1 Achutha Menon Centre for Health Science Studies, Sree Chitra Tirunal Institute for Medical Sciences and Technology, 695011 Trivandrum, Kerala, India
2 Human Biology Division, Fred Hutchinson Cancer Research Center, Seattle, WA 98109, USA
3 Sree Ramaswami Memorial School of Public Health, SRM Institute of Science and Technology, 603203 Chennai, Tamil Nadu, India
Abstract
As one of the most populous countries in the world, India plays a significant role in contributing to the global burden of female-specific cancers. This paper aims to provide a clearer understanding of this burden by comparing the situation in India with that of other countries and regions. Such an understanding will help policymakers assess the adequacy of cancer control measures in India.
The age-standardized incidence rates (ASIR) and age-standardized mortality rates (ASMR) of all cancers among women, as well as the rates of six female-specific cancers, i.e., of the breast, cervix uteri, ovary, corpus uteri, vagina, and vulva, were obtained from the Global Cancer Observatory for the year 2022. The estimates for India were compared with those of countries such as the United States of America (USA), Australia, the United Kingdom (UK), South Africa, El Salvador, and China.
Among the selected countries, India exhibited the lowest incidence and mortality rates for all-cause cancer among women, with rates of 100.83 and 62.61 per 100,000 person-years, respectively. It also reported the lowest incidence of breast cancer (26.6 per 100,000 person-years) and corpus uteri cancer (2.46 per 100,000 person-years) among the selected countries. However, the ASIR and ASMR of cervical cancer were the second highest in India (17.71 and 11.15 per 100,000 person-years) after South Africa (33.18 and 19.03 per 100,000 person-years). The incidence rates in India are below the global median for all cancers (157.66), breast cancer (46.21), and corpus uteri cancer (7.03), but they are above the global median for cervix uteri cancer (14.10). A similar trend was observed concerning cancer-related mortality rates among Indian women. Nearly 54% of cancer incidence and 50% of cancer mortality among women in India are attributed to these six female-specific cancers.
Although India contributes significantly to the global burden of female-specific cancers, the ASIR and ASMR for these cancers are lower than those in many other countries. It is essential to study how sociodemographic transitions influence the patterns of female-specific cancers in high-, low-, and middle-income countries to inform the implementation of effective cancer control strategies by health systems in countries like India.
Keywords
- age-standardized incidence rate
- age-standardized mortality rate
- GLOBOCAN
- female organ cancers
- gynecological cancers
Globally, cancer constitutes a substantial proportion of deaths from noncommunicable diseases. Addressing the cancer burden presents a major challenge for all countries in the current scenario. Recent GLOBOCAN estimates indicate a lifetime risk of approximately 20% for developing cancer and 8 to 11% for experiencing cancer-related deaths. However, there is considerable disparity in cancer burden, with a four- to five-fold difference in incidence rates among different regions and countries [1].
The burden of female organ cancers, including breast cancer and other gynecological cancers (GCs), also varies by region and country [2]. Breast cancer is one of the most common types of cancer in women globally, and an upward trend in age-standardized incidence rates has been observed in all female cancers except for cervix uteri. Between 1990 and 2021, age-specific rates of female cancers increased with age, as higher rates were observed among older women than younger. The rising incidence of breast, ovarian, and uterine cancers has contributed to the global increase in female cancers among women of childbearing age [2].
Variations in survival rates for different GCs have also been documented. A study conducted among older women aged 65 years or above using the Surveillance, Epidemiology, and End Results (SEER) population data demonstrated that the five-year survival rates for women diagnosed with corpus uteri, vulva, and cervix uteri cancers were 76%, 69.7%, and 56%, respectively [3]. In contrast, the five-year survival rates for women with cancers diagnosed in the fallopian tube (47.8%), vagina (44.8%), ovary (31%), and other female organ cancers (24.6%) were lower [3].
Disparities in social development status, lifestyle, and the availability of diagnostic as well as healthcare resources contribute to the differences in the female organ cancer burden across countries and regions [2, 4]. A temporal trend analysis using the World Health Organization (WHO) mortality database for countries such as Japan, the Republic of Korea, and Singapore indicates that age, period, and cohort effects influence the risk of mortality from these cancers [5].
Additionally, the cancer burden is associated with the human development index (HDI). The relationship between HDI and the incidence and mortality of GCs is multifaceted [6]. Countries with very high HDI have lower mortality rates despite higher incidence rates of GCs. This could be due to well-established and advanced healthcare systems, high socioeconomic status, and comprehensive cancer screening programs. Conversely, low HDI countries exhibit the highest incidence rates for GCs, which may be attributed to inadequate or inaccessible healthcare, low socioeconomic status, and a lack of vaccination strategies, along with other co-factors such as a higher prevalence of human immunodeficiency virus (HIV) and human papilloma virus (HPV) infections and/or coinfections [6].
Most cancer cases occur in low- and middle-income countries [7]. In terms of incident cases, India ranks third after China and the United States of America (USA), respectively, contributing to the second-largest number of cancer deaths after China [8]. The leading cancers among women in India are those arising from the breast, cervix, and ovary [9], which indicates that the screening coverage is low, despite various schemes and programs. According to the national family health survey (NFHS-5) data, the percentage of women who underwent cervical cancer screening in India was as low as 1.9%, while the percentage of those who ever participated in breast cancer screening practices was merely 0.9%. Lack of awareness about cancer screening, socioeconomic inequalities, stigma around screening outcomes and cancer, and limited health system resources may all contribute to inadequate screening practices among Indian women [10].
The challenge of addressing the cancer burden persists worldwide despite the availability of early detection and preventive measures. Breast cancer and other GCs substantially contribute to this burden, with notable disparities in their impact across regions and countries due to various factors. As a highly populated country, India witnesses a large number of cancer cases and deaths, adding to the global burden of cancers in general, and breast cancer and other GCs in particular. In this paper, we aim to assess the burden of female organ cancers—breast, cervix uteri, ovary, corpus uteri, vagina, and vulva—in India and compare it to a global context, using the latest age-standardized incidence and mortality estimates from GLOBOCAN reports. These estimates will facilitate valid comparisons of cancer burden between regions and countries. Such comparisons will yield a clearer understanding of the cancer burden in India relative to other countries and help assess the adequacy of cancer control measures in India.
GLOBOCAN, a reliable source of paramount importance in global cancer surveillance, provides comprehensive data on cancer incidence, mortality, and prevalence across 185 countries. Its extensive geographical coverage and high-quality sources, such as population-based cancer registries and the WHO mortality database, enable a detailed analysis of global cancer trends and inform public health policies [11].
For this study, we downloaded the data files available in Microsoft Excel from the Global Cancer Observatory, International Agency for Research on Cancer, World Health Organization, Lyon Cedex 07, France, which provide estimates for cancer incidence and mortality rates in 2022 [8]. The data files on age-standardized incidence rates (ASIR) and age-standardized mortality rates (ASMR) for all cancers, including non-melanoma skin cancer, among women across continents, as well as country-wise estimates for the six female organ cancers—breast, cervix uteri, ovary, corpus uteri, vagina, and vulva—were also obtained from this source.
Six countries from different regions were selected to compare India’s incidence and mortality rates for all cancers, as well as the female-specific cancers included in the study. The USA, Australia, and the UK were chosen to represent high-income countries from North America, Oceania, and Europe, respectively. South Africa and El Salvador were selected to represent upper- and lower-middle-income countries from Africa and Central America. Finally, China was included as a highly populated upper-middle-income country neighboring India [12].
We conducted a descriptive analysis to evaluate the cancer burden across regions and countries. The median and range of ASIR and ASMR for both overall and specific cancers were estimated for 185 countries. These estimates were compared across continents, and India’s estimates were specifically compared with those of the countries included in the study. Additionally, the proportionate contribution of these six cancers to all cancers among women was compared across regions and countries.
The trends in the ASIR and ASMR for breast and cervix uteri cancers in India and China from 2003 to 2017 were also illustrated. The HDI scores, which reflect socioeconomic status, were obtained for the selected countries from the World Population Review website [13]. In addition, the most recent data for 2021 on current health expenditure per capita (in USA$), current health expenditure (% of gross domestic product (GDP)), and population density (people per square kilometer), along with the rural population percentage (of total population) for 2023 and adolescent fertility rate (births per 1000 women aged 15–19) for 2022 were collected from the Databank, World Development Indicators, The World Bank Group 2024 [14]. Spearman Rank correlation was then calculated to estimate the relationship between these indicators and the ASIR (incidence).
The descriptive analysis was performed using STATA 17.0 (Statistics and Data Science, Standard Edition, Stata Corp, 4905 Lakeway Drive, College Station, TX, 77845, USA). The figures were generated using STATA and Microsoft Excel 2007 (Microsoft, Redmond, Washington, USA).
Table 1 presents the ASIR and ASMR for all cancers, as well as for the six female organ cancers, in women across different regions. The highest age-standardized all-cancer incidence was found in Oceania (371.3), followed by North America (340.7), Europe (253.4), Latin America and the Caribbean (177.4), Asia (157.7), and Africa (140.7). In contrast, the highest age-standardized all-cancer mortality was found in Africa (89.8), followed by Europe (84.4), Oceania (82.9), Latin America and the Caribbean (77.6), North America (74.9), and Asia (70.5).
| ASR among females (Per 100,000 female population) | Africa | Latin America and the Caribbean | North America | Europe | Oceania | Asia | Global | |||||||
| Inc | Mort | Inc | Mort | Inc | Mort | Inc | Mort | Inc | Mort | Inc | Mort | Inc | Mort | |
| *All cancers | 140.7 | 89.8 | 177.4 | 77.6 | 340.7 | 74.9 | 253.4 | 84.4 | 371.3 | 82.9 | 157.7 | 70.5 | 196.9 | 91.7 |
| Breast | 40.5 | 19.2 | 52.0 | 13.2 | 95.1 | 12.3 | 75.6 | 14.6 | 91.5 | 15.4 | 34.3 | 10.5 | 46.8 | 12.7 |
| Cervix uteri | 26.4 | 17.6 | 15.1 | 7.7 | 6.4 | 2.2 | 10.6 | 3.9 | 9.6 | 4.5 | 13.9 | 6.7 | 14.1 | 7.1 |
| Ovary | 5.3 | 4.0 | 5.7 | 3.6 | 7.5 | 3.8 | 9.3 | 5.0 | 8.1 | 4.5 | 6.2 | 3.7 | 6.7 | 4.0 |
| Corpus uteri | 3.5 | 1.1 | 8.1 | 2.0 | 22.3 | 3.2 | 15.5 | 2.8 | 13.8 | 2.5 | 5.7 | 1.2 | 8.4 | 1.7 |
| Vaginal | 0.4 | 0.2 | 0.4 | 0.1 | 0.4 | 0.1 | 0.3 | 0.1 | 0.5 | 0.2 | 0.3 | 0.2 | 0.4 | 0.2 |
| Vulva | 1.2 | 0.6 | 0.8 | 0.3 | 1.9 | 0.4 | 1.7 | 0.5 | 1.3 | 0.3 | 0.4 | 0.2 | 0.8 | 0.3 |
| **GCs | 36.8 | 23.5 | 30.1 | 13.7 | 38.5 | 9.7 | 37.4 | 12.3 | 33.3 | 12.0 | 26.5 | 12.0 | 30.4 | 13.3 |
| Breast cancer and GCs | 77.3 | 42.7 | 82 | 26.8 | 133.6 | 21.9 | 112.9 | 26.8 | 124.7 | 27.4 | 61 | 22.4 | 77.2 | 26.0 |
*All cancers: cancers of any cause and origin, including non-melanoma skin cancer.
**Gcs: cancers of cervix uteri, ovary, corpus uteri, vagina, and vulva.
ASR, age-standardized rate; GCs, gynecological cancers; Inc, incidence rate per 100,000 person-years; Mort, mortality rate per 100,000 person-years.
A similar pattern was observed for breast cancer, where Africa had an age-standardized incidence rate of 40.5—less than half that of Oceania (91.5) and North America (95.1). However, the age-standardized mortality rate in Africa was the highest among all at 19.2. Conversely, the incidence and mortality rates for cervical cancer were notably high in Africa (26.4 and 17.6, respectively). For ovarian cancer, both the incidence and mortality rates were highest in Europe (9.3 and 5.0, respectively).
The highest incidence rate for corpus uteri cancer was observed in North America (22.3) followed by Europe (15.5) and Oceania (13.8). However, all continents reported lower mortality rates for corpus uteri cancer, with rates of 3.2 or below. The incidence and mortality of cancers of the vagina and vulva were minimal across all regions. When considering the five GCs, the incidence ranged from 26.5 in Asia to 38.5 in North America, with variations in incidence for cancers of the cervix, ovary, and corpus uteri (Table 1).
Among the selected countries, Australia had the highest incidence of all-cause female cancers (415.21), followed by the USA (341.74), the UK (292.54), China (197.03), South Africa (190.35), El Salvador (128.37), and India (100.83). However, the highest mortality rates were observed in South Africa (110.58), followed by the UK (87.63), the USA (73.61), Australia (71.21), China (67.81), El Salvador (64.6), and India (62.61). The incidence of breast (26.6) and corpus uteri (2.46) cancers were also the lowest in India. However, the incidence of cervical cancer in India (17.71) ranked second highest after South Africa (33.18). The combined incidence rate of GCs (excluding breast cancer) was highest in South Africa (47.18), followed by the USA (38.36), the UK (33.74), Australia (29.65), India (27.87), China (26.9), and El Salvador (23.04) (Table 2).
| Countries | Incidence per 100,000 person-years | ||||||
| *All cancers among women | Breast cancer | Cervix uteri | Ovary | Corpus uteri | Vagina/Vulva | **GCs | |
| Australia | 415.21 | 101.47 | 5.25 | 7.84 | 14.61 | 1.95 | 29.65 |
| The USA | 341.74 | 95.91 | 6.32 | 7.32 | 22.47 | 2.25 | 38.36 |
| The UK | 292.54 | 94.03 | 7.51 | 9.2 | 14.76 | 2.27 | 33.74 |
| China | 197.03 | 33.04 | 13.83 | 5.68 | 6.84 | 0.55 | 26.9 |
| South Africa | 190.35 | 47.8 | 33.18 | 5.11 | 6.17 | 2.72 | 47.18 |
| El Salvador | 128.37 | 39.65 | 15.19 | 4.29 | 2.91 | 0.65 | 23.04 |
| India | 100.83 | 26.6 | 17.71 | 6.57 | 2.46 | 1.13 | 27.87 |
| Median of 185 countries | 157.66 | 46.21 | 14.10 | 6.26 | 7.03 | 0.00 | 31.54 |
| Min | 34.71 | 4.56 | 2.14 | 0.69 | 0.06 | 1.10 | 5.83 |
| Max | 415.21 | 105.42 | 95.89 | 15.33 | 26.22 | 5.87 | 105.38 |
| Countries | Mortality per 100,000 person-years | ||||||
| *All cancers among women | Breast cancer | Cervix uteri | Ovary | Corpus uteri | Vagina/Vulva | **GCs | |
| South Africa | 110.58 | 16.96 | 19.03 | 4.44 | 2.66 | 1.05 | 27.18 |
| The UK | 87.63 | 13.98 | 1.96 | 4.75 | 2.71 | 0.63 | 10.05 |
| The USA | 73.61 | 12.19 | 2.17 | 3.67 | 3.13 | 0.46 | 9.43 |
| Australia | 71.21 | 12.28 | 1.43 | 3.92 | 2.16 | 0.36 | 7.87 |
| China | 67.81 | 6.1 | 4.54 | 2.64 | 1.05 | 0.22 | 8.45 |
| El Salvador | 64.6 | 7.79 | 8.43 | 2.68 | 0.81 | 0.33 | 12.25 |
| India | 62.61 | 13.7 | 11.15 | 4.64 | 0.96 | 0.56 | 17.31 |
| Median of 185 countries | 80.85 | 14.53 | 6.97 | 4.07 | 1.88 | 0.00 | 14.16 |
| Min | 24.67 | 2.33 | 1.07 | 0.78 | 0.00 | 0.41 | 4.42 |
| Max | 150.93 | 38.85 | 64.33 | 9.29 | 9.53 | 4.30 | 71.13 |
*All cancers: cancers of any cause and origin, including non-melanoma skin cancer.
**GCs: cancers of cervix uteri, ovary, corpus uteri, vagina, and vulva.
Min, minimum; Max, maximum.
Mortality due to all cancers was highest in South Africa (110.58), with notably high rates for breast cancer and other GCs (16.96 and 27.18, respectively). India ranked second for breast and cervical cancer mortality (13.7 and 11.15) after South Africa (16.96 and19.03). All other countries, except South Africa, reported lower mortality rates than India (17.31) for GCs. India’s high mortality rate (17.31) for GCs is primarily driven by the cervix uteri mortality rate (11.15), which is only lower than that of South Africa (19.03), while all other countries reported lower mortality rates for GCs (Table 2).
The incidence rates in India are below the median rates for all cancers (157.66 vs. 100.83), breast cancer (46.21 vs. 26.6), and corpus uteri cancer (7.03 vs. 2.46) when compared to the 185 countries. Similarly, India’s mortality rates fall behind the median rates for all cancers (80.85 vs. 62.61), breast cancer (14.53 vs. 13.7), and corpus uteri cancer (1.88 vs. 0.96). In contrast, the incidence rates in India surpass the median rates for cervix uteri (14.10 vs. 17.71), ovary (6.26 vs. 6.57), and vulva/vagina (0.00 vs. 1.13) cancers. Likewise, the mortality rates for India exceed the median rates for cervix uteri (6.97 vs. 11.15), ovary (4.07 vs. 4.64), and vulva/vagina (0.00 vs. 0.56) cancers (Table 2).
Fig. 1 illustrates the contribution of breast cancer and other GCs to the incidence rates of all cancers among women across different regions. In Africa, the six cancers account for 55% of all cancer incidence and 47.6% of all cancer mortality among women. In Asia, they contribute 38.7% and 31.2% to all cancer incidence and mortality, respectively. In India, these six cancers represent nearly 54% of all cancer incidence and 50% of all cancer mortality among women (Fig. 2). South Africa and El Salvador follow India in the contribution of these cancers to the total cancer incidence among women. However, the percentage of these six cancers contributing to all cancer mortality among women is lower in El Salvador than India (Fig. 2).
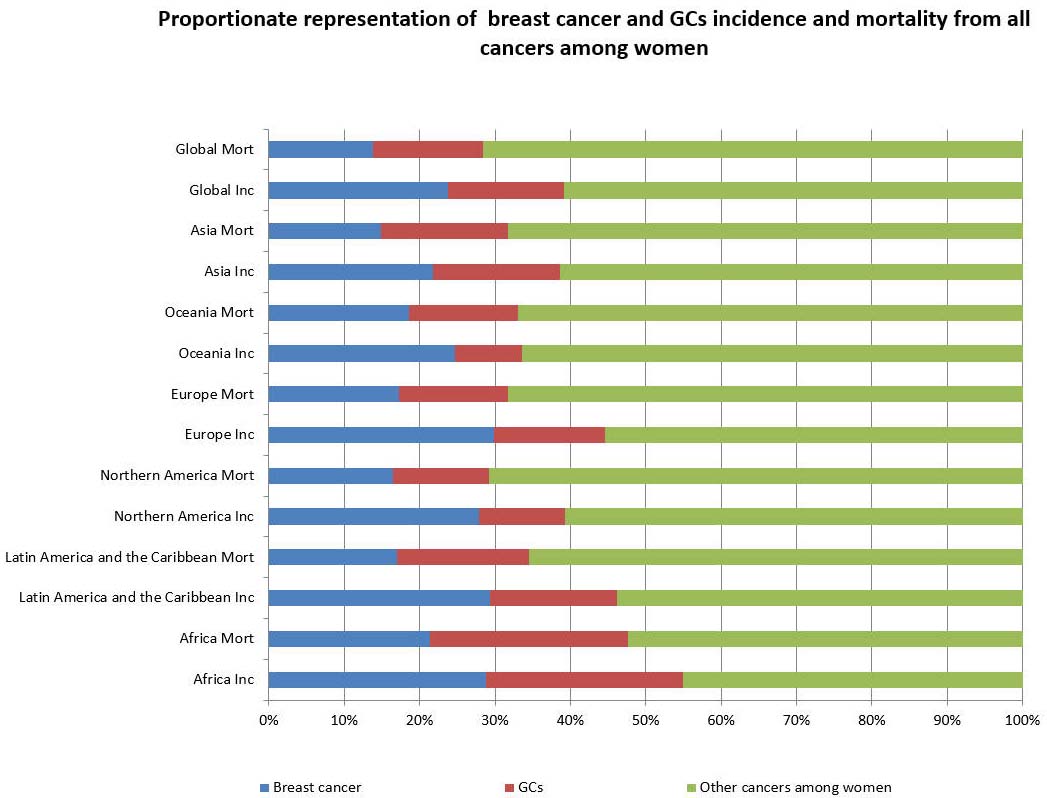 Fig. 1.
Fig. 1. Global incidence and mortality rates due to breast and GCs—proportionate representation from all cancers among women.
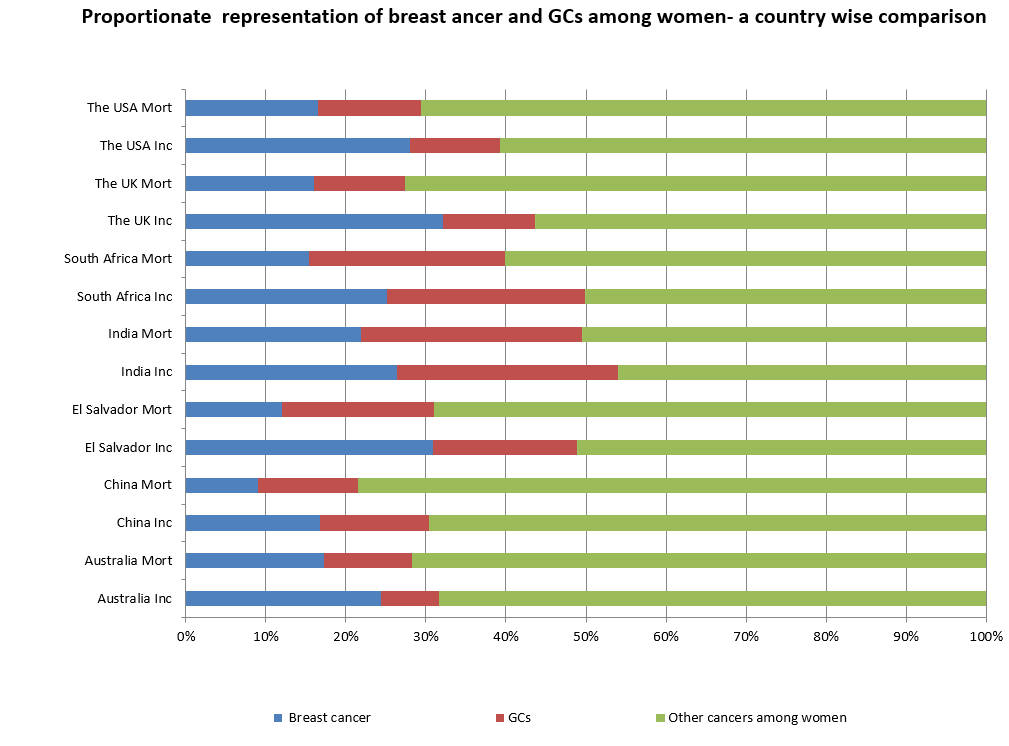 Fig. 2.
Fig. 2. Contribution of breast and other reproductive cancers to all cancer incidence and mortality among women—A comparison between selected countries.
Fig. 3 shows trends in the ASIR and ASMR of breast and cervical cancers in India and China from 2003 to 2017. Breast cancer incidence exhibits an upward trend in both countries, while the trend for cervix uteri moves in the opposite direction, showing a decline.
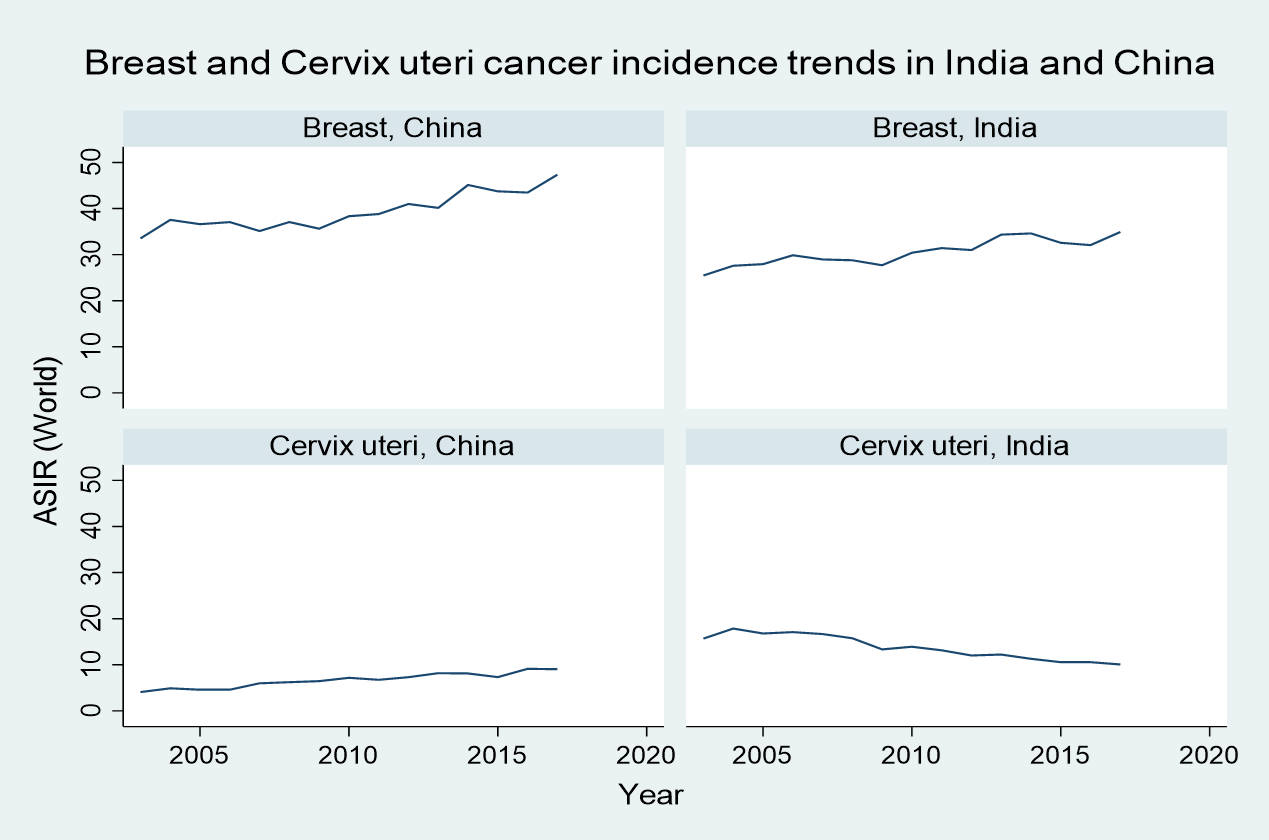 Fig. 3.
Fig. 3. Breast and cervix uteri cancer incidence trends in India and China from 2003 to 2017.
Table 3 (Ref. [13, 14]) and Table 4 present selected sociodemographic indicators and the results of the correlation analysis between ASIR and ASMR and these indicators. The HDI, health expenditure per capita, and current health expenditure (% of GDP) followed a similar pattern, showing a positive correlation with overall cancer rates among women, as well as with breast, ovarian, and corpus uteri cancers. In contrast, these indicators demonstrated a negative correlation with cervical cancer incidence.
| Countries | HDI 2022 | Current health expenditure per capita (current USA$) 2021 | Current health expenditure (% of GDP) 2021 | Population density (people per sq. km of land area) 2021 | Rural population (% of total population) 2023 | Adolescent fertility rate (births per 1000 women ages 15–19) 2022 |
| Australia | 0.95 | 7055.37 | 10.54 | 3.34 | 13.38 | 7.73 |
| United States | 0.93 | 12,012.24 | 17.36 | 36.30 | 16.70 | 15.12 |
| United Kingdom | 0.94 | 5738.48 | 12.36 | 277.05 | 15.36 | 9.99 |
| China | 0.79 | 670.51 | 5.38 | 150.44 | 35.43 | 11.15 |
| South Africa | 0.72 | 583.67 | 8.27 | 48.96 | 31.18 | 60.89 |
| El Salvador | 0.67 | 442.21 | 9.72 | 304.74 | 24.61 | 54.55 |
| India | 0.64 | 74.00 | 3.28 | 473.42 | 63.64 | 16.30 |
| ASIR | HDI 2022 | Current health expenditure per capita (current USA$) 2021 | Current health expenditure (% of GDP) 2021 | Population density (people per sq. km of land area) 2021 | Rural population (% of total population) 2023 | Adolescent fertility rate (births per 1000 women ages 15–19) 2022 |
| All cancers among women | 0.96 | 0.96 | 0.75 | –0.86 | –0.82 | –0.75 |
| Breast cancer | 0.86 | 0.86 | 0.86 | –0.82 | –0.93 | –0.50 |
| Cervix uteri | –0.86 | –0.86 | –0.71 | 0.61 | 0.79 | 0.86 |
| Ovary | 0.75 | 0.64 | 0.54 | –0.32 | –0.61 | –0.82 |
| Corpus uteri | 0.86 | 0.96 | 0.86 | –0.68 | –0.71 | –0.61 |
| Vagina/Vulva | 0.32 | 0.32 | 0.46 | –0.36 | –0.39 | 0.11 |
ASIR, age-standardized incidence rates.
Conversely, population density, the proportion of the rural population, and the adolescent fertility rate exhibited the opposite trend. These indicators positively correlated with cervical cancer incidence but negatively correlated with the ASIR and ASMR of other cancers.
There are considerable differences in the burden of female organ cancers among continents. In Asia, breast cancer incidence was the lowest, while cervical cancer incidence was lower than in Africa, Latin America, and the Caribbean. At the same time, cancer incidence rates for corpus uteri were low in Africa and Asia. However, the six female organ cancers’ contribution to the total cancer burden among women was observed to be high in the African continent. Nearly half of the all-cause incidence and mortality of cancers among women was due to these six cancers, whereas it was less than 40% in Asia. Specifically for India, the contribution of these six cancers to the overall incidence and mortality among women was more than 50%.
The incidence and mortality for GCs being highest in Africa, and East Africa in particular, may be attributed to its proximity to HIV infections and restricted access to early detection or treatment strategies [6]. When comparing South Africa with India, all cancer incidence and mortality rates among women were higher in South Africa, with notably high age-standardized incidence rates for breast and cervical cancers. However, the mortality rates for these cancers did not differ notably between the two countries. Limited access to healthcare services, socioeconomic disparity, and the presence of HPV infection across the African region likely contribute to the elevated incidence of GCs in South Africa [6].
Of 185 countries, China ranks 58th and 145th in ASIR and ASMR, respectively, for all cancers among women, whereas India ranks 170th and 162nd [8]. However, the ASIR and ASMR show different patterns when considering breast cancer and other GCs. Though the breast cancer incidence is lower in India compared to China (26 vs. 33 per 100,000 person-years), the breast cancer mortality rate is only half in China compared to India (6.1 vs. 13.7 per 100,000 person-years). Similarly, China maintains a better mortality rate compared to India for other GCs. Although, when considering the contribution of the six female organ cancers, China falls behind India with a lower proportion of female organ cancer incidence and mortality; conversely, other cancers contribute significantly to all cancer incidence and mortality among Chinese women. Trends from 2010 to 2018 in the incidence and mortality rates of cancers affecting the female genital organs in China suggest that most of these cancers increased during this period, particularly cervical cancer incidence and mortality across both rural and urban areas, despite a historical reduction in cervical cancer rates in China [15].
A comparison of cervical cancer incidence rates between China and India in the first two decades of this century clearly illustrates a slight but consistent increase in its incidence in China, contrasting with the notable reduction in incidence among many other low- and middle-income countries, such as India. Sociodemographic advancement positively influences a population by reducing infection-related cancers, including cervical and vaginal cancer incidence and mortality. Conversely, such transitions may increase the incidence of cancers like breast, ovary, and corpus uteri [16].
At this point, the finding of this increase in cervical cancer incidence in China warrants global attention. While socioeconomic improvements can reduce sociodemographic risk factors for cervical or other HPV-infection-related cancers in one direction, they can also contribute to behavioral risk factors that expand the possibility of acquiring persistent HPV infections, thus increasing cancer incidence in the other direction [17]. The findings from China suggest that comprehensive and sustainable cancer control strategies are warranted, considering the diverse socioeconomic development levels across China’s regions [16]. This serves as an example for low- and middle-income countries like India, where sociodemographic improvements alone cannot effectively reduce the cervical cancer burden, and highlights the need for more effective strategies to control the burden of HPV-related cancers.
Compared to India, the age-standardized incidence rates for all cancers among women, as well as breast cancer incidence rates, are three to four times higher in Australia, the UK, and the USA. However, all-cause mortality rates and mortality due to breast cancer show only minimal variations in the comparison. At the same time, the incidence and mortality rates of cervical cancer are relatively low in these countries. Factors such as the availability of conventional and well-placed healthcare services, public health initiatives, and extensive cancer screening programs in such regions may contribute to improved cancer control [6].
In Australia, GCs constitute almost 9.2% of cancers and nearly 10% of mortality rates due to cancer among women. Between 1994 and 2004, a gradual decrease in the incidence and mortality of cervical cancer was observed [18]. This can be attributed to the National Cervical Cancer Screening Program introduced in 1991. However, in 2024, the overall incidence of GCs gradually progressed to 49 per 100,000 women, up from 43 per 100,000 in 2003, with the increase in uterine cancer largely influencing this progression. The mortality of uterine cancer progressed from 3.3 deaths per 100,000 women in 2000 to 4.8 deaths per 100,000 women in 2024 [18].
Xu et al. (2024) [19] reported an escalation in breast cancer incidence among younger women in the USA, noting that young women diagnosed with breast cancer exhibit a poorer prognosis compared to their older counterparts. An increase in the incidence of Stage I tumors was previously observed, perhaps due to young women detecting those tumors earlier than before. However, an increase in the incidence of Stage IV cancers was also observed [19]. This may be attributed to the fact that in the USA, breast cancer screening among women without risk factors was not conducted before the age of 40, leading them to bear the responsibility of detecting any abnormalities that may result in later-stage diagnoses. Other factors contributing to the increased incidence of breast cancer among young women may include obesity, early age at menarche, family history of breast cancer, and increased alcohol intake [19]. Genetic susceptibility also plays a crucial role in the considerable variation in the incidence of breast and ovarian cancers between East Asian and Caucasian populations [16].
In the case of El Salvador from the Latin American region, the breast cancer incidence rate was higher compared to India, but the cervical cancer rate was slightly reduced; however, the mortality rates for both cancers were lower than in India. Cervical cancer is the principal cause of cancer-related deaths among women in El Salvador [20]. However, HPV screenings followed by treatments for more women could be incorporated into the management strategy for reducing cervical cancer mortality in this region [20]. In high-income countries, breast cancer incidence has increased, especially among those who have undergone epidemiological transition and economic expansion [21]. The Central and South American (CSA) region has experienced such changes owing to a high incidence. Additionally, risk factors such as lack of physical activity, changes in women’s menarche, and breastfeeding patterns may contribute to the high incidence of breast cancer in these regions [21].
The success of countries such as Australia, the USA, and the UK in reducing mortality due to cervical cancer can be attributed to organized screening and efficient healthcare systems. For example, Australia, which ranks in the top ten countries globally for healthcare efficiency, has a government-funded universal health system that ensures equity in access to healthcare services at the population level. The country has also established effective national programs for delivering HPV vaccinations and screening for cervical cancer. However, socioeconomic disparities exist in the participation observed within these programs [22].
While Australia demonstrates the benefits of a universal healthcare model, implementing a similar system in India poses challenges due to the large population and limited government resources. Nonetheless, India can take incremental steps toward equity in healthcare by initiating universal screening programs at the primary healthcare level and involving community health workers to promote these programs within local communities. Such ground-level initiatives can facilitate early detection of female cancers without imposing a significant financial burden on families and the healthcare system [22].
In our analysis, we found that the HDI, health expenditure per capita, and current health expenditure (% of GDP) positively correlated with overall cancer rates among women, as well as with breast, ovarian, and corpus uteri cancers; however, a negative correlation was observed with cervical cancer. Conversely, population density, the proportion of the rural population, and adolescent fertility rates showed a positive correlation with cervical cancer but a negative correlation with other cancers (Table 4). Socioeconomic inequality is a global issue, and the role of socioeconomic status in cancer outcomes has been extensively studied. A recent umbrella review of socioeconomic status and cancer outcomes reiterates the worst health outcomes in the poorest populations; this disparity exists both between countries and within countries of diverse socioeconomic statuses [23]. Incidence, prognosis, screening, and treatment accessibility are all influenced by socioeconomic status. Even when the incidence of certain cancers (for example, breast cancer) is high in countries with very high HDI, the mortality rates are observed to be very low. Conversely, countries with lower incidence rates for certain cancers may have very high mortality rates. Well-organized screening, healthcare accessibility, and resource allocation to healthcare contribute to these variations among countries [23].
Notably, ASIR and ASMR eliminate biases stemming from differences in the population structure, thus enabling valid comparisons among countries. However, the robustness of ASR comparisons across countries is subject to limitations. The reliability of the estimates can be affected by data quality and coverage, which may vary significantly by country. This is particularly true for low- and middle-income countries, where organized cancer registries are unavailable. Methodological inconsistencies and the under-representation of rural populations in available cancer registries further affect the estimates. Additionally, utilizing estimates from neighboring countries due to the unavailability of high-quality local data can also bias the estimation of ASIR and ASMR [11, 24, 25].
A recently published research paper conducted a similar global comparison as the one in this study. The authors described a detailed analysis of age-specific rates of the six female cancers across different countries and the contribution of China to women-specific cancers [16]. However, the present study focused on emphasizing India’s global position. Such an attempt would benefit a highly populated and resource-constrained country in promoting effective cancer control strategies in the future.
In this study, we observed that the ASIR and ASMR do not follow the same order among the regions or countries selected. Even though certain regions have high incidence rates, the mortality rates may not be alarmingly high, and vice versa. The African continent, for instance, had the highest burden in terms of mortality rates due to all-cause cancer, even when the incidence rates were less than half of those in Oceania and North America. This discrepancy may result from cancer cases not being diagnosed and reported during disease progression, but only identified upon death. Alternatively, the lack of proper treatment opportunities for those diagnosed with cancer could also lead to increased mortality rates. The mortality rate was high in Africa (89.8), where the incidence (140.7) was less than half that of Oceania and North America.
Despite the sociocultural disparities and infrastructural insufficiencies to meet the requirements of cancer control in a largely populated country, it is surprising to see the lowest all-cause incidence and mortality rates due to cancer among women in India, as compared to the other countries. This could be an effect of underreporting or a lower rate of diagnosis, leading to lower incidence rates. At the same time, those diagnosed could be effectively treated, resulting in low mortality rates, as observed in this study. Hence, the present comparative analysis of cancer statistics for India with other countries reveals that while the absolute numbers of cancer cases and deaths in India are substantial, the ASIR and ASMR in India are much lower than in many other countries and regions.
Though this appears encouraging, India’s vast population and limited healthcare resources necessitate continuous initiatives to provide cancer management facilities for a large number of patients and extend coverage of cancer control activities across the diverse population. Ensuring proper diagnosis and accurate reporting of cancer cases as well as deaths to avoid underdiagnosis or underreporting is also essential. A more robust cancer control strategy, along with improved healthcare infrastructure and extended diagnostic facilities, can further reduce the cancer burden, particularly of women-specific cancers that can be prevented or detected early.
Sociodemographic indicators are highly correlated with breast and other GCs, though these correlations may vary in different directions. Further exploration of the sociodemographic transition and the changing cancer patterns in high-, low-, and middle-income countries is required to thoroughly understand how such transitions influence the cancer burden in diverse populations. Research on genetic and environmental factors specific to cancer-prone regions could expound the disparities in cancer incidence and mortality. The role of innovative solutions, such as artificial intelligence, mobile health, and low-cost diagnostic tools, in improving early detection and access to healthcare, especially in resource-limited areas, can also be explored further.
In India, policies should focus on strengthening cancer registries to ensure more accurate data, particularly in rural areas. Scaling HPV vaccination programs and intensifying awareness programs to help people adopt lifestyle modifications, preventive measures, early detection, and timely treatment are crucial for controlling cervical cancer, breast cancer, and other GCs. Additionally, investments in healthcare infrastructure are required, especially in underserved regions, along with incentives for research and the development of affordable solutions for cancer management.
We used publicly available data for this study. The cancer incidence and mortality data extracted for the study is from the Global Cancer Observatory. The HDI scores were obtained for the selected countries from the World Population Review website. The health expenditure data, along with population density, rural population percentage and adolescent fertility rate were collected from the Databank, World Development Indicators, The World Bank Group 2024.
RM, PRP, and JVT designed the research study. RM and JVT obtained and analyzed data from the Global Cancer Observatory. PRP and GMG provided assistance and advice on data compilation, analysis, and interpretation of the observations. RM and JVT prepared the initial draft of the manuscript, and PRP and GMG contributed to completing and revising the draft. All authors reviewed and contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This study uses only publicly available, de-identified, aggregate data and as such institutional review board approval is not required.
We thank the efforts of various agencies and numerous individuals contributing to the available data that help make such a global comparison. We also acknowledge Paper True for their language editing services.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.



