1 Department of Obstetrics, Women’s Hospital, School of Medicine, Zhejiang University, 310006 Hangzhou, Zhejiang, China
†These authors contributed equally.
Abstract
The use of transvaginal ultrasound to measure several parameters has been investigated as an alternative to the cervical Bishop score to predict the success rate of induced labor. We analyzed the utility of the cervical Bishop score and cervical elastography ultrasound parameters in assessing cervical ripeness after 39 weeks gestation.
This retrospective case-control study reviewed 230 pregnant women who underwent labor induction and delivered at the Women’s Hospital, School of Medicine, Zhejiang University, from May 2022 to November 2023. Cervical Bishop scores and cervical elastography ultrasound parameters were measured prior to labor induction. According to the labor outcomes, participants were categorized into a successful induction group (n = 220) and a failed induction group (n = 10). We compared the differences between the two groups and analyzed the predictive value of the cervical Bishop score and cervical elastography ultrasound parameters for assessing cervical ripeness using receiver operator characteristic (ROC) curve analysis.
The cervical bishop score in the failed induction group was significantly lower than in the successful induction group (p < 0.05), and the height was also significantly lower in the failed induction group compared to the successful induction group (p = 0.047). No statistically significant differences were found in basic characteristics such as cervical length, cervical hardness, shape of the cervical internal os, cervical transverse width, and internal/external os (IOS/EOS) ratio (p > 0.05). There was no significant difference in the predictive value of the cervical Bishop score and cervical elastography ultrasound parameters for assessing cervical ripeness, with ROC curve areas of 0.706 and 0.710, respectively.
The cervical Bishop score and cervical elastography ultrasound parameters demonstrated equivalent effectiveness in evaluating cervical ripeness.
Keywords
- Bishop score
- cervical elastography ultrasound
- cervical ripeness
- labor induction
Induction of labor stands as one of the frequently employed obstetrical interventions [1]. Cervical ripeness is a key factor in the success of induced labor. The cervical Bishop score has been traditionally considered the gold standard to quantify cervical ripeness [2, 3]. Due to its simplicity and feasibility, the cervical Bishop score is widely used in clinical practice as an important indicator for predicting the success of induced labor. However, the results are largely extent subjective and rely on individual experience of the clinician, which impacts the accuracy of cervical ripeness assessment [4]. The cervical Bishop score is significantly influenced by the subjective factors of the examiner, and repeated examinations may increase the risk of infection, thereby limiting its clinical application. Additionally, digital vaginal examinations provide imprecise estimates of the cervical length or the shape of the internal os in the upper part of the cervix, which diminishes the accuracy of assessing cervical maturity [5]. Bishop score does not provide an objective assessment of the biological parameters of cervical ripening, but rather it is examiner-dependent. Multiple methods have been implemented to evaluate cervical ripeness prior to labor induction, and innovative approaches are currently being investigated for this aim. As early as 1991, Paterson-Brown et al. [6] began attempting to use transvaginal ultrasound to measure several parameters in place of the cervical Bishop score to predict the success rate of induced labor. Over the past few decades, with the development of ultrasound technology, the use of ultrasound as an objective means in obstetrics and gynecology has become a major research tool [7]. Elastography technology assesses the texture of the cervix by examining its histological characteristics and offers specific quantitative indicators to minimize subjectivity in evaluation [8].
Studies show that the cervical elastography ultrasound is a better predictor of cervical ripeness than the traditional Bishop method at full-term [9, 10]. In recent years, increasing evidence indicates that opting for elective induction of labor at 39 weeks could result in more positive perinatal outcomes when compared with the expectant management [11, 12]. In this study, we collected data from 230 pregnant women with a gestational age of 39 weeks or more. We examined the cervical Bishop score and cervical elastography ultrasound parameters in order to compare the effectiveness of these 2 methods in assessing cervical ripeness with the labor onset (regular contractions accompanied by progressive effacement, dilation of the cervix, and descent of the fetal presentation) [13] as the endpoint. In our study, we used 3 cm as standard for defining the labor onset.
This is a retrospective case-control study. It included 230 pregnant women who were registered at the Women’s Hospital, School of Medicine, Zhejiang University, from May 2022 to November 2023, and who underwent labor induction. The participants were classified into 2 groups: a successful induction group and a failed induction group, based on the outcomes of the labor induction process. This research has been approved by the hospital’s ethics committee (ethics number: IRB-20240303-R).
The inclusion criteria for participation in the study were as follows: (1)
Single fetal cephalic position; (2) Indication for induction of labor with no
preceding labor; (3) Absence of clear contraindications to vaginal delivery; (4)
Gestational age
The exclusion criteria included: (1) Multiple pregnancies; (2) Stillbirth; (3) Fetal malformation; (4) Pregnant women with contraindications to vaginal delivery; (5) Scarred uterus; (6) Presence of regular uterine contractions; (7) Previous history of cervical surgery.
The cervical Bishop score was assessed by 2 senior obstetricians prior to the induction of labor. As shown in Table 1, the Bishop scoring system evaluates dilation, consistency, position, effacement, and the fetal head’s station in the pelvis. Each parameter is assigned points, with a total score ranging from 0 to 13. Cervical dilation, effacement, and station are scored from 0 to 3 points, whereas cervical position and consistency are scored from 0 to 2 points [3, 14].
| Score | Dilation (cm) | Position of cervix | Effacement (%) | Station | Cervical consistency |
| –3 to +3 | |||||
| 0 | Closed | Posterior | 0–30 | –3 | Firm |
| 1 | 1–2 | Midposition | 40–50 | –2 | Medium |
| 2 | 3–4 | Anterior | 60–70 | –1, 0 | Soft |
| 3 | 5–6 | - | 80 | +1, +2 | - |
A standardized protocol was employed for measuring cervical length and assessing cervical elastography through E-Cervix. A transvaginal probe (3–10 MHz) connected to the Samsung HERA W10 ultrasound system (S2SKM3HW20000SE, Gangwon-do, Korea) was utilized, with the E-Cervix software (1.03.00a.3009, Seoul, Korea) activated. This was conducted by an experienced sonographer who had received training on the use of the E-Cervix program before labor induction. After emptying the bladder, the subjects remained still and breathed slowly and steadily. Measurements taken included the cervical length, the cervical hardness ratio, the shape of the internal cervical os, the transverse width of the cervix, and the IOS/EOS ratio (internal and external cervical oral strain ratio). As shown in Fig. 1.
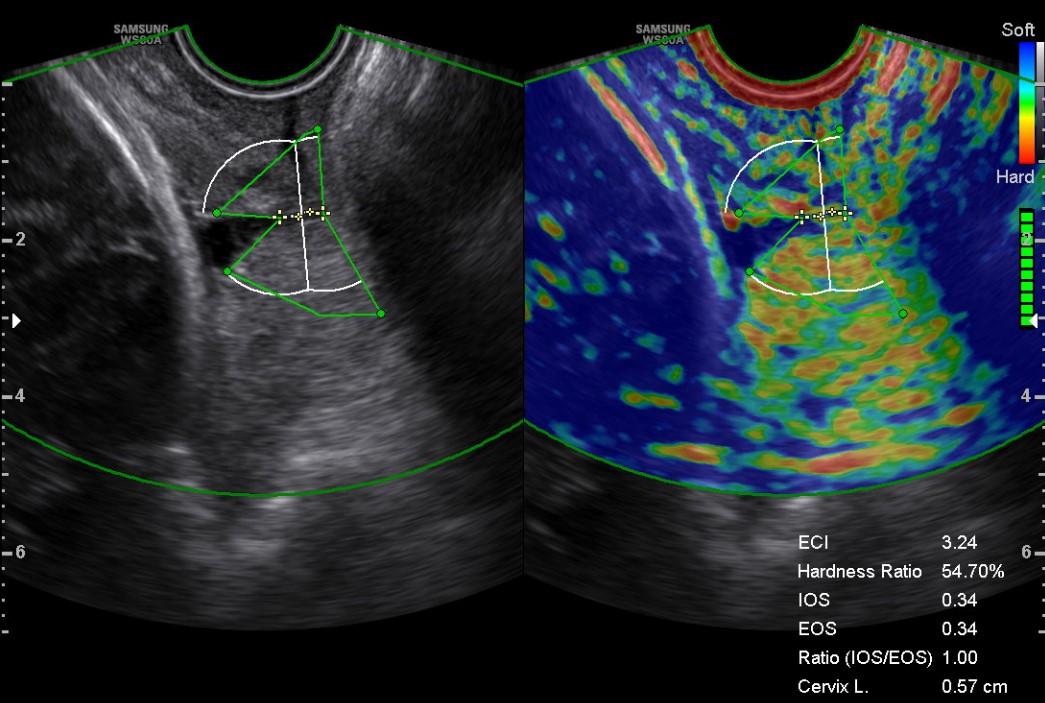 Fig. 1.
Fig. 1.
Transvaginal grayscale sonography and elastography images. The basic characteristics of this pregnant woman: 29 years old, height 1.64 m, 40 weeks gestation, pre-delivery body mass index (BMI) 24.91 kg/m2, weight gain 9 kg during pregnancy. The Bishop score: 5. Cervical elastography ultrasound parameters: cervical length 0.57 cm, cervical hardness ratio 54.7%, cervical internal opening shape Y, cervical transverse width 0.9 cm, internal/external os (IOS/EOS) ratio 1. ECI, elasticity contrast index; Cervix L, cervical length.
The clinical data encompass the following parameters: (i) General information including age, height, prenatal body mass index (BMI), pregnancy weight gain, and gestational age; (ii) The cervical Bishop score; (iii) Cervical elastography ultrasound parameters, which consist of cervical length, cervical hardness ratio, internal cervical os shape, cervical transverse width, and the IOS/EOS.
Kolmogorov-Smirnov test was used to test the normality of quantitative data. The
data conforming to normal distribution were described as mean
Among 230 women who underwent labor induction, 220 experienced successful
induction, while 10 did not. The height of failed induction was less than that of
the successful induction group (p = 0.047). There were no statistically
significant differences in maternal age, prenatal BMI, pregnancy weight gain, or
gestational age between the 2 groups (p
| Successful induction | Failed induction | U | p | |
| (n = 220) | (n = 10) | |||
| Age (years) [median (Q1, Q3)] | 30.5 (28.00, 33.00) | 30.5 (28.75, 35.25) | 902.00 | 0.334 |
| Height (m) [median (Q1, Q3)] | 1.61 (1.58, 1.65) | 1.58 (1.57, 1.60) | 1506.50 | 0.047* |
| Pre delivery BMI (kg/m2) [median (Q1, Q3)] | 26.11 (24.25, 27.85) | 26.14 (23.75, 28.91) | 1098.00 | 0.992 |
| Weight gain during pregnancy (kg) [median (Q1, Q3)] | 13.00 (11.00, 15.00) | 14.00 (12.88, 15.00) | 898.00 | 0.325 |
| Gestational weeks (week) [median (Q1, Q3)] | 40.00 (39.00, 40.00) | 39.00 (39.00, 40.00) | 1317.00 | 0.218 |
*p
As shown in Table 3, the cervical Bishop score in the failed induction group was
lower than that in the successful induction group, while the cervical length was
longer in the failed induction group compared to the successful induction group.
These differences were statistically significant (p
| Successful induction | Failed induction | U/t/ |
p | |
| (n = 220) | (n = 10) | |||
| Bishop score [median (Q1, Q3)] | 4.00 (3.00, 5.00) | 3.00 (2.75, 4.25) | 1556.00 | 0.023* |
| Cervical length (cm) [median (Q1, Q3)] | 2.45 (1.70, 2.99) | 2.58 (2.30, 2.81) | 953.00 | 0.475 |
| Cervical hardness ratio (%) [mean |
55.29 |
59.15 |
0.72 | 0.473 |
| Cervical internal opening shape [n, %] | T (194, 84.35%) | T (10, 100%) | 1.33 | 0.721 |
| Y (13, 5.65%) | Y (0, 0%) | |||
| V (5, 2.17%) | V (0, 0%) | |||
| U (8, 3.48%) | U (0, 0%) | |||
| Cervical transverse width (cm) [median (Q1, Q3)] | 0.00 (0.00, 0.00) | 0.00 (0.00, 0.00) | 1210.00 | 0.295 |
| IOS/EOS [median (Q1, Q3)] | 1.00 (0.86, 1.14) | 1.08 (0.93, 1.46) | 835.50 | 0.205 |
IOS/EOS, internal/external os. *p
As illustrated in Table 4 and Fig. 2, the area under the ROC curve for the cervical Bishop score in assessing cervical ripeness was found to be 0.706. In comparison, the area under the ROC curve for cervical length, cervical hardness, internal cervical os shape, cervical transverse width, and the IOS/EOS ratio as parameters of cervical elastography ultrasound was 0.710. However, this difference is not statistically significant.
| AUC | 95% CI | p | Sensitivity (%) | Specificity (%) | Yoden index | p a | |
| Bishop score | 0.706 | 0.554–0.858 | 0.009** | 72.60 | 60.00 | 0.326 | 0.975 |
| Joint model of cervical ultrasound parameters | 0.710 | 0.564–0.856 | 0.007** | 65.80 | 80.00 | 0.458 |
AUC, area under the curve. p a: The p-value of the
differences in AUC between the two methods. **p
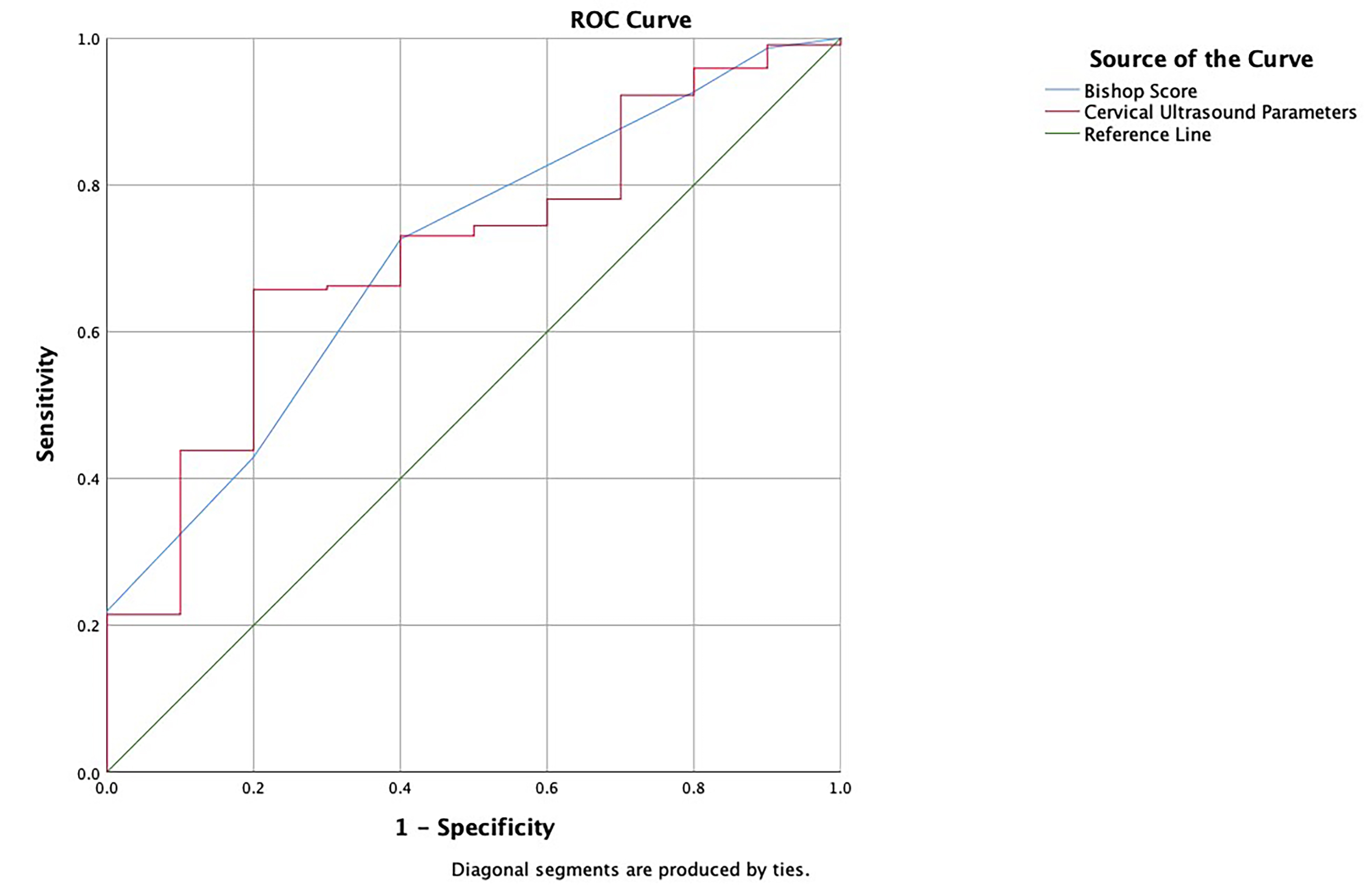 Fig. 2.
Fig. 2.
Receiver operator characteristic (ROC) curve.
Induced labor refers to the use of medication or other methods to initiate the labor process prior to natural labor in order to achieve the goal of labor onset and vaginal delivery. There are numerous factors that can affect vaginal delivery [15, 16]. In our study, the definition of successful induction was onset of labor.
The cervix is primarily composed of extracellular matrix components, including proteoglycans and glycosaminoglycans, along with fibrous elements such as collagen fibers and elastin. Prior to delivery, there is a decrease in the collagen content within the cervical tissue, accompanied by a rearrangement of various extracellular matrix components and collagen fibers. This process results in the gradual softening and shortening of the cervix, ultimately transforming it into a component of the soft birth canal [17]. The cervical hardness can be quantified by measuring the degree of tissue displacement under external compression, a principle known as strain elastography. Consequently, cervical elastography ultrasound, an ultrasound technique capable of quantitatively assessing tissue hardness, is anticipated to enhance the accuracy of evaluating cervical ripeness and may serve as a novel method for predicting cervical ripeness [18]. Ultrasound elastography plays a crucial role in the evaluation of cervical lesions by effectively differentiating between normal and abnormal cervical tissues. This technology is particularly valuable in distinguishing benign lesions from malignant ones, thereby enhancing the accuracy of diagnoses related to cervical health. Its application significantly elevates the diagnostic specificity for cervical cancer, allowing healthcare professionals to make more informed decisions based on the findings. Furthermore, ultrasound elastography not only aids in identifying the depth of infiltration and staging of cervical cancer but also serves as a predictive tool for assessing how well a patient might respond to chemoradiotherapy treatments, providing an essential resource for tailoring individualized treatment plans [19]. In the context of pregnancy, ultrasound elastography proves to be beneficial in monitoring cervical conditions. It aids in the assessment of cervical softening, which is crucial for predicting the likelihood of premature delivery [18, 20].
The cervix ripens prior to delivery, and then shortens and dilates with
contractions of the uterus. Previous studies have shown that cervical length is
an independent predictor of induced labor outcomes [21, 22]. At 37 weeks of
gestation, ultrasound measurement of cervical length can be used to predict the
risk of cesarean section during labor. Patients with cervical length
The Bishop score is a commonly used tool in digital cervical examinations at the time of induction to determine whether cervical ripening is necessary [14]. However, recent studies have suggested that the predictive ability of the Bishop score regarding induction failure may be limited, especially in relation to the newer cervical ripening methods that have emerged [9, 25]. Despite being a subjective assessment method, the Bishop score remains the standard technique for assessing the cervix before labor induction. This system is valued for its simplicity and effectiveness in predicting vaginal delivery.
In clinical practice, vaginal examinations are frequently associated with pain and discomfort for many pregnant women. In contrast, transvaginal ultrasound examinations tend to be more acceptable. One reason for this may be due to the poor lubrication of the birth canal prior to the onset of labor, particularly during the first examination prior to induction. A more objective evaluation of cervical ripeness can guide clinicians to choose the appropriate mode of labor induction and delivery.
The strength of this study lies in its use of successful induction as the endpoint, directly addressing the clinical need for cervical ripeness assessment tools. The results indicate no significant difference in the efficacy of the two assessment methods, suggesting that the traditional Bishop score remains practical in resource-limited settings, while elasticity ultrasound can serve as a supplementary tool. However, this study has some limitations. The induction failure group included only 10 cases, significantly fewer than the success group (220 cases), which may reduce statistical power and result in insufficient identification of differences in certain parameters (such as cervical hardness and internal os morphology) between the groups. Future research should expand the sample size, particularly by increasing the number of cases in the failure group, to enhance the robustness of the results. This study solely considered “successful induction of labor” as the endpoint, without further analysis of maternal and neonatal outcomes (such as duration of labor, mode of delivery, and neonatal complications). Subsequent research should incorporate multidimensional outcome indicators to comprehensively evaluate the clinical significance of the two methods.
This study is retrospective clinical research, whose findings indicate that both the cervical Bishop score and cervical elastography ultrasound are equally effective in assessing cervical ripeness. This has significant implications for selecting appropriate clinical methods to evaluate cervical ripeness in pregnant women. However, given that this study is a retrospective analysis with a limited sample size, further large-scale prospective studies are necessary for additional confirmation and validation.
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
JW and MD designed the research study. YQ performed the research and drafted the manuscript. SB analyzed the data. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was carried out in accordance with the guidelines of the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Women’s Hospital, School of Medicine, Zhejiang University (ethics number: IRB-20240303-R). All patients or their families/legal guardians gave their informed consent for inclusion before they participated in the study.
We would like to express our gratitude to all those who helped us during the writing of this manuscript.
This work was supported by the National Key Research and Development Program of China (No. 2021YFC2700700).
The authors declare no conflict of interest.
During the preparation of this work the authors used Deepseek in order to check spell and grammar. After using this tool, the authors reviewed and edited the content as needed and takes full responsibility for the content of the publication.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.


