1 Department of Obstetrics, The Second Affiliated Hospital of Fujian Medical University, 326000 Quanzhou, Fujian, China
2 Department of Nursing, The Second Affiliated Hospital of Fujian Medical University, 326000 Quanzhou, Fujian, China
Abstract
The rising incidence of gestational diabetes mellitus (GDM), driven by modern lifestyle and dietary changes, underscores the need for effective management strategies. This prospective observational study evaluates the effectiveness of group prenatal care combined with nutritional guidance in managing GDM.
This research is a prospective study. Convenience sampling was used to identify pregnant women who registered for and received regular prenatal care at the Second Affiliated Hospital of Fujian Medical University obstetrics and gynecology department from February 2023 to February 2024. Based on the recorded antenatal care methods, the study included 50 patients in the observation group and 46 patients in the control group. The control group received routine prenatal care, whereas the observation group received group prenatal care supplemented with nutritional guidance. Dietary compliance, GDM knowledge, self-management ability, and perceived social support were assessed and compared between the two groups.
Post-intervention analysis revealed that the observation group exhibited significantly higher scores in dietary compliance, GDM knowledge, self-management ability, and perceived social support compared to the control group (p < 0.05).
The implementation of group prenatal care combined with nutritional guidance significantly improves dietary compliance, enhances GDM knowledge, and boosts self-management skills and perceptions of social support in pregnant women with GDM.
The study is registered on https://www.isrctn.com/ (registration number: ISRCTN14579442).
Keywords
- group healthcare model
- personalized nutritional guidance
- pregnant women with GDM
- pregnancy outcome
The increasing prevalence of gestational diabetes mellitus (GDM) in China highlights the growing importance of effective management and prevention strategies [1]. This upward trend has been associated with modern lifestyle changes and dietary habits, underscoring the need for early intervention and effective management of GDM. Recent statistics indicate that GDM affects approximately 1.78 million women in China, making it one of the most common pregnancy-related complications [2]. GDM not only compromises maternal and neonatal health but also elevates the risk of type 2 diabetes and cardiovascular disease for both mothers and their offspring [3].
The current management strategies for GDM generally include individualized nutritional intervention, blood glucose monitoring, and weight management. However, these traditional approaches often encounter challenges such as inadequate patient adherence and limited professional support. In response, the combined approach of group prenatal care with nutritional guidance has emerged as a promising alternative. This model seeks to enhance patient self-management and improve pregnancy outcomes by integrating standardized professional lifestyle management with individualized nutritional counseling and systematic blood glucose monitoring [4].
Following the guidelines of the American Diabetes Association, this study developed a tailored maternal nutritional assessment and management program aimed at stabilizing blood glucose levels [5]. By employing group prenatal care alongside nutritional guidance, the study aims to empower pregnant women and enhance their self-management abilities [6]. This research evaluates the practical application of this combined approach and aims to support the development of more effective GDM management strategies. The study’s findings are detailed below.
This research is a prospective study. A convenience sampling method was employed to select pregnant women who were registered and received regular prenatal care in the Department of Obstetrics and Gynecology at the Second Affiliated Hospital of Fujian Medical University from February 2023 to February 2024 were retrospectively included. They were grouped according to the different antenatal care methods recorded, with 50 patients in the observation group and 46 patients in the control group, as delineated in the patient selection flow chart (Fig. 1). The control group received routine prenatal care, whereas the observation group received group prenatal care combined with nutritional guidance in addition to the standard care provided to the control group. This study adhered to the principles of the Helsinki Declaration and our study was registered on https://www.isrctn.com/ (registration number: ISRCTN14579442) and can be found at https://www.isrctn.com/ISRCTN14579442.
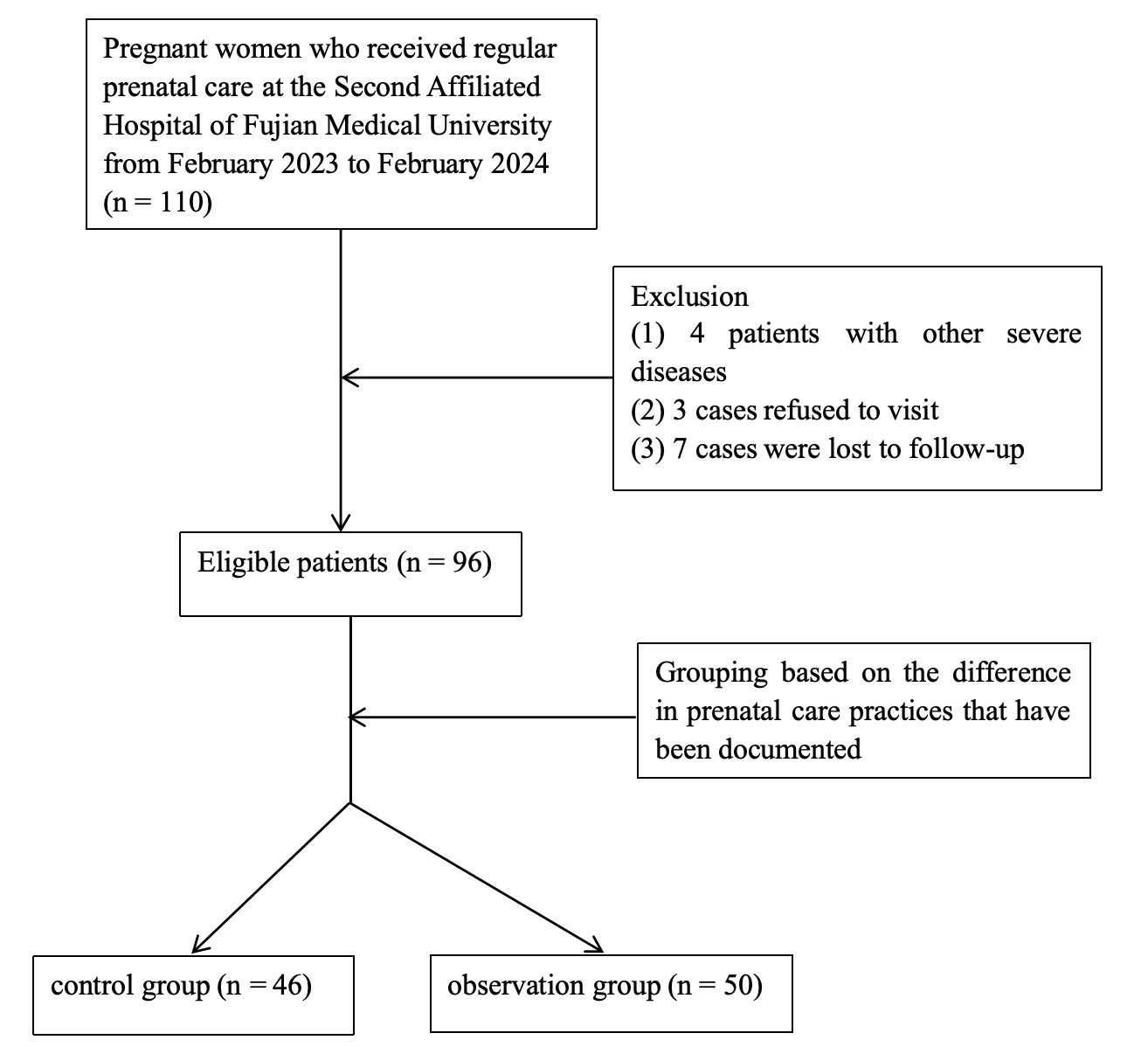 Fig. 1.
Fig. 1. Flow chart of the study design and grouping.
Inclusion criteria: participants were included if they met the diagnostic criteria [7]; (1) the patients undergoing a 75-gram oral glucose tolerance test (OGTT) during pregnancy: fasting blood glucose
Exclusion criteria: participants were excluded if they had severe pregnancy complications or communication disorders due to various diseases.
In the control group, a perinatal health care card was established for each participant following standard procedures. The prenatal examinations were conducted as scheduled, including routine blood glucose monitoring, regular prenatal visits, and fetal ultrasound assessments. Nursing care encompassed dietary control, exercise, regular prenatal check-ups, and pharmacological treatment. Traditional pregnancy care measures involved moderate exercise, a balanced diet, maintaining a normal weight, and avoiding tobacco and alcohol.
In addition to the routine care provided to the control group, the observation group utilized a WeChat platform for enhanced management through the group prenatal care model. This approach included internet-based self-management, group activities, and social support.
The team for the intervention was organized as follows: an associate chief nurse served as the group leader, overseeing the development and coordination of cluster activities. An obstetric nurse was responsible for establishing maternal health records and including patients in the WeChat management group. An obstetrician provided online consultations to address various issues encountered by pregnant women. Another obstetric nurse focused on monitoring patient blood glucose levels and managing dietary guidance. Additionally, a nursing graduate student was tasked with data collection, conducting scale surveys, preparing health education content modules, and organizing themes for cluster activities. The group leader conducted uniform training for all team members, covering maternal theoretical knowledge and operational skills, and performed assessments to ensure the effectiveness of the training.
Obstetric nurses entered maternal data collected between 24 weeks and 28 weeks of gestation into personal health records. Team members used the platform to monitor and assess various health indicators, prenatal examination results, and the psychological status of pregnant women. Weekly recordings included parameters such as blood pressure, abdominal circumference, uterine height, body weight, and fetal movement. Abnormal results were promptly addressed with guidance from the team. Pregnant women documented their psychological changes, experiences from prenatal examinations, and daily life activities through online communication and group interactions. The obstetrician reminded patients to upload abnormal prenatal examination results, including deviations in body weight, amniotic fluid index, blood glucose levels, and blood pressure, to the WeChat platform in a timely manner following each examination. The platform also provided regular reminders and text messages about diet, exercise, medication, and prenatal examination schedules based on the doctor’s recommendations.
The online group activities were designed based on both domestic and international pregnancy health care models and were aligned with “Diagnosis and therapy guideline of pregnancy with diabetes mellitus” [8]. The curriculum incorporated the “Internet +” group pregnancy health care model, addressing common health issues and informational needs of pregnant women in China [9].
A total of 92 pregnant women with GDM were divided into eight groups, each consisting of 8 to 12 participants, based on their expected delivery dates. Each group was supervised by a senior midwife, an obstetric nurse, and an attending physician. Activities were conducted by an experienced midwife (with over 10 years of experience) and an attending physician, with sessions recorded by the obstetric nurse. The intervention spanned from 24 weeks to 28 weeks of gestation to 42 days postpartum, with a total of seven sessions, each lasting two hours. Table 1 below shows the specific contents of the pregnancy health care program of the “Internet +” group.
| Time | Theme | Goal | Main contents |
| 28 weeks gestation | Building peer relationships | 1. Recognize each other and build trust. | 1. Self-introduction. |
| 2. Learn self-monitoring methods during pregnancy. | 2. Guide pregnant women and their families to discuss their knowledge of gestational diabetes and their educational needs. | ||
| 3. Understand GDM. | 3. Instruct pregnant women to self-monitor parameters such as blood pressure, weight, abdominal circumference, uterine height, and fetal movement; provide relevant knowledge about gestational diabetes. | ||
| 4. Browse health education content weekly; develop, implement, and record health plans. | |||
| 30 weeks gestation | Lifestyle guidance during pregnancy | 1. Implement a reasonable diet and exercise plan. | 1. Health assessment. |
| 2. Reduce unhealthy living habits. | 2. Guide pregnant women and their families to discuss their current eating, exercise, and sleeping habits. | ||
| 3. Promote activity during pregnancy. | 3. Provide case analysis and PowerPoint (PPT) lectures on reasonable diet and exercise during pregnancy. | ||
| 4. Encourage sharing of diet and exercise experiences among pregnant women. | |||
| 32 weeks gestation | Prevent adverse pregnancy outcomes | 1. Understand the pregnancy test report. | 1. Health assessment. |
| 2. Recognize pregnancy complications. | 2. Guide pregnant women and their families to discuss their understanding of prenatal examination results and the presence of gestational diabetes. | ||
| 3. Provide case analysis and PPT lectures on pregnancy complications. | |||
| 4. Encourage strict adherence to health plans, including diet, exercise, and body weight management. | |||
| 34 weeks gestation | Psychological support | 1. Recognize negative emotions and learn coping strategies. | 1. Health assessment. |
| 2. Guide pregnant women and their families to discuss negative emotions experienced during pregnancy and coping strategies. | |||
| 3. Use the Self-Rating Anxiety and Depression Scale to assess psychological status; psychologists provide methods for managing adverse emotions. | |||
| 4. Encourage communication with family, medical staff, and other pregnant women in the group. | |||
| 36 weeks gestation | Recognize signs of childbirth | 1. Identify signs of labor. | 1. Health assessment. |
| 2. Master delivery preparation skills. | 2. Guide pregnant women and their families to discuss signs of labor and delivery preparation. | ||
| 3. Understand breastfeeding. | 3. Provide PPT lectures and model demonstrations on the delivery process. | ||
| 4. Encourage joint preparation of delivery materials with families. | |||
| 5. Educate on the benefits of breastfeeding, particularly for mothers and infants with diabetes, and its role in reducing future diabetes risk in infants. | |||
| 38 weeks gestation | Enhancing confidence in delivery | 1. Understand the delivery room environment and prepare delivery items. | 1. Health assessment. |
| 2. Guide pregnant women and their families to discuss their emotions about delivery and necessary delivery supplies. | |||
| 3. Share experiences and review the delivery room environment to boost confidence. | |||
| 4. Encourage communication with experienced mothers and record their feelings. | |||
| 5. Recommend “hypoglycemic exercises” 3–5 times a week, and advise against exercising on an empty stomach, as both fasting and exercise can influence insulin secretion and blood glucose levels. | |||
| 42 days postpartum | Postpartum maternal and child care | 1. Master neonatal care and rehabilitation exercises. | 1. Health assessment. |
| 2. Identify postpartum diabetes symptoms. | 2. Guide pregnant women and their families to discuss postpartum rehabilitation and the feasibility of breastfeeding while on medication. | ||
| 3. Provide PPT lectures and model demonstrations on postpartum care; rehabilitation specialists explain postpartum rehabilitation. | |||
| 4. Instruct mothers on early contact with newborns, breastfeeding techniques, and observation of neonatal health indicators. Perform neonatal blood glucose monitoring as needed. |
GDM, gestational diabetes mellitus.
(1) Diet Compliance Questionnaire [10]: a self-developed diet compliance scale for GDM patients was used, encompassing three dimensions: diet treatment attitude, motivation, and behavior regulation. This scale includes 13 items and employs a Likert 5-point scale, with a maximum total score of 65 points. Higher scores indicate better dietary compliance. The scale has a Cronbach’s alpha coefficient of 0.85.
(2) GDM Knowledge Level Questionnaire [11]: this questionnaire consists of 16 items across three dimensions: knowledge of gestational diabetes, diet during pregnancy, and exercise. The total score is 80 points, with higher scores reflecting greater knowledge of diabetes. The Cronbach’s alpha coefficient for this questionnaire is 0.868.
(3) Self-Management Ability Questionnaire [12]: this instrument includes four dimensions: daily life behavior, fetal monitoring behavior, compliance behavior, and self-protection behavior, comprising 25 items. The total score ranges from 25 to 125, with higher scores indicating better self-management ability. The Cronbach’s alpha coefficient for this questionnaire is 0.926.
(4) Perceived Social Support Level: developed by Dou et al. [13], this measure includes three dimensions: family support, friend support, and other support, with a total of 12 items. Higher scores represent greater perceived social support. The Cronbach’s alpha coefficient ranges from 0.85 to 0.91, and the test-retest reliability is 0.85.
Data analysis was performed using SPSS 25.0 statistical software (IBM Corp., Chicago, IL, USA). For measurement data that followed a normal distribution, results are presented as mean
Among the 110 patients, 7 patients went missing, 3 patients refused to visit, and 4 patients had serious illnesses. Our data analysis showed no significant difference in the general data between the two groups (p
| Group | Control group (n = 46) | Observation group (n = 50) | χ2/t | p | |
| Age (years) | 29.15 | 28.63 | 0.898 | 0.371 | |
| Pre-pregnancy BMI (kg/m2) | 25.87 | 26.17 | –0.540 | 0.591 | |
| Fasting blood glucose (mmol/L) | 5.31 | 5.36 | –0.313 | 0.755 | |
| Education | |||||
| Middle school or below | 10 (21.73%) | 13 (26.00%) | 0.908 | 0.635 | |
| College and undergraduate | 34 (73.91%) | 33 (66.00%) | |||
| Graduate or above | 2 (4.34%) | 4 (8.00%) | |||
BMI, body mass index.
Post-intervention, the dietary compliance score of patients in the observation group was significantly higher than that of the control group (p
| Group | No. of case | Dietary compliance | |
| Before intervention | After intervention | ||
| Control group | 46 | 47.00 | 50.09 |
| Observation group | 50 | 47.23 | 62.98 |
| t | –0.537 | –14.132 | |
| p | 0.593 | ||
After the intervention, the GDM knowledge score was significantly higher in the observation group compared to the control group (p
| Group | No. of case | GDM knowledge | |
| Before intervention | After intervention | ||
| Control group | 46 | 54.29 | 66.22 |
| Observation group | 50 | 53.02 | 71.51 |
| t | 0.797 | –3.631 | |
| p | 0.428 | ||
GDM, gestational diabetes mellitus.
The self-management ability of pregnant women improved significantly in the observation group compared to the control group after the intervention (p
| Group | No. of case | Self-management ability of pregnant women | |
| Before intervention | After intervention | ||
| Control group | 46 | 93.62 | 101.24 |
| Observation group | 50 | 95.49 | 112.23 |
| t | –1.229 | –10.412 | |
| p | 0.222 | ||
After the intervention, the perceived social support score was found to be significantly better than that of the control group, and the difference was statistically significant (p
| Group | No. of case | Perceived social support | |
| Before intervention | After intervention | ||
| Control group | 46 | 77.10 | 76.67 |
| Observation group | 50 | 76.94 | 79.26 |
| t | 0.485 | –2.284 | |
| p | 0.629 | 0.025 | |
Dietary compliance is critical for managing GDM and directly influences the effectiveness of dietary treatment and glycemic control [14]. The results of our present study demonstrated that group pregnancy care combined with nutritional guidance significantly improved patients’ dietary compliance. The dietary compliance score in the observation group was notably higher than in the control group, indicating that group pregnancy care can effectively stimulate patients’ self-management potential. Through dietary guidance, patients developed a correct dietary attitude, which encouraged them to engage more actively with dietary management knowledge. In this study, the integration of group pregnancy care and nutritional guidance achieved a multi-level and multi-directional connection. Initially, guiding patients to identify and address individual poor eating behaviors helped resolve diet management issues, stimulated their intrinsic motivation for dietary management, and successfully mobilized their enthusiasm for diet management [15]. Subsequently, family members’ supervision facilitated the correction of poor eating habits, supported the development of positive habits such as maintaining a diet and blood glucose diary, and enhanced dietary compliance by leveraging family support [16]. Lastly, strengthening the interaction and communication among team members effectively increased patients’ awareness of dietary control and improved their confidence in diet management, leading to a significant enhancement in dietary compliance [17]. Therefore, the combination of group pregnancy care with nutritional guidance proved to be highly effective in improving dietary compliance among GDM patients, supporting a more comprehensive approach to overall patient management.
The results of this study indicated that, following the intervention, the GDM knowledge score in the observation group was significantly higher compared to the control group, with statistical significance, suggesting that group pregnancy care, which provides personalized attention-tailored to patient needs, enhances their understanding and management of GDM-related issues. Therefore, the patients were better able to absorb and retain relevant knowledge [18]. The group setting facilitated the sharing of experiences and addressing of uncertainties, fostering interaction and knowledge exchange, which improved learning outcomes. Patients benefited from the success stories of other group members, which likely motivated them to engage more actively with diabetes management [19]. Additionally, the combined nutritional guidance offered comprehensive information on various aspects of pregnancy care, including diabetes management, diet, and nutrition. This holistic approach enabled patients to acquire broader health knowledge [20]. Thus, the significant improvement in clinical outcomes observed with group pregnancy care combined with nutritional guidance presents a viable and comprehensive method for the effective management of GDM patients.
Active self-management in pregnant women with GDM is essential for achieving optimal maternal and fetal outcomes and for reducing the risk of developing type 2 diabetes in both the patients and their offspring [21]. The results indicated that the total self-management score for pregnant women in the observation group was significantly higher than that in the control group following the intervention, suggesting that group-based pregnancy care combined with nutritional guidance enhances the self-management capabilities of women with GDM. Unlike traditional pregnancy management models, this study used a group pregnancy care model consisting of seven intervention sessions, each lasting 2 hours. This format allowed for thorough discussion and communication, ensuring that participants fully understood and effectively applied self-management strategies [22]. By empowering patients, the intervention facilitated the development of daily habits such as recording fetal movements, which in turn stimulated maternal engagement and improved self-management [23]. Health assessments conducted before the intervention covered maternal health plans, prenatal examination items, and personal health issues, providing a comprehensive basis for personalized self-management [24]. Additionally, discussions led by experienced midwives effectively communicated pregnancy care and nutritional knowledge, increasing patients’ awareness of their condition and appropriate self-management methods [25]. Moreover, group activities fostered the sharing of experiences and promoted collective support, which bolstered patients’ confidence in managing their condition [26]. In summary, these factors collectively contributed to the significant improvement in self-management levels observed with group pregnancy care combined with nutritional guidance.
The results of this study indicated that, following the intervention, the perceived social support scores in the observation group were significantly higher than those in the control group, consistent with results reported in both domestic and international studies [27]. The “Internet +” group pregnancy care model facilitates group management of pregnant women, thereby enhancing social interaction, and this approach provides a platform for pregnant women to connect, share experiences, and build closer social networks [28]. Specifically, pregnant women engage with online health education, participate in group activities, and interact in chat groups where they exchange examination results and pregnancy experiences and discuss challenges and discomforts. This collaborative environment allows them to resolve issues, form friendships, and receive peer support [29]. Additionally, team members are involved throughout the pregnancy management process, addressing the evolving needs for pregnancy healthcare knowledge and offering professional guidance [30]. Group activities focused on psychological support aim to address negative emotions and reduce tension among pregnant women before delivery, thereby alleviating pregnancy-related stress. In a group setting, patients are more likely to encounter individuals with similar experiences, fostering mutual understanding and emotional resonance. This shared experience contributes to the development of stronger social support networks [31]. Additionally, the group provides a platform for learning, communication, and discussion, allowing pregnant women to access a broader range of information, which facilitates not only the dissemination of knowledge but also the enhancement of social support through communication, enabling pregnant women to receive more advice and assistance in managing GDM. Group interactions offer diverse forms of social support, including guidance from professional medical teams, the sharing of practical experiences among group members, and emotional support from peers. This multifaceted approach helps to address the needs of pregnant women more comprehensively.
In summary, the “Internet +” group pregnancy care model combined with nutritional guidance provides comprehensive support for patients with GDM. This group management approach establishes an integrated platform for social interaction, allowing pregnant women to engage in learning, communication, and discussion from the first trimester, thereby forming a supportive social network. Additionally, the model effectively alleviates concerns and stress related to pregnancy by offering various forms of social support, including professional guidance, shared experiences, and emotional support from peers within the group. However, this study faced limitations, including constraints on human resources and scheduling and transportation issues for prenatal examinations, which necessitated shifting group activities to an online format. This adjustment limited the integration of professional prenatal care and may have impacted the study outcomes. Moreover, the exclusion of pregnant women with low social support after loss to follow-up could have influenced the results, warranting further investigation.
The authors declare that all data supporting the findings of this study are available within the paper and any raw data can be obtained from the corresponding author upon request.
XCH and HFZ designed the study and carried it out. XCH, HFZ, MJZ, HYW, YPX supervised the data collection, analyzed the data, interpreted the data. XCH, HFZ, MJZ, HYW, YPX prepared the manuscript for publication and reviewed the draft of the manuscript. All authors have read and approved the manuscript. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This study complied with the guidelines of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Second Affiliated Hospital of Fujian Medical University (Approval no. 2023-254). Written informed consent was obtained from a legally authorized representative(s) for anonymized patient information to be published in this article.
Not applicable.
This work was supported by Provincial clinical key specialty construction project (Grant No. HLZDZK202302).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

