1 Department of Family Medicine, Faculty of Medicine, King Abdulaziz University, 21589 Jeddah, Saudi Arabia
2 Famile Medicine Residency Program, King Abdulaziz University Hospital, 21589 Jeddah, Saudi Arabia
Abstract
The menopausal phase represents a pivotal transition in a woman’s reproductive life, characterized by a wide spectrum of somatic, psychological, and urogenital symptoms. Research indicates that, despite the severity of these symptoms, women encounter multiple barriers when seeking medical care. This study aims to assess the prevalence and severity of menopausal symptoms among women in Saudi Arabia, as well as the barriers to seeking medical consultation for their management.
A cross-sectional study was conducted in 2024 among 430 perimenopausal and postmenopausal women in Saudi Arabia using a self-administered online questionnaire. Data were collected on demographics, menopausal symptom severity using the menopause rating scale (MRS), and barriers to seeking medical advice. Statistical analyses were performed using SPSS version 27.
The mean MRS score was 17.28 ± 9.43, with 52.5% of participants reporting severe to very severe symptoms. Physical and mental exhaustion was the most prevalent symptom (84.9%), while the belief that menopausal symptoms are a natural part of aging was the most frequently reported barrier to seeking medical advice (45.1%). Severe to very severe menopausal symptoms were significantly more common among married participants. In addition, older age, higher educational level, unemployment, and the presence of a chronic disease were identified as risk factors for greater symptom severity.
More than half of the women in this study experienced severe to very severe menopausal symptoms. There is a critical need for enhanced health education to promote strategies for alleviating these symptoms and to emphasize the importance of seeking appropriate medical care.
Keywords
- menopause
- symptom
- severity
- barriers
- Saudi Arabia
The term “menopause” refers to the permanent cessation of menstruation for more than a year owing to a decline in ovarian follicular activity [1]. Menopause usually starts gradually, with symptoms emerging between the ages of 47 and 55 years, marking a significant transition in a woman’s reproductive lifecycle [2]. Estimates suggest that by 2030, the global count of postmenopausal women will exceed 1.2 billion [3]. With the aging global population and increasing life expectancy, women are now spending a considerable portion of their lives, approximately one-third, in the postmenopausal phase [1].
Menopausal syndrome encompasses a wide range of symptoms, from physiological to psychological manifestations [4]. These include vasomotor symptoms such as hot flashes and night sweats, emotional changes such as mood swings and irritability, cognitive challenges including concentration difficulties and mental confusion, and various urogenital symptoms, such as stress incontinence and vaginal dryness [4, 5]. Women may also be more susceptible to headaches, sleep disorders such as insomnia, and osteoporotic symptoms [4]. Physical symptoms include exhaustion, reduced skin elasticity, and incontinence, while psychological symptoms may involve sadness, low self-esteem, memory loss, anxiety, and panic attacks [5]. These symptoms, which fall into four categories, namely, vasomotor, physical, emotional, and sexual, usually start during the perimenopausal stage [5]. Each category has a significant impact on daily functioning and overall quality of life of women undergoing this transition [6].
The majority of women experience vasomotor symptoms, which are often considered a hallmark of menopause [7]. Approximately 75% of women describe their menopausal experiences as moderately to severely challenging in the workplace [7]. These factors, which vary widely among women worldwide, show a great deal of heterogeneity among women, highlighting the complexity and diversity of menopausal experiences [8]. Furthermore, 44% of women reported taking sick leave without revealing that their absence was caused by menopausal symptoms [7].
The incidence of menopausal symptoms among postmenopausal women varies based on several factors, including lifestyle choices, psychological situations, cultural influences, and sociodemographic features [8, 9]. The severity and frequency of these symptoms are not uniform across different countries and can also vary within the same population [10]. A systematic review of published data revealed significant variations in the prevalence of menopausal symptoms, with rates ranging from 22% to 63% in Asia, 36% to 50% in North America, and up to 74% in European populations [11].
Research conducted in different regions of Saudi Arabia has yielded varying results regarding the severity of menopausal symptoms, as measured by the menopause rating scale (MRS). The average MRS score in Riyadh indicated that most symptoms were mild (MRS
A study conducted in the United Kingdom found that more than 80% of women experience some combination of menopausal symptoms [7]. Despite the availability of effective treatments, such as hormone replacement therapy (HRT), which can alleviate menopausal symptoms and improve quality of life [13, 14], only 54% of women actively seek medical treatment for disorders associated with estrogen insufficiency during menopause [7].
In many societies, menopause is rarely discussed, leading to lower levels of awareness and understanding among women experiencing it. This lack of dialogue can contribute to stigma, misinformation, and reluctance to seek medical advice or treatment [15]. Despite these challenges, little research has explored the obstacles to obtaining medical help for menopausal symptoms. This study aims to investigate the frequency and intensity of menopausal symptoms, as well as the obstacles Saudi Arabian menopausal women face while seeking medical help. By considering the unique cultural and social context, this study aims to provide important insights into how menopausal symptoms are experienced and handled within this community.
A cross-sectional analytic study was conducted in Saudi Arabia from February to December 2024.
The study included women in Saudi Arabia aged 45 to 65 years who had reached menopause, defined as 12 months of amenorrhea, or who were experiencing perimenopausal menstrual irregularities. Women currently using hormonal therapy or those with serious medical conditions that could considerably affect the evaluation of menopausal symptoms, such as advanced-stage cancer or severe psychiatric disorders, were excluded from the study.
Participants completed a self-administered questionnaire hosted on Google Forms. The questionnaire was distributed through social media channels, particularly WhatsApp Messenger, to reach the target population. To select participants, a snowball sampling method was employed, where initial participants were invited to share the questionnaire within their networks, allowing the study to expand and ultimately reach the broader study population.
The questionnaire consisted of three sections: the first section gathered sociodemographic information, including age, nationality, residence, marital status, education level, income, job, parity, menstrual status, and history of chronic disease. The second section assessed the severity of menopausal symptoms using the Arabic version of a previously validated scale: the MRS [16, 17]. The MRS consists of 11 symptoms categorized into three domains: somatic, psychological, and urogenital. Each symptom is scored on a scale from 0 (none) to 4 (very severe), yielding a total score ranging from 0 to 44. Symptom severity was classified as follows: none/little (0–4), mild (5–8), moderate (9–16), and severe/very severe (17+). The last section of the survey examined barriers to seeking medical advice, such as cultural beliefs, societal stigma, financial constraints, perceived efficacy of treatments, awareness about menopausal health, and access to healthcare services. A pilot study was conducted with 20 participants to assess the reliability of the questionnaire. The Cronbach’s alpha value was estimated to be 0.884, indicating strong internal consistency. The scale is considered internally consistent when Cronbach’s alpha value is greater than 0.7 [18].
The target population in this age group was 1,228,385, based on demographic data from the Saudi General Authority for Statistics for the year 2022. The sample size was determined using the Raosoft calculator [15], assuming a 50% response distribution, a 5% margin of error, and a 95% confidence level. The calculator suggested a sample size of approximately 385 participants, ensuring statistically significant results.
Data were analyzed using the Statistical Package for Social Sciences, version 27 (IBM Corp., Armonk, NY, USA). Qualitative data were expressed as numbers and percentages, while quantitative variables were expressed as mean and standard deviation (mean
The present study included 430 participants, the majority of whom (94.0%) were Saudi nationals, 43.5% were residents of the Western region of Saudi Arabia, and 71.2% were married. The remaining demographic variables are presented in Table 1.
| N | % | ||
| Age (years) | |||
| 45–49 | 138 | 32.1% | |
| 50–54 | 162 | 37.7% | |
| 55–60 | 108 | 25.1% | |
| 61–65 | 22 | 5.1% | |
| Nationality | |||
| Saudi | 404 | 94.0% | |
| Non-Saudi | 26 | 6.0% | |
| Residence | |||
| Central region | 62 | 14.4% | |
| Western region | 187 | 43.5% | |
| Eastern region | 60 | 14.0% | |
| Southern region | 66 | 15.3% | |
| Northern region | 55 | 12.8% | |
| Marital status | |||
| Single | 25 | 5.8% | |
| Married | 306 | 71.2% | |
| Divorced | 61 | 14.2% | |
| Widowed | 38 | 8.8% | |
| Education level | |||
| School (Primary, middle, or high school) | 71 | 16.5% | |
| Diploma | 71 | 16.5% | |
| Bachelor’s (University or College) | 252 | 58.6% | |
| Master’s or PhD | 36 | 8.4% | |
| Occupation | |||
| Not working | 164 | 38.1% | |
| Working | 266 | 61.9% | |
| Socioeconomic status | |||
| Low | 23 | 5.4% | |
| Middle | 330 | 76.7% | |
| High | 77 | 17.9% | |
| Have you ever been pregnant and given birth | |||
| No | 86 | 20.0% | |
| Yes | 344 | 80.0% | |
| Describe menstrual regularity in the past 12 months | |||
| Irregular | 245 | 57.0% | |
| Stopped | 185 | 43.0% | |
| Lifestyle factors | |||
| Non-smoker | 361 | 84.0% | |
| Current smoker | 52 | 12.0% | |
| Ex-smoker | 17 | 4.0% | |
| Do you have a chronic disease? | |||
| No | 338 | 78.6% | |
| Yes | 92 | 21.4% | |
| Have you sought medical advice for menopausal symptoms? | |||
| No | 285 | 66.3% | |
| Yes | 113 | 26.3% | |
| Never had symptoms | 32 | 7.4% | |
Fig. 1 illustrates severity of menopausal symptoms among participants according to MRS. The mean total MRS score was 17.28
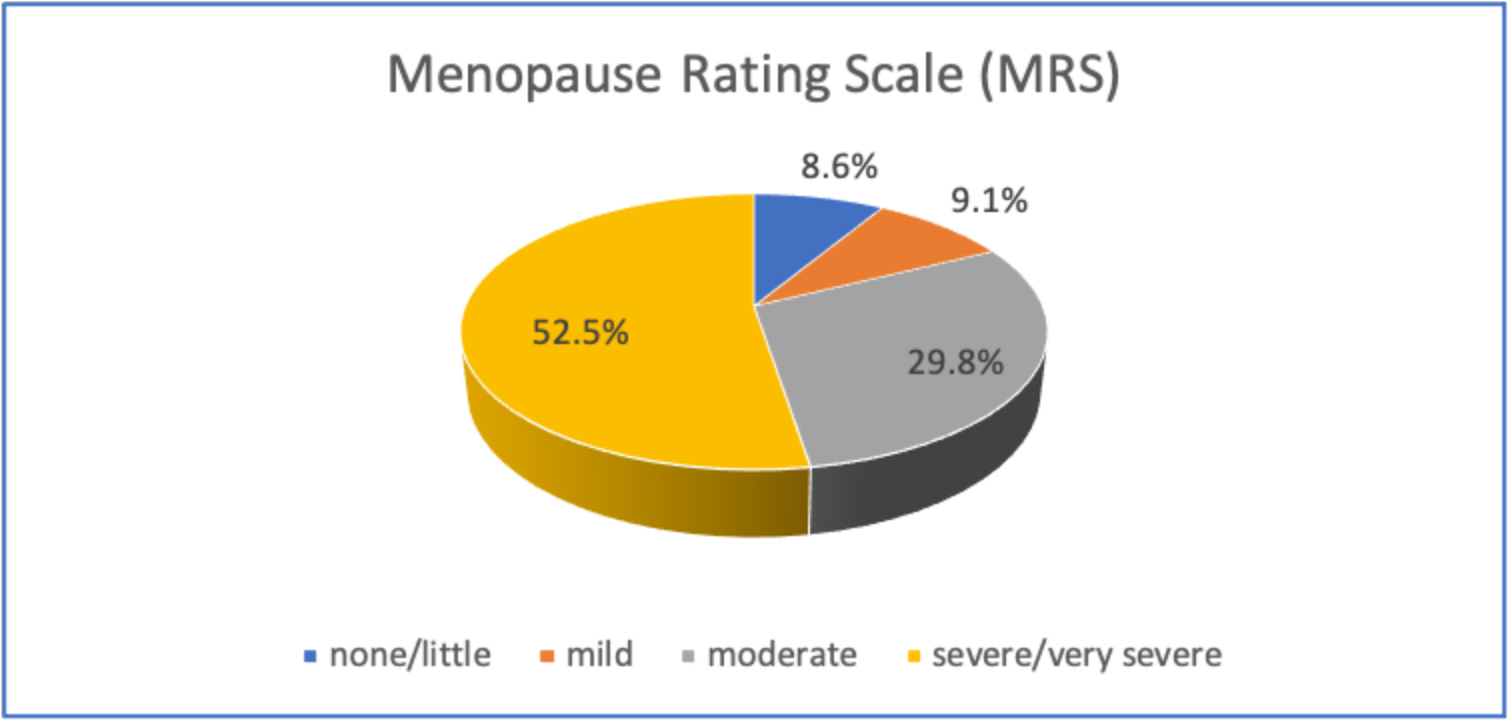 Fig. 1.
Fig. 1. Severity of menopausal symptoms among women according to MRS: 226 (52.5%) described severe to very severe symptoms, 128 (29.8%) moderate symptoms, 39 (9.1%) mild symptoms, and 37 (8.6%) had no or little symptoms. MRS, menopause rating scale.
The prevalence and severity of menopausal symptoms are presented in Table 2. The most prevalent symptom was physical and mental exhaustion, affecting 84.9% of the participants, with 31.0% classified as experiencing severe to very severe symptoms. The second most frequent symptom was joint and muscular discomfort, reported by 80.7% of participants, of whom 31.2% had severe to very severe symptoms. Sleeping problems were the third most common symptom, affecting 79.5% of the participants, closely followed by depressive mood, reported by 79.2% of the participants, then hot flashes in 78.8% of participants.
| None | Mild | Moderate | Severe/very severe | ||||||
| n | % | n | % | n | % | n | % | ||
| Somatic symptoms | |||||||||
| Sleep problems (difficulty falling asleep, difficulty sleeping through, waking up early) | 88 | 20.5% | 104 | 24.2% | 113 | 26.3% | 125 | 29.0% | |
| Joint and muscular discomfort (pain in joints, rheumatoid complaints) | 83 | 19.3% | 105 | 24.4% | 108 | 25.1% | 134 | 31.2% | |
| Hot flashes, sweating (episodes of sweating) | 91 | 21.2% | 112 | 26.0% | 120 | 27.9% | 107 | 24.9% | |
| Heart discomfort (unusual heartbeat, heart skipping, heart racing, and tightness) | 112 | 26.0% | 127 | 29.5% | 92 | 21.4% | 99 | 23.0% | |
| Psychological symptoms | |||||||||
| Physical and mental exhaustion (decreased performance, impaired memory, decreased concentration, forgetfulness) | 65 | 15.1% | 130 | 30.2% | 102 | 23.7% | 133 | 31.0% | |
| Anxiety (inner restlessness, feeling panicky) | 109 | 25.3% | 127 | 29.5% | 89 | 20.7% | 105 | 24.5% | |
| Depressive mood (feeling down, sad, on the verge of tears, lack of drive, mood swings) | 89 | 20.7% | 112 | 26.0% | 121 | 28.1% | 108 | 25.1% | |
| Irritability (feeling nervous, tense, or aggressive) | 108 | 25.1% | 132 | 30.7% | 84 | 19.5% | 106 | 24.7% | |
| Urogenital symptoms | |||||||||
| Sexual problems (change in sexual desire, sexual activity, and satisfaction) | 140 | 32.6% | 91 | 21.2% | 98 | 22.8% | 101 | 23.5% | |
| Bladder problems (difficulty in urinating, increased need to urinate, bladder incontinence) | 145 | 33.7% | 113 | 26.3% | 88 | 20.5% | 84 | 19.6% | |
| Vaginal dryness (sensation of dryness or burning in the vagina, difficulty during sexual intercourse) | 163 | 37.9% | 104 | 24.2% | 78 | 18.1% | 85 | 19.8% | |
Fig. 2 demonstrates the barriers preventing women from seeking medical advice for menopausal symptoms. Among the participants, 45.1% believed that menopausal symptoms are a natural part of aging and do not require medical attention, 35.1% cited a lack of time or other personal commitments, and 30.9% reported difficulties in scheduling appointments or long wait times. The remaining barriers are described in the figure.
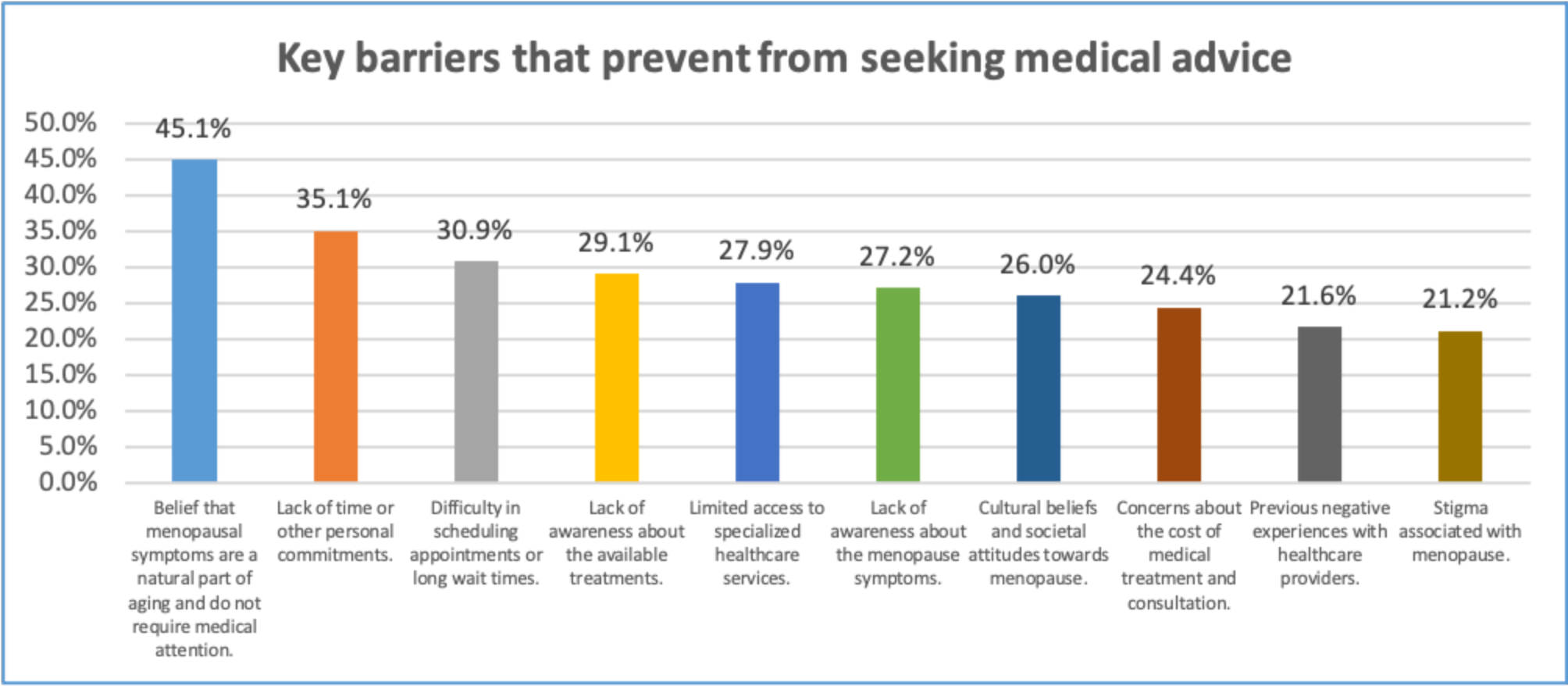 Fig. 2.
Fig. 2. Key barriers to seeking medical advice.
Fig. 3 illustrates the influence of cultural norms and societal attitudes on the decision to seek medical help for menopause. A significant proportion of respondents (47.7%) reported that these factors did not influence their choices, while 17.7%, 17.9%, 10.9%, and 5.8% of respondents stated that cultural and societal factors had a slight, moderate, significant, and complete influence, respectively, on their decision.
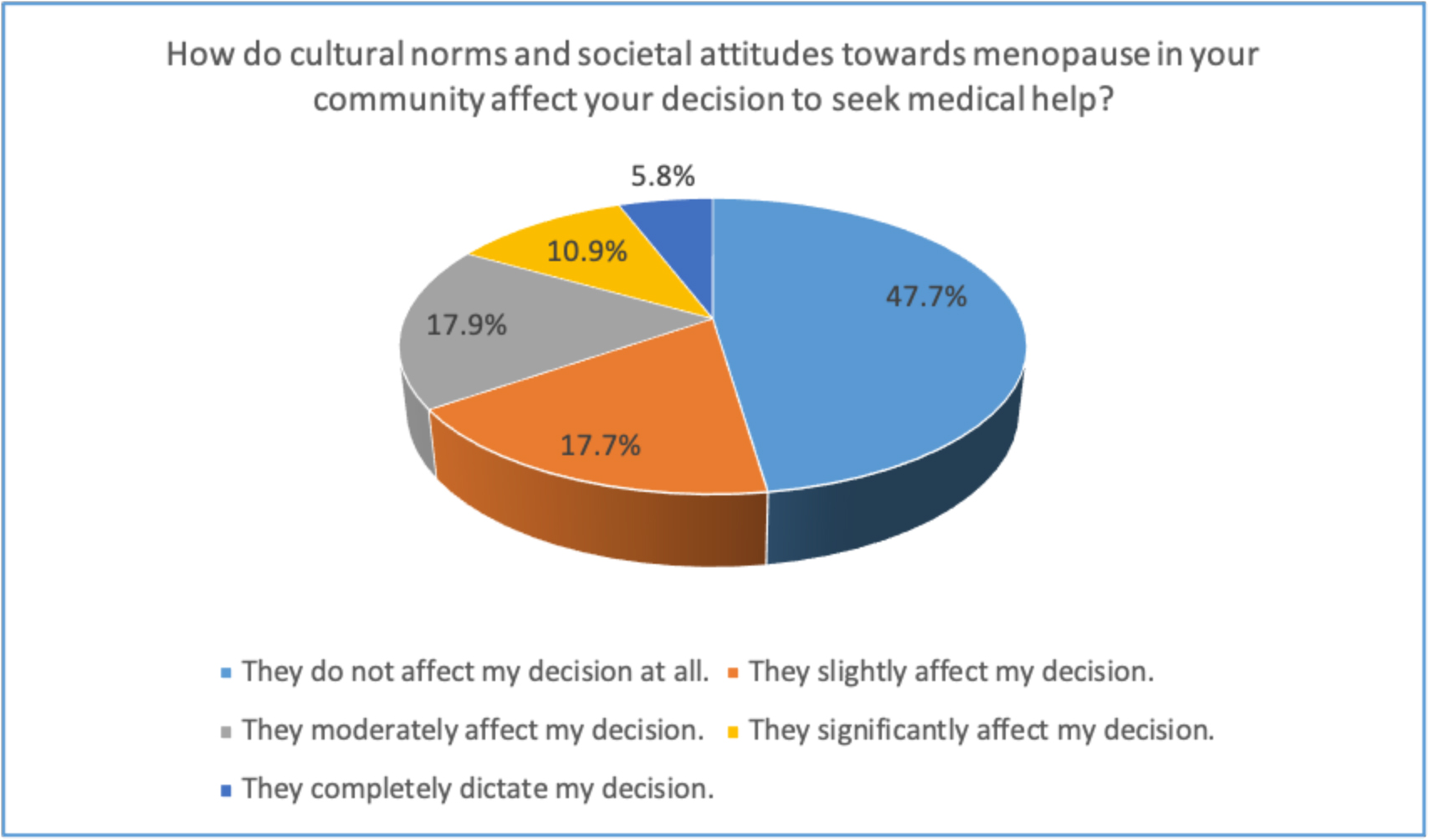 Fig. 3.
Fig. 3. Impact of cultural and societal attitudes toward menopause on the decision to seek medical help.
The study examined the effect of various demographic variables on the MRS. The prevalence of severe or very severe menopausal symptoms was significantly higher among married participants (71.7%) compared to those with other marital statuses; where it was found to be 16.4% among divorced, 10.2% among widowed and 1.8% among single participants (p
Table 3 presents the results of the univariate analysis examining the effects of various predictors on the MRS continuous outcome scale. The findings indicate that age, education level, and the presence of a chronic disease significantly influence MRS severity. Specifically, increasing age and higher educational levels are associated with greater MRS severity, while the presence of a chronic disease further contributes to increased symptom severity.
| B | t | p-value | 95% CI for B | R2 | ||
| Lower bound | Upper bound | |||||
| Age | 2.063 | 4.065 | 1.065 | 3.060 | 0.037 | |
| Education level | 1.327 | 2.525 | 0.012 | 0.294 | 2.360 | 0.015 |
| Occupation | −1.720 | −1.841 | 0.066 | −3.556 | 0.116 | 0.008 |
| Socioeconomic status | 0.393 | 0.402 | 0.688 | −1.529 | 2.316 | 0.000 |
| Have you ever been pregnant and given birth? | 1.052 | 0.925 | 0.355 | −1.184 | 3.288 | 0.002 |
| Do you have a chronic disease? | 4.728 | 4.350 | 2.591 | 6.864 | 0.042 | |
| Have you sought medical advice for your menopausal symptoms? | 1.772 | 1.689 | 0.092 | −0.290 | 3.834 | 0.007 |
B, regression coefficients; CI, confidence interval.
Table 4 shows the assessment of the multiple effects of independent scaled predictors on the MRS continuous outcome scale. Only variables that were significant or near significant were included in the model. The analysis revealed that increasing age, higher educational level, unemployed, and the presence of a chronic disease were independent predictors of greater MRS severity (p
| B | t | p-value | 95% CI for B | R2 | ||
| Lower bound | Upper bound | |||||
| Age | 1.278 | 2.361 | 0.019 | 0.214 | 2.342 | 0.092 |
| Education level | 1.764 | 3.114 | 0.002 | 0.650 | 2.877 | |
| Occupation | −2.184 | −2.152 | 0.032 | −4.180 | −0.189 | |
| Do you have a chronic disease? | 3.901 | 3.447 | 0.001 | 1.676 | 6.126 | |
| Have you sought medical advice for your menopausal symptoms? | 0.719 | 0.698 | 0.486 | −1.306 | 2.744 | |
This study evaluated the severity of menopausal symptoms and the barriers women face when seeking medical advice. Our results indicate a mean MRS score of 17.28
In our study, the most commonly reported symptoms were physical and mental exhaustion (365 participants, 84.9%) and joint and muscular discomfort (347 participants, 80.7%). These findings aligned with previous studies conducted in India and Pakistan [19, 20, 21], which also reported similar findings. The high prevalence of physical and mental exhaustion experienced during menopause can be attributed to hormonal fluctuations during this critical phase in a woman’s life, which often lead to mood changes [9]. Additionally, the high prevalence of joint and muscular discomfort in our sample may be due to the widespread vitamin D deficiency among Saudi women (reported as 60.2% in a recent study [22]), which contributes to joint and muscle pain [22].
The results of our study differed slightly from those of a study conducted in the United Kingdom, where the most predominant symptoms were sleep disturbances (81.8%), followed by hot flashes (80.7%), and memory problems (75.6%) [7]. Similarly, studies conducted in Sri Lanka and Malaysia reported that hot flashes and sweating were the most common symptoms [9]. These differences could be explained by the hot climate in our region, which may reduce women’s sensitivity to the temperature fluctuations caused by hot flashes or lead them to mistake these sensations for the natural heat of the weather [12]. Moreover, racial and ethnic variations, as well as differences in body composition—women in those regions tend to be leaner—may affect the manifestation of menopausal symptoms [9].
The study revealed that married women tend to experience more severe menopausal symptoms, aligning with previous research showing that married women report higher levels of symptoms [23]. This may be because married women are more likely to be sexually active, making them more aware of urogenital symptoms such as dyspareunia and vaginal dryness. However, some studies have presented contrasting findings [24]. These differences may be attributed to various factors, such as the nature of the relationship between partners and the level of supportive care, which could influence the severity of menopausal symptoms [2, 23].
Our study found that several demographic factors significantly influenced the severity of menopausal symptoms, as measured by the MRS. Increasing age, higher educational level, unemployment, and the presence of chronic diseases were all identified as risk factors associated with greater MRS severity. These findings align with previous research suggesting that aging exacerbates menopausal symptoms [10, 25]. The primary explanation for this is the substantial decline in estrogen levels as women age, which contributes to the worsening of menopausal symptoms [10]. The findings also revealed a significant association between a history of a chronic disease and the severity of menopausal symptoms. Middle-aged women with a history of chronic illness are 2.56 times more likely than those without such conditions to develop severe menopausal symptoms [10]. These results are consistent with findings from several previous studies [10, 26]. This observation may be explained by several factors, including hormonal imbalances caused by underlying endocrine dysfunctions such as diabetes and thyroid disorders, medication side effects, and autonomic nervous system dysfunction, all of which can exacerbate vasomotor symptoms. In addition, chronic illness may limit physical activity, which can negatively impact overall health and reduce the body’s ability to manage menopause-related symptoms such as weight gain, mood swings, and sleep disturbances.
Our study suggests that educational level influences the severity of menopausal symptoms. This may be due to the fact that women with higher education are generally more attuned to their health, making them better able to recognize and report their symptoms [21]. This finding aligns with previous research [21, 23, 27]. Additionally, increased awareness and attention to health matters could introduce reporting bias, which may further explain this observed association.
Unemployment status significantly affected the severity of menopause symptoms in our study. Multiple studies have highlighted the influence of employment status on the severity of menopausal symptoms, with varying results [2, 23, 28, 29]. This variation suggests that for some women, work is a source of stress that exacerbates symptoms, while for others, employment provides social interaction and a busy schedule that helps distract them from menopausal symptoms [28, 29].
To the best of our knowledge, this is the first study to assess barriers to seeking medical advice among women from different regions of Saudi Arabia. Almost half of the participants believed that menopausal symptoms are a natural part of aging and do not require medical attention, which is consistent with previous studies in Asia, which also concluded that most women viewed menopausal symptoms as a natural process and were unaware of the potential benefits of prescription treatments [30]. Similarly, another study found that more than half of the participants did not seek medical advice for menopause because they did not consider it a valid reason to consult a healthcare provider [7]. These findings highlight the need for a societal shift in how menopause is perceived, emphasizing that menopausal symptoms can significantly influence quality of life and that seeking medical support is essential [7].
A study conducted in the United Kingdom identified a lack of knowledge about menopause and HRT among both women and general physicians as key barriers to seeking treatment [31]. Similarly, a study in Taif, Saudi Arabia, revealed that only 16.4% of participants had good knowledge about menopausal hormone therapy, while the vast majority (83.6%) had poor knowledge on the subject [13]. Another study among Saudi physicians found that more than half of the participants experienced difficulty prescribing HRT to postmenopausal patients, with the most commonly reported barrier is patients preferences for complementary and alternative therapies, and difficulty explaining HRT risks and benefits to women [32]. This highlights a widespread gap in awareness and education regarding HRT across different regions. Healthcare providers should reconsider their perspectives on menopause and adopt a more proactive stance in offering support to women experiencing menopausal symptoms [7]. Additionally, enhancing the education of healthcare providers is essential to ensuring they deliver appropriate and effective care to menopausal women [33]. This education should extend beyond simply prescribing hormone therapy to include guidance on lifestyle modifications, such as diet and exercise, which can help alleviate menopausal symptoms [34]. Therefore, physicians at all levels require enhanced knowledge regarding the safety, indications, and contraindications of HRT. It is equally important for them to be educated on the preferred duration and appropriate dosage forms of HRT to effectively balance its potential benefits and risks. This is a critical component of the decision-making process [32].
This study has several limitations. First, the online data collection method, with a predominance of participants from the Western region, limits the generalizability of the findings to the broader Saudi Arabian population, which is large and culturally diverse. Second, the use of a self-administered questionnaire, in which participants rated their own symptoms, may have introduced recall bias. Finally, as with all observational studies, the findings reflect associations rather than causality.
More than half (52.5%) of the perimenopausal and postmenopausal women included in the study experienced severe to very severe menopausal symptoms, with physical and mental exhaustion being the most frequently reported. Risk factors for increased MRS severity included being married, older age, higher education level, unemployment, and the presence of a chronic disease. A frequently cited reason for not seeking medical help was the belief that menopausal symptoms are a natural and expected part of the aging process.
This study highlights an increase in menopausal symptoms among women, with the majority of barriers attributed to physician-related factors. This reflects the need for improved awareness, education, and counseling regarding the management of menopausal symptoms, as well as guidance on the appropriate timing for initiating HRT. Further studies are needed to examine the attitudes of physicians, particularly in primary care, toward menopausal care.
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
SSO and RAA designed the research study. RAA collected the data. Both authors analysed the data. Both authors contributed to editorial changes in the manuscript. Both authors read and approved the final manuscript. Both authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was carried out in accordance with the guidelines of the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board (IRB) of the Biomedical Ethics Committee at King Abdulaziz University Hospital (Ref: 689-23) in February 2024. All participants signed a written informed consent for inclusion before they participated in the study.
The authors would like to thank the study participants for their contribution.
This research received no external funding.
The authors declare no conflict of interest.
During the preparation of this work the authors used ChatGpt-3.5 in order to check spell and grammar. After using this tool, the authors reviewed and edited the content as needed and takes full responsibility for the content of the publication.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.



