1 Department of Gynaecology, The Affiliated Hospital of Xuzhou Medical University, 221006 Xuzhou, Jiangsu, China
2 Health Management Centre, Affiliated Hospital of Xuzhou Medical University, 221006 Xuzhou, Jiangsu, China
†These authors contributed equally.
Abstract
Our goal was to add an auxiliary examination method for the detection of cervical cancer, and to further explore its application value in clinical staging and treatment.
Shear wave elastography (SWE) technique was used to examine the cervical hardness of patients, and the maximum, mean and minimum values of elastic modulus were recorded, with differences being compared. The area under the receiver operating characreristic (ROC) curve and diagnostic efficacy of elastic modulus were compared with Medcalc software. The differences of elastic modulus values under different parameters were compared in the cervical cancer group.
The mean, maximum and minimum values of the cervical cancer group were all the highest, and the differences were statistically significant. The area under the ROC curves were 0.925, 0.909 and 0.873, respectively. For the mean and maximum values, the Youden indexes were 0.79 and 0.72, the positive likelihood ratios were 21.74 and 19.97, and the negative likelihood ratios were 0.18 and 0.25. The optimal cut-off point was 82.2 kilpoascal (kPa) for maximum value and was 66.5 kPa for mean value. Elastic modulus were all significantly different according to International Federation of Gynecology and Obstetrics (FIGO) stages and tumor lesion size. Also, elastic modulus of cervical cancer patients before and after radiotherapy were statistically significant.
SWE technology has an application value in the detection of cervical cancer. The mean and maximum values have higher diagnostic accuracy. SWE technology also has potential clinical application value in the clinical staging and treatment of cervical cancer, but further studies with larger sample sizes are needed.
Keywords
- application value
- cervical cancer
- clinical staging and treatment
- elastic modulus
- shear wave elastography (SWE)
The incidence and mortality of cervical cancer ranks as the fourth malignant tumor in women worldwide [1, 2]. Persistent infection with high-risk human papillomavirus (hrHPV) is the main cause of cervical cancer [3, 4]. Approximately 90% of cervical cancers occur in underdeveloped or developing countries with inadequate screening or lack of human papillomavirus (HPV) vaccination [5]. Early diagnosis and accurate staging are the basis for a good prognosis. At present, the diagnosis of cervical cancer is mainly through cervical cell scraping, and hrHPV testing, colposcopy, and pathological biopsy of the cervix and endocervical canal [6]. However, the coverage of cervical cancer screening and HPV vaccination is insufficient in China. Therefore, it is necessary to seek an economical, non-invasive and convenient auxiliary examination method, so as to timely remind clinicians to screen patients for cervical cancer.
Study has demonstrated that the elastography software installed on the ultrasound scanner can greatly improve the detection accuracy of ordinary ultrasound technology, increase its clinical application value and significantly improve the accuracy of disease diagnosis [7]. Shear wave elastography (SWE) is a kind of elastography, which is a new form of real-time dynamic elastography technology [8]. It can achieve real-time imaging and has good image quality. It displays tissue elastography in real time by color coding technology, where red indicates hard tissues, green indicates moderately stiff tissues and blue indicates softer tissues [9]. These are quantified as Young’s modulus (elastic modulus) values in kilpoascal (kPa), so this technique utilizes use numerical values to describe the hardness differences between tissues [10]. Pathological changes, such as the presence of tumors or inflammation, alter the composition and structure of the tissue and increase the stiffness of the diseased tissue [11]. The cervical tissue is of medium hardness, and in the presence of cervical cancer, the cervical tissue becomes significantly hard, allowing hardness to be one of the characteristics to distinguish benign and malignant cervical lesions [12]. SWE technology quantifies the hardness of cervical tissue by using Young’s modulus value [13], which is a form of quantitative elastography in real terms and has the advantages of being objective, economic, non-invasive, non-radiation, real-time dynamic and repeatable [14].
This study utilized SWE technology to detect cervical stiffness of the subjects and provide a quantitative evaluation index, in order to explore the application value of this objective, economical, convenient and non-invasive examination technology for patients with cervical cancer. This technique may contribute to the screening of cervical cancer, and provide a new reference index for assisting cervical cancer screening. Second, the relationship between cervical tissue stiffness and clinicopathological factors in patients with cervical cancer was further analyzed, and the value of SWE technology in clinical staging and treatment of cervical cancer was explored.
Data of patients treated in the department of Gynecology, Affiliated Hospital of Xuzhou Medical University from October 2020 to April 2022 were collected, mainly from outpatient colposcopy and inpatient wards. Patients who met the inclusion criteria were included in the study.
The age ranged from 18 to 73 years. All subjects signed informed consent, and this study was approved by the Ethics Committee of the Affiliated Hospital of Xuzhou Medical University (Ethical approval number: XYFY2020-KL154-01).
(1) All patients had postoperative pathological data, including cervical biopsy, cervical conization or radical resection of cervical cancer. According to the pathological results, they were divided into three groups: chronic cervicitis group (cervicitis group, n = 40), cervical intraepithelial neoplasia (CIN) group (n = 40), and cervical cancer group (n = 87).
(2) Outpatients with HPV typing results undergoing colposcopy were in line with the indications for colposcopy [15], and transvaginal SWE technology was performed before colposcopy. Ward patients underwent transvaginal SWE techniques prior to surgery.
(3) The Karnofsky Performance Status (KPS) of all patients was
(1) Did not meet the listed inclusion criteria.
(2) Cervical cancer during pregnancy; cervical stump cancer.
(3) Severe dysfunction of heart, liver or kidney; the presence of other malignant tumors; history of chemoradiotherapy and cervical surgery.
(4) Patients who failed to complete SWE measurement at the end of radiotherapy were excluded from the study.
The Supersonic Imagine Aixplorer color Doppler ultrasound (Software version12.5.0.891, Aix-en-Provence, France) instrument with built-in SWE technology, SE12-3 vaginal probe, frequency 3~12 MHz was used in this study. Before the examination, the patient emptied the bladder and was assisted to lie flat and assume the lithotomy position. The vaginal probe was coated with a coupling agent and covered by a disposable condom. First, transvaginal ultrasound was used to examine the routine conditions of the uterus, adnexa and pelvic cavity. Subsequently, the maximum, mean and minimum values of cervical stiffness were measured by SWE technique. Each index was measured three times, and the average value was recorded and stored.
The clinical data of the cervical cancer group were collected and analyzed, and
the patients with complete diagnosis and treatment records were included in the
analysis. The clinical data of 36 cervical cancer patients were collected. All
patients were staged according to the 2018 International Federation of Gynecology
and Obstetrics (FIGO) staging system. Relevant clinicopathological factors were
recorded, including: age, FIGO stage, pathological type (squamous cell
carcinoma/adenocarcinoma), HPV typing, lymph-vascular space involvement (LVSI),
squamous cell carcinoma antigen (SCCA) value (normal value
(1) SPSS 23.0 (IBM Corporation, Armonk, NY, USA) statistical analysis software
was used. Quantitative data were expressed as mean
(2) MedCalc Statistical Software version 20.113 (MedCalc Software bv, Ostend, Belgium) was used. The area under the receiver operating characreristic (ROC) curve of the maximum, mean and minimum values of elastic modulus were compared in order to determine the best diagnostic cut-off point, sensitivity, specificity, Youden index, positive likelihood ratio and negative likelihood ratio respectively. The diagnostic cut-off point of elastic modulus value and its corresponding sensitivity and specificity were dynamically observed by MedCalc software.
The comparative analysis of cervical elasticity values in the three groups
showed that the mean, maximum and minimum values of elastic modulus in cervical
cancer group were the maximum (Table 1). The elastic modulus of cervical cancer
group and CIN group, cervical cancer group and cervicitis group were compared.
The differences were statistically significant (p
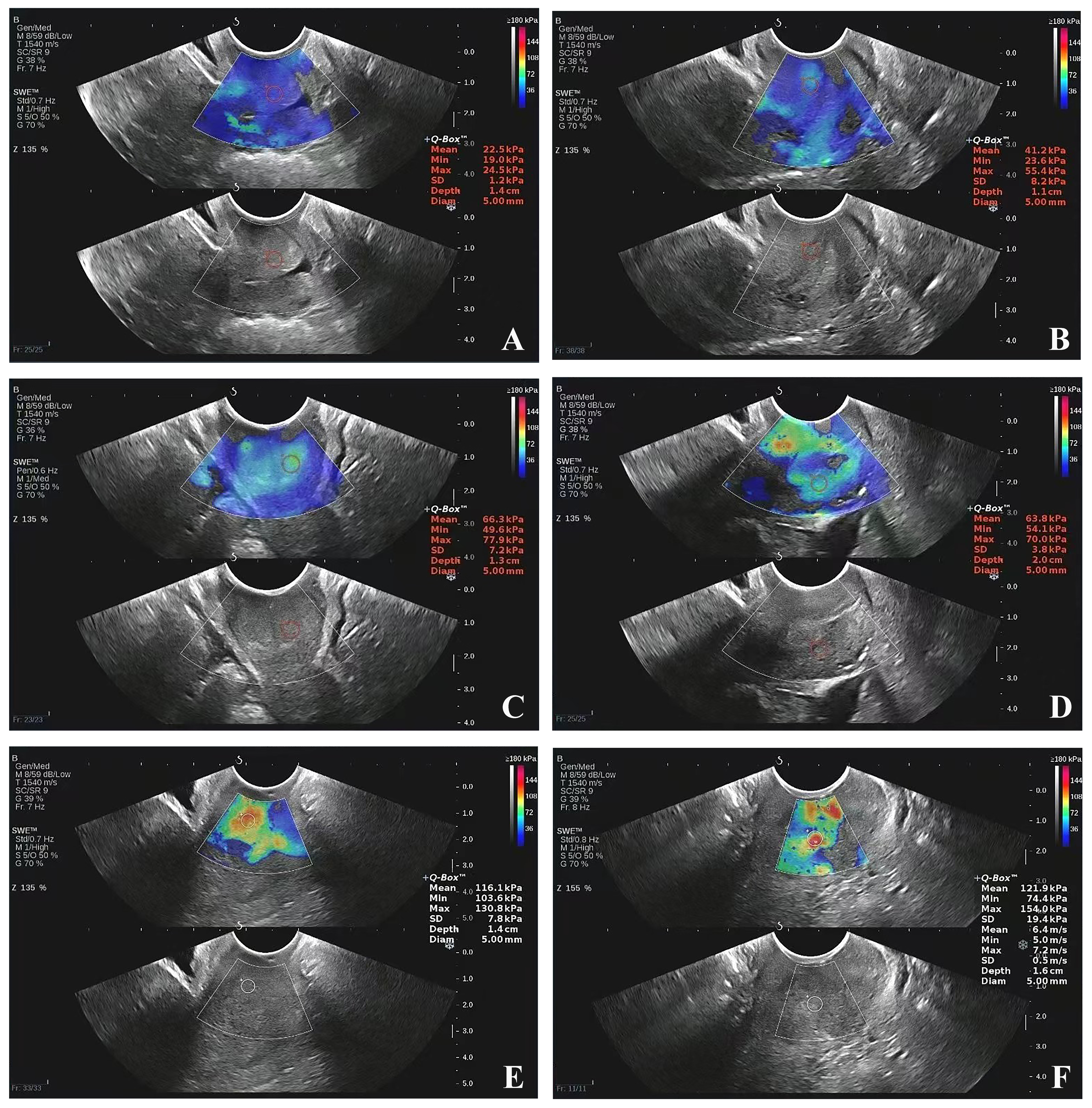 Fig. 1.
Fig. 1.
Representative SWE images of the three groups. (A,B) Cervicitis group, (C,D) CIN group, (E,F) Cervical cancer group. SWE, shear wave elastography; CIN, cervical intraepithelial neoplasia.
| Groups | n | Maximum value | Minimum value | Mean value |
| Cervical cancer group | 87 | 102.60 |
68.66 |
88.38 |
| CIN group | 40 | 65.64 |
41.40 |
53.70 |
| Cervicitis group | 40 | 60.20 |
38.35 |
49.53 |
| H | 84.32 | 69.78 | 90.53 | |
| p |
CIN, cervical intraepithelial neoplasia; H, Kruskal-Wallis H.
| Comparison | Maximum value | Minimum value | Mean value |
| Cervicitis group vs. CIN group | 0.272 | 0.396 | 0.524 |
| Cervical cancer group vs. CIN group | |||
| Cervical cancer group vs. Cervicitis group |
CIN, cervical intraepithelial neoplasia.
The area under the ROC curve of the mean, maximum and minimum values of elastic
modulus in the diagnosis of cervical cancer was 0.925, 0.909 and 0.873,
respectively (Table 3). After pairwise comparison, just the difference between
the mean value and the minimum value was statistically significant (Z = 2.725,
p
| Elastic modulus | The area under the ROC curve | Standard error | 95% Confidence interval |
| Mean value | 0.925 | 0.020 | 0.874, 0.960 |
| Maximum value | 0.909 | 0.022 | 0.855, 0.948 |
| Minimum value | 0.873 | 0.027 | 0.813, 0.920 |
ROC, receiver operating characreristic.
| Comparison | Z | p |
| Mean value vs. Maximum value | 1.516 | 0.130 |
| Mean value vs. Minimum value | 2.725 | 0.006 |
| Maximum value vs. Minimum value | 1.398 | 0.162 |
The positive likelihood ratios of the mean value and the maximum value were
21.74 and 19.97, respectively (both
| Elastic modulus | Sensitivity (%) | Specificity (%) | Best diagnostic cut-off point (kPa) | Youden index | Positive likelihood ratio | Negative likelihood ratio |
| Mean value | 82.8 | 96.2 | 66.5 | 0.79 | 21.74 | 0.18 |
| Maximum value | 75.9 | 96.2 | 82.2 | 0.72 | 19.97 | 0.25 |
| Minimum value | 82.8 | 78.7 | 48.5 | 0.62 | 3.89 | 0.22 |
Based on the principle of minimizing the rate of missed diagnosis, the changes of sensitivity and specificity could be observed by dynamically changing the diagnostic cut-off point (Fig. 2).
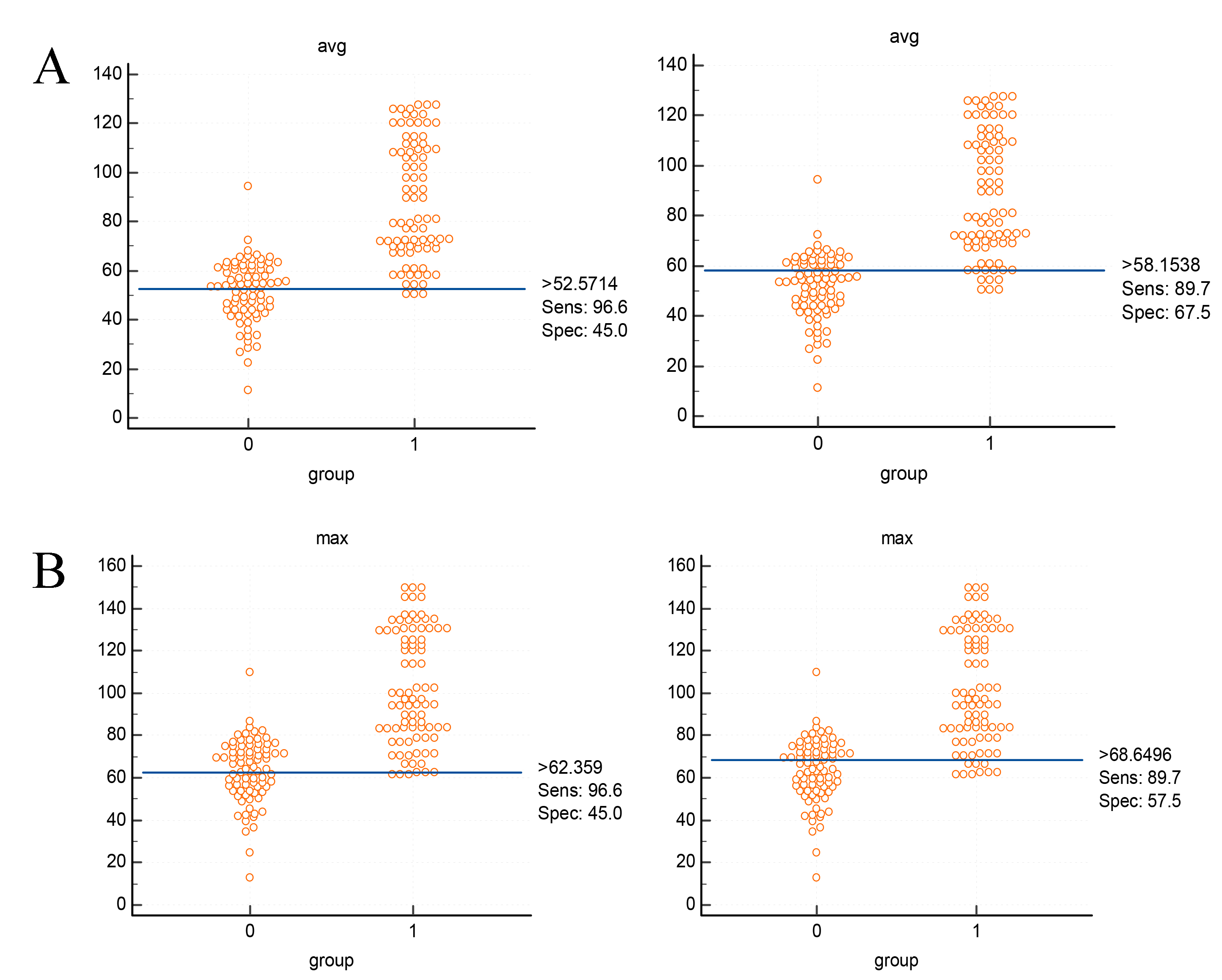 Fig. 2.
Fig. 2.
The sensitivity and specificity of the mean value and the maximum value of the elastic modulus after the change of the diagnostic cut-off point. (A) Mean value, (B) Maximum value.
The clinical data of 36 patients in the cervical cancer group were analyzed. The
age ranged from 29 to 73 years, of which 3 patients were more than 70 years old,
and the median age was 53 years. According to FIGO staging, there were 5 cases in
stage ⅠA, 7 cases in stage ⅠB, 7 cases in stage ⅡA, 9 cases in stage ⅡB, 7 cases
in stage Ⅲ, and 1 case in stage Ⅳ. The mean, maximum and minimum values were
statistically different according to different FIGO stages and tumor lesion size
(p
| Factors | Comparison (n = 36) | Mean value | Maximum value | Minimum value |
| FIGO stage | I (n = 12) | 67.64 |
80.45 |
51.34 |
| II (n = 16) | 84.76 |
97.04 |
68.61 | |
| III-IV (n = 8) | 109.64 |
125.79 |
83.50 | |
| p | 0.004 | 0.005 | 0.020 | |
| Lesion size | 62.47 |
73.33 |
48.61 | |
| 85.40 |
99.56 |
64.87 | ||
| 98.04 |
112.15 |
78.64 | ||
| p | 0.016 | 0.021 | 0.025 | |
| Types of pathology | Adenocarcinoma (n = 3) | 62.03 |
69.40 |
51.83 |
| Squamous cell carcinoma (n = 33) | 86.63 |
100.49 |
67.46 | |
| p | 0.114 | 0.077 | 0.347 | |
| HPV typing | 16/18 positive (n = 15) | 83.91 |
98.13 |
63.30 |
| Others (n = 21) | 85.06 |
97.74 |
66.78 | |
| p | 0.903 | 0.970 | 0.864 | |
| Initial treatment | Radical resection (n = 23) | 80.50 |
94.50 |
60.89 |
| Radiation therapy (n = 13) | 91.80 |
103.91 |
75.49 | |
| p | 0.234 | 0.376 | 0.091 | |
| SCCA | 73.75 |
85.51 |
56.32 | |
| 92.32 |
106.75 |
73.19 | ||
| p | 0.062 | 0.035 | 0.043 | |
| LVSI | Negative (n = 26) | 79.10 |
90.26 |
64.18 |
| Positive (n = 10) | 98.83 |
117.77 |
71.31 | |
| p | 0.049 | 0.012 | 0.449 |
FIGO, International Federation of Gynecology and Obstetrics; HPV, human papillomavirus; SCCA, squamous cell carcinoma antigen; LVSI, lymph-vascular space involvement.
Among the 13 patients with cervical cancer who were initially treated with
radiotherapy and did not undergo surgery, 7 patients underwent the measurement of
cervical elastic modulus after radiotherapy. The results revealed that the mean,
maximum and minimum values of elastic modulus before radiotherapy were
significantly higher than those after radiotherapy, and the differences were
statistically significant (p
| Comparison | Mean value | Maximum value | Minimum value |
| Before radiotherapy | 92.71 |
107.41 |
74.94 |
| After radiotherapy | 57.60 |
67.97 |
43.01 |
| p | 0.017 | 0.005 | 0.037 |
In 2010, Sebag et al. [16] first reported the use of SWE in the diagnosis of thyroid cancer, which made quantitative assessment of tissue stiffness possible. With different hardness, the quantitative value of elasticity is different. SWE technology is a major advance of ultrasound elastography technology, which can directly quantify the tissue hardness with the results being more objective [12]. At present, SWE, as a quantitative examination technique, analyzes tissue stiffness by measuring the elastic modulus value of tissue, and is widely used in the screening and efficacy evaluation of thyroid cancer [17], breast cancer [18], prostate cancer [19, 20] and other tumors. Some scholars have pointed out that elastography improves the ability of ultrasound to differentiate benign and malignant breast lesions, thereby reducing the number of biopsies of benign breast nodules [21].
SWE technology has potential in the research of cervix pathology, and its non-invasiveness and repeatability are favored by clinicians [22, 23]. Regarding repeatability, relevant studies have pointed out that it is affected by the expertise of the examiners, especially as some experience is required to obtain reproducible results [24, 25]. It is currently believed that if performed by an experienced sonographer, ultrasound can provide the same diagnostic accuracy as magnetic resonance imaging (MRI) [26]. How to overcome the differences in measurement values between different machines and different sonographers may be a further difficulty to be overcome in the future clinical application of this examination technology. For accuracy, it is necessary to improve the machine measurement and strengthen the training of sonographers.
In this study, it was found that the maximum, minimum and mean elastic modulus
of the cervical cancer group were significantly different from those of the
cervicitis group and the CIN group (p
Taking pathology as the gold standard, this study evaluated the application
value of SWE technology in cervical cancer and determined its accuracy. In this
study, the area under the ROC curve of the mean value was the largest, followed
by the maximum value, and the minimum value being the smallest. For the commonly
used indicators of accuracy evaluation, the positive likelihood ratios of the
mean, maximum and minimum values were 21.74, 19.97 and 3.89, respectively, and
the negative likelihood ratios of the mean, maximum and minimum values were 0.18,
0.25 and 0.22, respectively. Based on statistics, it is generally believed that
the positive likelihood ratio
The optimal cut-off point of the maximum elastic modulus was 82.2 kPa, with a sensitivity of 75.9% and a specificity of 96.2%. The optimal cut-off point of the mean value of elastic modulus was 66.5 kPa, with a sensitivity of 82.8% and a specificity of 96.2%. Clinically, if the best diagnostic cut-off point was used as the cut-off value to diagnose cervical cancer, compared with the original data and patient data, we found that the maximum value was less than 82.2 kPa in 3 patients with cervical cancer, and the mean value was less than 66.5 kPa in 1 patient with cervical cancer. After changing the diagnostic cut-off point dynamically, changes of sensitivity and specificity could be observed. The rate of missed diagnosis decreased, but the specificity also decreased. When the cut-off point of the maximum value was 68.6 kPa, the sensitivity increased to 89.7%, and when the cut-off point of the maximum value was 62.4 kPa, the sensitivity increased to 96.6%. When the diagnostic cut-off point of the mean value decreased to 58.2 kPa, the sensitivity increased to 89.7%, and when the diagnostic cut-off point of the mean value decreased to 52.6 kPa, the sensitivity increased to 96.6% (Fig. 2). Therefore, based on an auxiliary screening examination technology, for the purpose of early detection, early diagnosis and early treatment, reducing the diagnostic cut-off point in clinical application can reduce the rate of missed diagnosis. In conclusion, we suggest that when SWE technology is applied to the clinical screening of cervical cancer patients, it may be more suitable to consider the appropriate reduction of the diagnostic cut-off point (i.e., the appropriate reduction of the elastic modulus value). Before the actual application in clinical practice, we will increase the sample size and correlation analysis to make the results more meaningful.
This study attempted to further analyze the relationship between cervical
stiffness and the clinicopathological factors. The results of statistical
analysis showed that there were statistically significant differences according
to different FIGO stages and tumor lesion size, but there was no statistically
significant difference according to pathological type. The analysis may be
related to the fact that only 3 patients with cervical adenocarcinoma had
complete data, so the number of cases was quite small. In the future, if we
increase the sample size of patients with cervical adenocarcinoma, the estimated
results may be different. As can be seen from Table 6, as the tumor lesions
gradually increased, according to the tumor size (
In addition, the significance of SWE technology in staging is also reflected in the following two points: first, with the increase of FIGO stage, the elasticity value of cervical stiffness gradually increased (Table 6), and the difference was statistically significant; second, we found that patients with advanced cervical cancer have higher SCCA values and are more likely to have LVSI positivity. As shown in Table 6, according to whether SCCA is abnormal or not, the maximum value and the minimum value are statistically significant. According to whether LVSI is positive or not, the maximum value and the mean value are also statistically significant, which further illustrates the research value of SWE technology in clinical staging. As for the exploration of SWE technology in the clinical staging of cervical cancer, we need further clinical research in order to achieve the purpose of improving the accuracy of clinical staging of cervical cancer prior to surgery and guiding clinical treatment [28].
In this study, the elastic values of 7 patients with cervical cancer were measured before and after radiotherapy. It can be seen that the elastic values after radiotherapy were significantly lower than those before radiotherapy, and the differences before and after radiotherapy were statistically significant. This supports that SWE technology also has clinical guiding significance and application value in the treatment of cervical cancer, which supports research in increasing the sample size and performing further in-depth exploration.
The research value of SWE technology in clinical staging and treatment of cervical cancer, including radiotherapy needs to be further evaluated. In addition, whether prognosis is also related to stiffness will be one of our focuses in future research.
SWE technology has an application value in the detection of cervical cancer. The mean and maximum values have higher diagnostic accuracy. SWE technology also has potential clinical application value in the clinical staging and treatment of cervical cancer, but further studies with larger sample sizes are needed.
All SWE data measured in this paper are stored in the ultrasound room machine of our hospital, and further enquiries can be directed to the corresponding author.
LC designed the study and wrote the manuscript. PS was the primary operator of the SWE technique. XL, WD and MW participated in data collection and supervision. All authors have read and approved the final manuscript. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This study was approved and informed consent was adopted by the institutional review board of Affiliated Hospital of Xuzhou Medical University (number: XYFY2020-KL154-01).
We would like to thank our colleagues in the outpatient department and medical records room for their help. We would like to express our gratitude to all those who helped us during the writing of this manuscript. Thanks to all the peer reviewers for their opinions and suggestions.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.


