1 Department of Obstetrics and Gynecology, Dokuz Eylul University School of Medicine, 35330 Balcova, Izmir, Turkey
2 Department of Radiology, Dokuz Eylul University School of Medicine, 35330 Balcova, Izmir, Turkey
Abstract
Adnexal torsion is a gynecological emergency that can lead to loss of ovarian function if not diagnosed promptly. This study aimed to determine which computed tomography (CT) findings, or combinations of findings, can accurately diagnose adnexal torsion in women presenting with abdominal pain and adnexal masses.
In this retrospective single-center cohort study conducted between January 2018 and December 2023, a total of 66 patients were evaluated. Group 1 (n = 35; 53%) included women who underwent preoperative CT for abdominal pain and were subsequently diagnosed with adnexal torsion. Group 2 (n = 31; 47%) served as the control group and comprised patients who underwent preoperative CT for untwisted adnexal masses. Statistical analysis was performed using SPSS version 26.0. Normality was assessed with the Kolmogorov-Smirnov test. Non-normally distributed variables were analyzed using the Mann-Whitney U test. Categorical variables were analyzed using the chi-square test or Fisher’s exact test. Interobserver agreement for CT findings was evaluated, and logistic regression analyses were conducted. A p-value < 0.05 was considered statistically significant.
Interobserver agreement was almost perfect for the identification of unusual adnexal and uterus location, the presence of an interutero-ovarian mass, the whirlpool sign, peritoneal effusion, and tubal thickening. The unusual location of the adnexa and the presence of the whirlpool sign were significantly more frequent in the adnexal torsion group (Group 1) and remained statistically significant in the logistic regression analysis.
Accurate interpretation of CT scans performed in emergency settings, particularly in experienced centers, may help in reliably diagnosing or excluding adnexal torsion, potentially reducing unnecessary surgical interventions.
Keywords
- adnexal torsion
- computed tomography
- whirlpool sign
Adnexal torsion (AT) constitutes a gynecological emergency that occurs when the ovary and/or fallopian tube undergoes twisting around its vascular pedicle. This mechanical rotation primarily disrupts venous and lymphatic drainage, eventually compromising arterial perfusion if left untreated [1, 2]. Early identification and timely surgical intervention are vital for preserving ovarian viability and minimizing the risk of severe outcomes. Failure to promptly address adnexal torsion can result in irreversible ischemic injury, leading to infertility or necessitating oophorectomy [3].
AT accounts for approximately 2% to 3% of all gynecological emergencies and most commonly affects women of reproductive age, particularly those between 20 and 40 years old [4, 5]. Right-sided torsion is reported more frequently, potentially due to the stabilizing effect of the sigmoid colon on the left side [5]. Risk factors include ovarian cysts or masses larger than 5 cm, pregnancy, assisted reproductive techniques (such as ovulation induction), and prior pelvic surgery [6, 7].
Delayed diagnosis or treatment can lead to irreversible damage to the adnexa, resulting in infertility, infection, and in rare cases, peritonitis or sepsis [2, 5]. Early surgical intervention, ideally via laparoscopy, can restore perfusion and prevent loss of the ovary or tube [3].
Ultrasonography, complemented by color Doppler assessment, is typically employed as the initial imaging tool when adnexal torsion is suspected. Nevertheless, ultrasonography demonstrates limited sensitivity in detecting torsion, primarily because the ovary possesses a dual arterial supply and exhibits variable imaging characteristics [4, 6]. When ultrasonographic evaluation fails to provide definitive results, particularly in non-pregnant individuals, computed tomography (CT) is frequently utilized as a supplementary diagnostic method. CT may reveal various features indicative of adnexal torsion, including ovarian enlargement, displacement of the adnexa, and identification of the characteristic whirlpool pattern [8].
Several CT findings have been associated with AT, such as an enlarged ovary, thickened fallopian tube, abnormal adnexal location, uterine deviation, interutero-ovarian mass, and the presence of the whirlpool sign (a twisted vascular pedicle near the ovary) [4, 6, 8, 9, 10, 11]. Previous research investigating CT characteristics associated with adnexal torsion has faced limitations, including small patient cohorts, diverse study populations, and variability in imaging interpretation [11]. More recent investigations emphasize the necessity of establishing standardized imaging approaches to enhance the diagnostic accuracy for adnexal torsion [12].
Given that adnexal torsion often presents with acute abdominal pain, this study was designed to investigate specific CT features and assess their diagnostic value in differentiating torsion from other adnexal pathologies in standard, well characterized cohort.
This retrospective single-center cohort study concerned patients managed at Dokuz Eylul University School of Medicine between January 2018 and December 2023. Informed consent was obtained from all individual participants included in this study. The study was performed in accordance with the principles of the Declaration of Helsinki. Dokuz Eylul University Ethics Committee approval was provided (file number: 7992-GOA, registration date: 2023/12-23).
A total of 160 women who underwent surgery for adnexal lesions were identified through a search of our institutional surgical registry. Of these, 94 patients who did not undergo preoperative contrast-enhanced CT at our hospital were excluded. Consequently, 66 patients with both preoperative CT imaging and surgical confirmation were included in the study.
To create two clinically comparable groups, the institutional database was queried for women aged 17 years or older who presented with acute abdominal pain and underwent surgery for adnexal lesions during the study period.
Group 1 (adnexal torsion group) consisted of 35 patients who had preoperative CT due to abdominal pain and were diagnosed intraoperatively with AT. These cases were confirmed by histopathology.
Group 2 (control group) consisted of 31 patients who also underwent CT for abdominal pain and subsequently had surgery for adnexal masses without evidence of torsion (e.g., functional cysts, teratomas). These patients served as controls, allowing comparison with the adnexal torsion group.
Both groups were drawn from the same time frame and institutional registry. Importantly, all patients included had similar presenting symptoms and underwent comparable imaging protocols. This design allowed for evaluation of CT findings that may distinguish AT from other causes of adnexal masses in symptomatic women (Fig. 1).
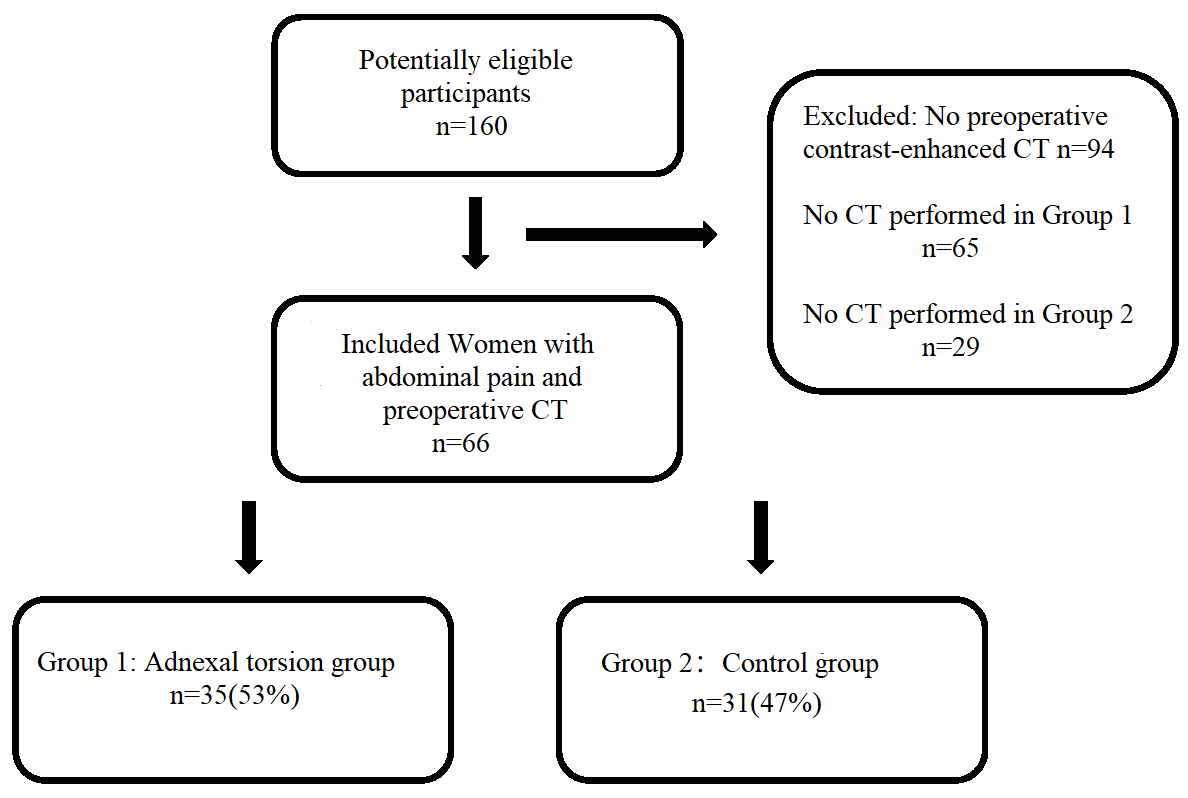 Fig. 1.
Fig. 1. Standards for reporting diagnostic accuracy studies (STARD) diagram to report the flow of participants throughout the study. CT, computed tomography.
CT scans were performed using standardized abdominal imaging protocols with contrast-enhanced acquisition in the portal venous phase. Detailed acquisition parameters are available in Supplementary Table 1 adapted from Hwang et al. [13].
Preoperative CT scans were independently and retrospectively evaluated by two radiologists, possessing 18 and 14 years of expertise in gynecologic imaging (Canan Tuncer Altay and Isıl Basara Akın, respectively), using a randomized sequence within the institutional image archiving system. Any discrepancies in interpretation were resolved through consensus by a third radiologist with 26 years of experience in gynecologic imaging (Mustafa Secil). Although all reviewers were informed about the study’s objectives, they remained blinded to the patients’ clinical, biological, surgical, and histopathological information, as well as the original CT reports generated at the time of imaging.
For each adnexa, the radiologists systematically evaluated multiple parameters across all included cases: ovarian dimensions along three perpendicular axes and the corresponding volume (calculated using the formula: length
All statistical analyses were conducted using SPSS software version 26.0 (IBM Corp., Chicago, IL, USA). Assessment of data normality was performed utilizing the Kolmogorov-Smirnov test. Variables not following a normal distribution were analyzed using the Mann-Whitney U test, and results were reported as median values along with their respective minimum and maximum ranges. Categorical variables were compared employing the chi-square test or Fisher’s exact test, as appropriate, and findings were expressed as frequencies and percentages. Fisher’s exact test was applied when the expected frequency in any cell of the contingency table was less than 1, or when the total sample size was less than 40. When the expected frequency in any cell was between 1 and 5 and the sample size was
Table 1 summarizes the demographic characteristics of the two groups. There were no statistically significant differences between Group 1 and Group 2 in terms of age, gravidity, parity, menopausal status, history of adnexal torsion, contraception methods, or history of pelvic surgery (p
| Variables | Group 1 (Adnexal torsion group) (n = 35, 53%) | Group 2 (Control group) (n = 31, 47%) | p-value | |
| Age (years) | 34 (17–70) | 43 (20–73) | 0.190 | |
| Gravida | 1 (0–3) | 1 (0–5) | 0.560 | |
| Parity | 1 (0–3) | 1 (0–5) | 0.560 | |
| Premenopausal status | 26 (74.2%) | 21 (67.7%) | 0.550 | |
| History of adnexal torsion | 2 (5.7%) | 0 (0.0%) | 0.490 | |
| Contraception | 0.530 | |||
| None | 24 (68.6%) | 26 (83.9%) | ||
| Oral contraceptive pills | 1 (2.9%) | 1 (3.2%) | ||
| Intrauterine device | 2 (5.7%) | 0 (0.0%) | ||
| Condom | 7 (20.0%) | 4 (12.9%) | ||
| Tubal ligation | 1 (2.9%) | 0 (0.0%) | ||
| History of pelvic surgery | 16 (45.7%) | 9 (29.0%) | 0.160 | |
Table 2 shows the histological diagnoses of the adnexal masses in both groups. The most common diagnosis in Group 1 was ovarian functional cysts (22.9%), followed by mature cystic teratomas (17.5%). In Group 2, functional cysts and teratomas were also the most frequent. No histopathological result was available in 5 patients in Group 1 who underwent detorsion only.
| Variables | Group 1 (Adnexal torsion group) (n = 35, 53%) | Group 2 (Control group) (n = 31, 47%) | p-value |
| Mature cystic teratoma | 6 (17.5%) | 10 (32.3%) | 0.150 |
| Ovarian functional cyst | 8 (22.9%) | 11 (35.4%) | 0.250 |
| Mucinous cystadenoma | 5 (14.3%) | 4 (12.9%) | 1.000 |
| Para-Fallopian cyst | 4 (11.4%) | 0 (0.0%) | 0.110 |
| Serous cystadenofibroma | 3 (8.6%) | 5 (16.1%) | 0.570 |
| Serous carcinoma | 2 (5.7%) | 0 (0.0%) | 0.490 |
| Borderline epithelial tumor | 0 (0.0%) | 1 (3.2%) | 0.470 |
| Undetermined | 2 (5.7%) | 0 (0.0%) | 0.490 |
Note: Pathology results were not available because only detorsion surgery was performed on 5 (14.3%) patients in Group 1.
Table 3 shows the interobserver agreement for each evaluated CT feature. The agreement was almost perfect for most findings, particularly the unusual location of the adnexa, interutero-ovarian mass, and tubal thickening (
| Variables | Interobserver agreement rate (%) | Kappa (95% CI) | p-value |
| Unusual location of adnexa | 96.9% | 0.93 (0.85–1.00) | |
| Unusual location of the uterus | 96.8% | 0.93 (0.83–1.00) | |
| Asymmetric crescent-shaped thickening | 87.8% | 0.61 (0.37–0.85) | |
| Haemorrhagic content | 90.9% | 0.71 (0.49–0.92) | |
| Interutero-ovarian | 98.4% | 0.94 (0.83–1.00) | |
| Whirlpool sign | 92.4% | 0.81 (0.65–0.96) | |
| Peritoneal effusion | 100.0% | 1.00 (1.00–1.00) | |
| Pelvic fat haziness and pelvic peritoneal thickening | 92.4% | 0.80 (0.64–0.96) | |
| Tubal thickening | 96.9% | 0.93 (0.85–1.00) |
CI, confidence interval; CT, computed tomography.
Table 4 compares the presence of various CT features between the torsion and control groups. The whirlpool sign, unusual location of the adnexa and interutero-ovarian mass were significantly more frequent in the torsion group (p
| Variables | Group 1 (Adnexal torsion group) (n = 35, 53%) | Group 2 (Control group) (n = 31, 47%) | p-value |
| Largest diameter of the ovary (mm) | 86.8 (45.0–207.0) | 76.0 (34.8–289.5) | 0.160 |
| Unusual location of adnexa | 19 (54.3%) | 7 (22.6%) | 0.009 |
| Unusual location of uterus | 22 (62.9%) | 22 (71.0%) | 0.480 |
| Asymmetric crescent-shaped thickening | 5 (14.3%) | 5 (16.1%) | 1.000 |
| Haemorrhagic content | 8 (22.9%) | 3 (9.7%) | 0.150 |
| Interutero-ovarian mass | 9 (25.7%) | 1 (3.2%) | 0.028 |
| Whirlpool sign | 16 (45.7%) | 2 (6.5%) | |
| Peritoneal effusion | 19 (54.3%) | 13 (41.9%) | 0.300 |
| Pelvic fat haziness and pelvic peritoneal thickening | 10 (28.6%) | 8 (25.8%) | 0.800 |
| Tubal thickening | 25 (71.4%) | 15 (48.4%) | 0.050 |
Univariate logistic regression analysis (Table 5) identified the whirlpool sign and the unusual location of the adnexa as significant predictors of adnexal torsion, with odds ratios of 28.592 (95% CI: 2.308–354.132; p = 0.008) and 8.294 (95% CI: 1.514–45.433; p = 0.010), respectively. In the multivariate logistic regression model (Table 6), both findings remained statistically significant, confirming their independent diagnostic value. The whirlpool sign had an adjusted odds ratio of 16.994 (95% CI: 3.171–91.087; p = 0.001), while the unusual location of the adnexa had an adjusted OR of 5.910 (95% CI: 1.735–20.129; p = 0.004).
| Variables | OR (95% CI) | p-value |
| Largest diameter of the ovary (mm) | 0.999 (0.984–1.013) | 0.800 |
| Unusual location of adnexa | 8.294 (1.514–45.433) | 0.010 |
| Unusual location of uterus | 0.462 (0.114–1.883) | 0.200 |
| Asymmetric crescent-shaped thickening | 1.004 (0.158–6.381) | 0.900 |
| Haemorrhagic content | 1.845 (0.228–14.958) | 0.500 |
| Interutero-ovarian mass | 3.351 (0.228–49.317) | 0.300 |
| Whirlpool sign | 28.592 (2.308–354.132) | 0.008 |
| Peritoneal effusion | 1.923 (0.383–9.661) | 0.400 |
| Pelvic fat haziness and pelvic peritoneal thickening | 0.197 (0.025–1.558) | 0.100 |
| Tubal thickening | 0.779 (0.136–4.459) | 0.700 |
OR, odds ratio.
| Variables | Adjusted OR (95% CI) | p-value |
| Unusual location of adnexa | 5.910 (1.735–20.129) | 0.004 |
| Whirlpool sign | 16.994 (3.171–91.087) | 0.001 |
After completing the multivariate analysis, age, gravidity, and parity were additionally evaluated as potential confounders. Age, gravidity, and parity did not differ significantly between the torsion and control groups (p
Our study demonstrated that the unusual location of the adnexa and the presence of the whirlpool sign are reliable CT features associated with adnexal torsion in women presenting with abdominal pain and adnexal masses. The most common histological diagnoses associated with torsion in our cohort were ovarian functional cysts and mature cystic teratomas, consistent with previous reports [8, 9, 10]. Malignant tumors were rare in our torsion group, which may be explained by the hypothesis that pelvic adhesions, as seen in conditions like endometriosis or tubo-ovarian abscesses, can restrict adnexal mobility and lower torsion risk. Additionally, risk factors such as prior surgery, pregnancy, or tubal ligation did not significantly differ between groups, reinforcing that anatomical and mechanical factors likely play a dominant role. Although ovarian size was greater in the torsion group, the difference was not statistically significant.
Tubal thickening was more common in the torsion group but was not a significant predictor in regression models, echoing prior findings that highlight its variability across observers and imaging protocols [8, 9, 10, 16]. In contrast, the whirlpool sign was highly specific and reproducible, making it a valuable indicator of mechanical torsion. It represents the spiral appearance of twisted vascular structures, correlating well with intraoperative findings. The unusual location of the adnexa, though less studied, also demonstrated strong diagnostic value and interobserver agreement. This feature likely reflects the anatomical displacement caused by torsion and should be considered in future structured radiological assessments.
Differences in the diagnostic performance of CT signs across studies may be due to variations in imaging protocols, use of coronal reconstructions, definitions of imaging findings, or heterogeneity in study populations. Standardization in future studies is essential for establishing consistent and reliable diagnostic criteria. Our findings suggest that both the whirlpool sign and unusual adnexal location are clinically valuable CT features that may aid in early diagnosis and help guide management in emergency settings, especially when ultrasound is inconclusive. Incorporating these signs into diagnostic algorithms could potentially reduce delays in treatment and prevent loss of ovarian function. Additionally, variables such as age, menopausal status, surgical history, and contraceptive use were comparable between groups, minimizing confounding. Nevertheless, unmeasured variables may remain. Future studies with larger, multicenter populations and multivariable models are warranted to strengthen the external validity of these findings. All CT scans were performed using standardized protocols on similar equipment and reviewed by experienced radiologists, enhancing the reproducibility of our observations. However, subtle differences in image quality or interpretation could still influence results.
The main limitation of this study is its retrospective design. Although the sample size may seem modest, it is comparable to similar studies in the literature. The high proportion of torsion cases (53%) resulting from strict inclusion criteria may limit generalizability. Moreover, the study included only symptomatic patients with adnexal masses who underwent surgery, which introduces selection bias and excludes conservatively managed or less severe cases. Nevertheless, this design was intended to reflect the diagnostic challenge encountered in real-world emergency practice. Although ultrasonography remains the first-line modality for suspected adnexal torsion, our analysis focused on CT due to its frequent use in emergency settings when ultrasound results are inconclusive or unavailable. We acknowledge the lack of direct comparison with ultrasound findings as a limitation, which was primarily due to the inconsistent quality and retrospective nature of ultrasound reports. Future prospective studies should incorporate both imaging modalities in parallel to provide a more comprehensive evaluation. Moreover, different brands of contrast agents were used across cases. Although all agents were low-osmolar, nonionic iodinated media with comparable enhancement profiles, slight variability between products could not be entirely excluded and may have minimally influenced the imaging findings. A further limitation concerns five patients who underwent detorsion without oophorectomy. Although the diagnosis of torsion was made intraoperatively based on typical surgical findings, the absence of histopathological confirmation may reduce the robustness of the diagnostic reference standard. Some logistic regression estimates showed wide confidence intervals, suggesting potential overfitting. In particular, the association between the whirlpool sign and adnexal torsion, although statistically significant, should be interpreted cautiously and warrants further validation. Another important consideration is the relatively high number of variables included in the logistic regression analysis relative to the sample size. This may raise concerns regarding overfitting, as reflected in the wide confidence intervals for certain predictors—most notably the whirlpool sign. Although statistically significant, such results should be interpreted with caution and require confirmation in larger prospective studies. Finally, while age and obstetric history were not significantly different between groups, residual confounding cannot be entirely excluded. The relatively small sample size may have also limited the statistical power to detect more subtle associations.
CT is an accurate technique for diagnosing AT in patients with acute abdominal pain and adnexal masses. Interpretation of CT scans performed in emergency situations in experienced centers can help prevent unnecessary surgical procedures by correctly identifying or excluding AT. The use of specific signs, particularly the whirlpool sign and the unusual location of the adnexa, should be emphasized in structured CT interpretations to enhance diagnostic confidence and guide timely intervention.
The datasets generated during the current study were available from the corresponding author on reasonable request.
Concept and design: OY, AA, CTA; Data acquisition: OY, AA, KAM, IBA; Data analysis and interpretation: OY, CTA, MS; Drafting the manuscript: OY, IBA, AA; Drafting the manuscript or reviewing it critically for important intellectual content: KAM, CTA, MS; Knowledge content: OY, MS. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This study was performed in line with the principles of the Declaration of Helsinki. And this was a retrospective cohort research. Informed consent was obtained from all individual participants included in this study. All procedures performed were in accordance with the ethical standards of the Dokuz Eylul University Ethics Committee, and approval was provided (file number: 7992-GOA, registration date: 2023/12-23).
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
During the preparation of this work the authors used ChatGpt in order to check spell and grammar. After using this tool, the authors reviewed and edited the content as needed and takes full responsibility for the content of the publication.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/CEOG38400.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

