1.
Fig. 1. Two-dimensional ultrasound image of the whirlpool sign. (A, B) Images characterized by a spiral-shaped mass of dilated bowel loops, observed in all seven cases of fetal intestinal volvulus, confirming the diagnostic reliability of this technique. Arrows indicate the spiral configuration of the dilated bowel loops, and a scale bar is included for spatial reference. The little finger indicates the center of the whirlpool sign.
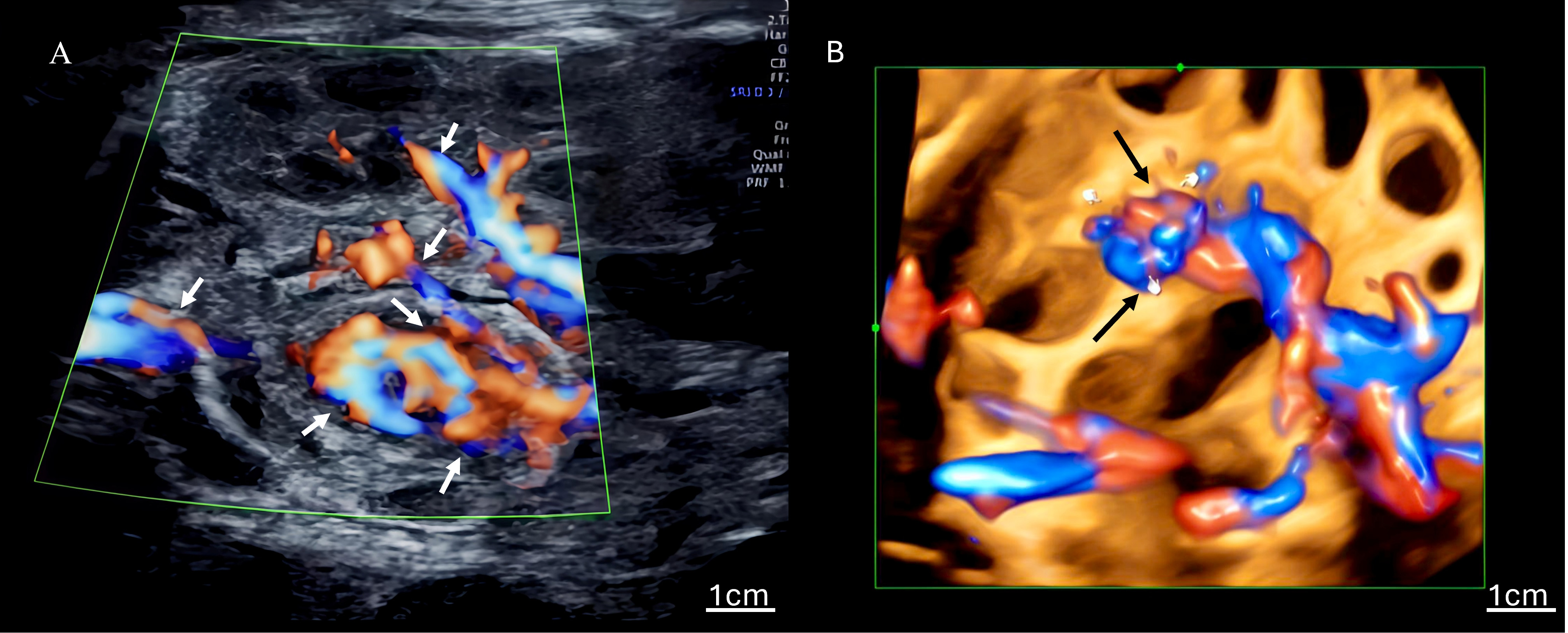 Fig. 2.
Fig. 2. Ultrasound images of the vascular spiral sign. (A) Two-dimensional color Doppler ultrasound of the vascular spiral sign, with the mesenteric vein swirling around the mesenteric artery, a direct indicator of volvulus; arrows highlight the swirling mesenteric vein, and a scale bar is included. (B) Three-dimensional power Doppler ultrasound enhances the visualization of the vascular spiral sign, observed in all cases. Arrows indicate the vascular spiral pattern, with a scale bar provided for reference. The little finger indicates the center of the whirlpool sign.
| Case no. | No. of examinations | Whirlpool sign | Vascular spiral sign | Bowel dilation | Coffee bean sign | Ascites | Abdominal pseudocysts | Hydramnios |
| 1 | 4 | 4/4 | 4/4 | 4/4 | 0/4 | 3/4 | 0/4 | 0/4 |
| 2 | 5 | 4/5 | 4/5 | 5/5 | 2/5 | 4/5 | 0/5 | 3/5 |
| 3 | 4 | 3/4 | 3/4 | 4/4 | 0/4 | 3/4 | 0/4 | 0/4 |
| 4 | 3 | 3/3 | 3/3 | 3/3 | 0/3 | 0/3 | 0/3 | 0/3 |
| 5 | 5 | 3/5 | 3/5 | 4/5 | 0/5 | 4/5 | 2/5 | 0/5 |
| 6 | 3 | 3/3 | 3/3 | 3/3 | 0/3 | 2/3 | 0/3 | 0/3 |
| 7 | 3 | 3/3 | 3/3 | 3/3 | 2/3 | 3/3 | 3/3 | 0/3 |
| Total | 27 | 23/27 (85.2%) | 23/27 (85.2%) | 26/27 (96.2%) | 4/27 (14.8%) | 18/27 (66.7%) | 5/27 (18.5%) | 3/27 (11.1%) |
The clinical outcomes, summarized in Table 3, varied according to the severity of the complications observed on ultrasound. Six fetuses were born alive (five preterm, 26–37 weeks), and five underwent successful resection of the necrotic bowel and enterostomy, achieving favorable outcomes (cases 1, 2, 3, 5, and 6). One neonate (case 7) died post-surgery due to complications from intestinal perforation, which was predicted by prenatal findings of ascites, the coffee bean sign, and loss of peristalsis (Tables 1,2). The presence of ascites (6/7 cases) and the coffee bean sign (2/7) were associated with severe complications, including necrosis and perforation. In contrast, bowel dilation (7/7) was a consistent early indicator, prompting further investigation (Table 1). Intestinal atresia, observed in five cases (four type III), correlated with more extensive surgical interventions and prolonged recovery (Table 2). All cases lacked intestinal malrotation, confirmed by surgical or autopsy findings, distinguishing this cohort from typical volvulus presentations.
| Case no. | GA at delivery | Mode of delivery | Birth weight (g) | Outcome | Surgical or pathological findings |
| 1 | 34 w, 0 d | Cesarean | 2190 | Cure | Volvulus, type III atresia, necrosis, meconium peritonitis |
| 2 | 34 w, 4 d | Vaginal | 2100 | Cure | Volvulus, type III atresia, necrosis, meconium peritonitis |
| 3 | 31 w, 2 d | Vaginal | 2000 | Cure | Volvulus, necrosis, meconium peritonitis |
| 4 | 26 w, 0 d | Vaginal (TOP) | 750 | TOP | Volvulus, necrosis (autopsy) |
| 5 | 36 w, 6 d | Vaginal | 2970 | Cure | Volvulus, type III atresia, necrosis, meconium peritonitis |
| 6 | 37 w, 2 d | Vaginal | 2550 | Cure | Volvulus, type III atresia, necrosis |
| 7 | 33 w, 4 d | Vaginal | 3069 | Death | Volvulus, type III atresia, necrosis, meconium peritonitis, perforation |
Note: TOP, termination of pregnancy.
All seven pregnant women had low-risk results in the Down syndrome screening (Tang screen) with normal nuchal translucency measurements. Noninvasive prenatal testing (NIPT) indicated low risk for chromosomal abnormalities. Cordocentesis in cases 4 and 5 revealed no significant karyotype abnormalities, although copy number variation sequencing (CNV-seq) identified variants of uncertain clinical significance (case 4: 293.83 kb duplication on chromosome 5; case 5: 142.07 kb deletion in 13q21.31q21.31). No medications were prescribed during pregnancy.
This case series presents the prenatal ultrasonographic characteristics and clinical outcomes of seven fetuses diagnosed with intestinal volvulus in the absence of malrotation, a rare and potentially catastrophic condition that poses significant diagnostic and therapeutic challenges. Consistent detection of the whirlpool sign, characterized by a spiral configuration of dilated bowel loops, and the vascular spiral sign, defined by the mesenteric vein encircling the mesenteric artery on Doppler imaging, across all cases underscores the pivotal role of these characteristics as diagnostic hallmarks, corroborating prior observations in the literature [4, 5, 7]. These findings, detailed in the Results section (Tables 1,3; Figs. 1,2), were observed in 74.1% of the 27 ultrasound examinations, affirming the reliability of these diagnostic hallmarks in identifying volvulus without malrotation, a subset of cases less frequently reported than those associated with rotational anomalies [4]. Unlike traditional presentations of volvulus, which often manifest with aberrant positioning of the superior mesenteric vessels due to malrotation, the absence of malrotation in our cohort, confirmed by surgical or autopsy findings, suggests alternative etiological pathways, potentially driven by mechanical torsion of the mesentery, independent of developmental rotation defects.
The absence of malrotation in our cohort suggests that alternative mechanisms, such as localized ischemia or abnormal mesenteric fixation, may contribute to the development of volvulus. Localized ischemia, potentially resulting from transient vascular insults in utero, could induce mesenteric torsion, leading to volvulus independent of rotational anomalies. Similarly, inadequate mesenteric fixation may allow excessive mobility of the bowel, predisposing the bowel to twisting and subsequent obstruction, as supported by recent case reports [8, 16]. This hypothesis warrants further investigation to elucidate the precise etiological pathways underlying this rare anomaly, which may inform targeted diagnostic and therapeutic strategies.
The diagnostic utility of prenatal ultrasound in this context cannot be overstated, as this modality facilitates the early identification of a condition prone to rapid progression toward severe complications, including intestinal necrosis, atresia, perforation, and meconium peritonitis. The universal presence of bowel dilation (85.2% of examinations) served as an early indicator of detailed ultrasonographic scrutiny, while ascites (66.7%) and the coffee bean sign (7.4%) emerged as critical markers of advanced pathology, such as strangulated obstruction or perforation, as evidenced in cases 2 and 7 (Table 3). The prenatal detection of the coffee bean sign, observed in two cases, is a critical indicator of strangulated obstruction, underscoring the need for urgent multidisciplinary perinatal collaboration to expedite delivery and surgical management, thereby mitigating the risk of irreversible complications such as perforation [9]. These findings align with recent studies emphasizing the specificity of the whirlpool sign in detecting volvulus and the prognostic significance of secondary signs, such as ascites and pseudocysts [9]. Meanwhile, compared to magnetic resonance imaging (MRI), which offers enhanced anatomical resolution but is constrained by cost and limited dynamic assessment, ultrasound real-time visualization of bowel dynamics and vascular patterns renders this imaging platform the modality of choice for routine prenatal monitoring. The high sensitivity of the whirlpool and vascular spiral signs in our cohort (100% case detection) advocates for their integration into standardized obstetric ultrasound protocols, particularly when bowel dilation is detected, to expedite diagnosis and mitigate adverse outcomes [8, 9, 17].
The prognostic implications of our findings are profound because the severity of ultrasonographic abnormalities is closely correlated with postnatal outcomes. All seven cases exhibited intestinal necrosis, with five complicated by intestinal atresia (four type III), a severe form associated with significant bowel loss and protracted recovery [18]. The presence of ascites and the coffee bean sign observed in cases with the most severe complications, such as perforation in case 7, which resulted in neonatal demise, underscores their utility as predictors of poor prognosis. These observations align with larger case series, such as those reported by Taşdemir et al. [10] and Montironi et al. [1], which highlight the prognostic heterogeneity of fetal volvulus and the critical role of early diagnosis in optimizing surgical planning. The timely identification of volvulus in our cohort enabled successful resection and enterostomy in five of six live births, demonstrating the clinical impact of prenatal ultrasound in facilitating prompt postnatal intervention. However, the neonatal death in case 7, predicted by worsening ascites and loss of peristalsis, illustrates the limitations of the current management strategies in mitigating the consequences of advanced pathology, emphasizing the need for refined therapeutic approaches.
The absence of malrotation in our cases challenges conventional paradigms that associate volvulus with rotational anomalies, suggesting that mechanical factors such as mesenteric torsion or localized ischemia may precipitate volvulus in otherwise normally rotated intestines. This hypothesis is supported by previous reports of volvulus without malrotation, which propose that intrauterine events, such as transient obstructions or vascular insults, may trigger torsion [8]. The high incidence of intestinal atresia in our cohort (71.4%) further suggests a mechanistic link wherein volvulus-induced ischemia impairs bowel development, leading to atresia as a secondary consequence [16, 18]. This interplay between volvulus and atresia warrants further investigation as the interaction may inform prenatal risk stratification and surgical planning. Additionally, the genetic analyses in cases 4 and 5, which identified variants of uncertain significance, revealed no definitive association with volvulus, consistent with the paucity of evidence in the literature linking this condition to specific genetic aberrations [4]. Thus, routine genetic testing in isolated cases of volvulus may be of limited utility, although larger studies are required to clarify this.
Despite the contributions of this study, limitations exist, including the small sample size of seven cases, which reflects the rarity of fetal intestinal volvulus without malrotation, with an estimated incidence of related conditions of approximately 1 in 6000 [12, 17, 19, 20]. This limitation, acknowledged as acceptable given the rarity of the condition, underscores the value of case series in elucidating rare anomalies [12, 17, 19, 20]. The single-center retrospective design may introduce information bias, although this was mitigated by employing a standardized ultrasound protocol, expert validation, and corroboration of postnatal findings. The variability in detection rates of the whirlpool and vascular spiral signs (74.1% across examinations) may reflect the dynamic nature of volvulus, wherein prolonged ischemia leads to necrosis and adhesion, obscuring these signs, as noted in prior studies [15]. Nevertheless, our detailed ultrasonographic and clinical characterization provides a robust foundation for future research, particularly in the context of this rare entity. Multicenter studies with larger cohorts are imperative to validate our findings, refine the diagnostic criteria, and explore the genetic and environmental factors contributing to volvulus without malrotation. Additionally, the development of advanced imaging techniques, such as high-resolution Doppler or fetal MRI, may enhance diagnostic precision and prognostic accuracy, further improving the clinical outcomes.
In summary, this study underscores the instrumental role of prenatal ultrasound in the early diagnosis and management of fetal intestinal volvulus without malrotation, with whirlpool and vascular spiral signs serving as reliable diagnostic markers. The correlation between ultrasonographic findings and prognostic outcomes highlights the importance of vigilant monitoring and timely intervention to mitigate severe complications. By elucidating the characteristics of a rare condition, our findings contribute to the evolving landscape of prenatal diagnostics, paving the way for enhanced counseling and therapeutic strategies to optimize fetal and neonatal outcomes.
This investigation elucidates the pivotal role of prenatal ultrasound in the early and precise diagnosis of fetal intestinal volvulus without malrotation, which is a rare yet potentially life-threatening condition. The consistent identification of the whirlpool and vascular spiral signs across all seven cases, as detailed in the results, underscores their diagnostic reliability, enabling timely detection in the absence of malrotation. Prenatal ultrasound, through the identification of these characteristic signs, provides a critical foundation for timely intervention decisions, facilitating multidisciplinary perinatal collaboration and improving neonatal outcomes by expediting postnatal surgical management. Nonspecific ultrasonographic findings, such as bowel dilation and ascites, further corroborate the diagnosis, whereas the presence of ascites and the coffee bean sign serve as critical predictors of severe complications, including necrosis and intestinal atresia, which were prevalent in our cohort. Specific findings, such as the coffee bean sign, underscore the importance of multidisciplinary collaboration in perinatal care to optimize outcomes for high-risk cases. These findings facilitated informed prenatal counseling and expedited postnatal surgical intervention, resulting in favorable outcomes in five of six live births. The high incidence of type III atresia (four of five cases with atresia) highlights the prognostic significance of early diagnosis, as delayed intervention may exacerbate adverse outcomes, as evidenced by the neonatal death in case 7. Despite the inherent limitations of a small, single-center cohort, this study provides a robust foundation for understanding the ultrasonographic and clinical profiles of this rare entity, contributing valuable insights to the limited literature. Future multicenter studies are imperative to validate these findings and refine the diagnostic protocols, potentially incorporating advanced imaging modalities to enhance precision. By delineating the diagnostic and prognostic utility of prenatal ultrasound, this study advances the paradigm of fetal medicine, fostering improved prenatal management and optimized neonatal outcomes for fetal intestinal volvulus without malrotation.
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request, subject to institutional data-protection policies.
SZ and XH contributed equally to this work by performing ultrasound examinations, data collection, and drafting the initial manuscript. ML and JZ conducted the data analysis and interpretation, contributing to the methodology and results sections of the manuscript. XZ contributed to data visualization and literature review. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work
This study was approved by the Institutional Ethics Committee of the Women and Children’s Hospital, School of Medicine, Xiamen University (Approval No. KY-2024-079-K01). Written informed consent was obtained from all participants prior to their inclusion in the study in accordance with the Declaration of Helsinki.
We express our profound gratitude to the clinical staff of the Department of Ultrasound and the Department of Pediatric Surgery at the Women and Children’s Hospital, School of Medicine, Xiamen University, for their invaluable contribution to the execution of ultrasound examinations and postnatal surgical interventions. We also extend our sincere appreciation to the participating families for their cooperation, which facilitated this research. The institutional support provided by Women and Children’s Hospital was pivotal in enabling the successful completion of this study.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.