1 Department of Obstetrics & Gynecology, College of Medicine, King Saud University, 12372 Riyadh, Saudi Arabia
2 Department of Obstetrics & Gynecology, King Abdullah Medical Complex, 23816 Jeddah, Saudi Arabia
Abstract
Urinary incontinence (UI) significantly affects women’s quality of life globally. Mid-urethral sling (MUS) procedures are common minimally invasive surgeries for treating stress urinary incontinence (SUI) and mixed urinary incontinence (MUI), but comparative outcome studies, especially regarding complication rates, are lacking. The purpose of this study was to assess and compare the efficacy and safety of the retropubic tension-free vaginal tape (TVT) and transobturator tape (TOT) approaches in treating SUI and MUI. The study also aimed to investigate predictive factors for intraoperative and postoperative complications.
A retrospective cohort study was conducted at King Saud University Medical City from February 2016 to October 2022, involving 166 women who underwent either TVT or TOT surgeries. Data were collected on intraoperative and postoperative complications, with statistical analyses performed using chi-square tests and multivariate regression to identify significant predictors of morbidity.
The study included 166 patients who underwent MUS procedures, with 61% (n = 102) undergoing retropubic TVT and 39% (n = 64) undergoing TOT surgeries. The demographic characteristics were similar between the groups, with no significant differences in age (p = 0.559), body mass index (BMI) (p = 0.600), or presence of cystocele (p = 0.912). The TVT group experienced a significantly higher rate of intraoperative bladder/urethral perforation compared to the TOT group (9.8% vs. 0%, p = 0.008). Early postoperative complications, including urinary retention, were comparable between the groups (TVT: 10.8%, TOT: 12.5%, p = 0.600). Patients in the TOT group had shorter hospital stays, with 71.9% discharged within one day compared to 41.2% in the TVT group (p < 0.001). At long-term follow-up (>6 months), both groups reported high satisfaction, with 93.7% of TVT and 87.3% of TOT patients reporting good or very good comfort (p = 0.252). However, pain-free status was significantly higher in the TVT group (91.1% vs. 67.2%, p < 0.001). Both retropubic and transobturator MUS techniques are effective for managing SUI, with the transobturator approach showing fewer complications and shorter recovery times.
Both retropubic and transobturator MUS techniques are effective for managing SUI, with the transobturator approach showing fewer complications and shorter recovery times. We recommend the formation of a national registry to track long-term outcomes and enhance procedural evidence.
Keywords
- stress urinary incontinence
- mid-urethral sling
- retropubic
- transobturator
- surgical outcomes
- urinary incontinence
Urinary incontinence (UI) is a common health problem that significantly impacts the quality of women’s lives, including physical, psychological, and social wellbeing. Most studies report a UI prevalence of about 25% in young women, 44–57% in middle-aged and postmenopausal women, and 75% of older women [1]. Most women complain of stress urinary incontinence (SUI) which represents a percentage of 50–88% [1]. In Saudi Arabia, the prevalence of urinary incontinence was estimated to be 44.2% [2]. UI can take several different forms with varying pathologic pathways & therefore require different management methods. According to the American College of Obstetricians and Gynecologists (ACOG) [1], SUI is defined as the involuntary loss of urine on effort, physical exertion, sneezing, or coughing. In urge urinary incontinence (UUI) women have an involuntary loss of urine associated with a sudden compelling urge to void. Mixed urinary incontinence (MUI) includes both stress and urge incontinence symptoms and signs. Among all risk factors, obesity and being overweight was found to be one of the most significant risks leading to UI [3]. Several studies highlighted important risk factors that may be associated with SUI including pregnancy and mode of delivery [4], smoking, ethnicity, hormonal replacement therapy and other comorbidities (i.e., depression, diabetes) [5].
Typically, the first line of management for SUI is conservative treatment and usually involves pelvic floor muscle training and biofeedback physical therapy which are mainly used in mild cases of UI [3, 6]. Possibly due to patient hesitancy, many women seek medical advice in more advanced stages of urinary incontinence. In conditions where conservative treatment does not succeed or is not feasible, there are multiple minimally invasive procedures currently available for the treatment of SUI and they include; mid-urethral slings (MUS), bladder neck slings and the Burch colposuspension [1]. Other minimally invasive treatments available include: urethral bulking injections procedures, electrical stimulation of pelvic floor, Electroacupuncture & Pulsed magnetic stimulation [7, 8, 9]. The MUS is the gold standard for treatment of stress urinary incontinence [10], due to their high success rates, less invasive nature and lower complication rates [11]. Commonly women with MUI are treated with a similar approach to SUI [12].
In 1995, Ulmsten and Petros [13] proposed a new method built on previous experimental and clinical studies & thus established the retropubic tension-free vaginal tape. In 2001, Delorme [14] introduced an alternative method using an inside-out transobturator tape procedure through the groin. With the introduction of these procedures concerns were raised regarding a lack of evidence in the literature addressing long term morbidity post implantation of vaginal mesh [15, 16]. In the literature, most publications focus on efficacy & short term morbidity with the evidence suggesting a positive impact on women’s lives [17]. Apart from groin pain less adverse outcomes are reported with a transobturator route when compared with the retropubic approach [11, 18]. Complications such as vascular or bladder injuries, intra operative blood loss, operating time and length of hospital stay were less frequent with the transobturator approach [11, 19, 20].
To our knowledge, there have been no published studies designed to address the incidence and nature of complications of retropubic and transobturator procedures in Saudi Arabia. The aim of our study is to determine the efficacy of MUS and to delineate the predictive factors for intraoperative and postoperative morbidity among women diagnosed with SUI and MUI. Additionally, another objective of the study is to compare both approaches in terms of outcome & complications.
Ethical approval was obtained from the Internal review board of King Saud University (KSU), Riyadh, Saudi Arabia (E-23-7864). Informed written consent was obtained from all study participants. The study was a retrospective cohort comparing retorpubic and transobturator MUS for the treatment of SUI. A chart review of all patients who underwent a MUS procedure in King Saud University Medical City (KSUMC) from February 2016 until October 2022 was conducted.
Inclusion criteria included patients diagnosed with stress urinary incontinence confirmed with a urodynamic exam, those who underwent retropubic or transobturator surgery and completed a clinical follow up postoperatively, not being pregnant, not using immunosuppressive and steroid medication, did not receive chemotherapy & radiotherapy less than 3 months prior to surgery, not diagnosed with cirrhosis, clinical collagen defects, thrombocytopenia, infections, chronic renal failure, and mental illness. The exclusion criteria were lack of follow-up or the patients desire to end participation, stress urinary incontinence with a negative urodynamic exam and pure urge urinary incontinence.
Preoperative assessment included a comprehensive medical history & examination including a cough stress test, and urodynamic assessment. The main goal from the preoperative assessment was to confirm the diagnosis of stress urinary incontinence objectively.
A total of 166 patients were eligible for participation in the study. They were divided into 2 groups, the “retropubic” group (n = 102) and the “transobturator” group (n = 64) based on the surgeons preference, comfort and familiarity with the procedure. The follow-up appointments were planned for less than 6 months and more than 6 months after surgery. The variables collected consisted of intraoperative complications such as hematoma, intraoperative mucosal erosion, bladder perforation and postoperative complications such as postoperative groin pain, mesh erosion, urinary retention, long term catheterization and recurrent UI. These variables were analysed as adverse outcomes of MUS. Fig. 1 illustrates the study participants and groups. At the postoperative appointment evaluation of comfort/discomfort, assessment of pain, and recurrence of urinary incontinence were ascertained with a comprehensive interview by one of the team members.
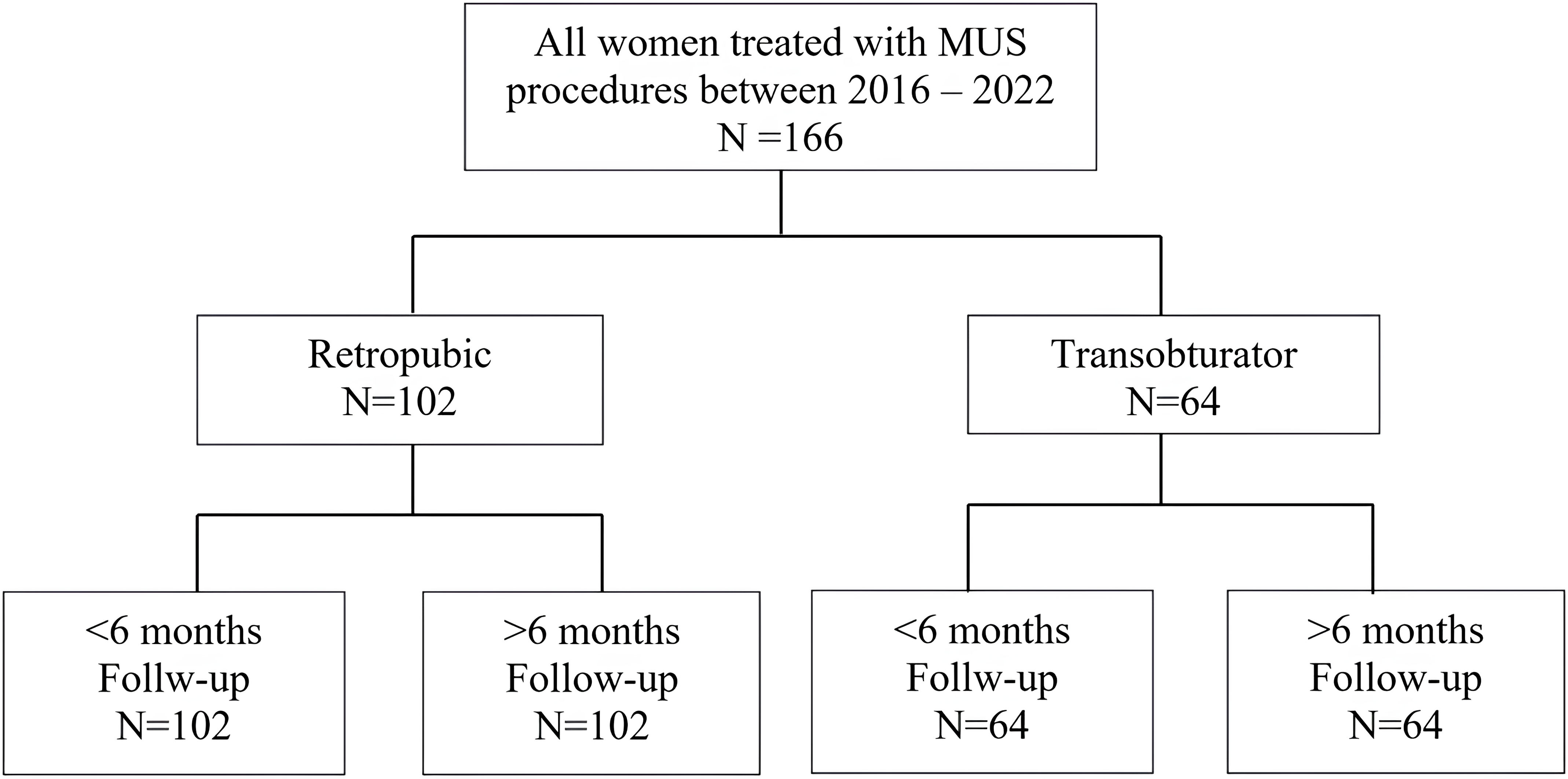 Fig. 1.
Fig. 1.
Flow chart for study follow-up. A flow chart of the study participants, showing the total number of patients and their division into the groups. MUS, mid-urethral sling.
All procedures were performed by urogynecology surgeons who received speciality training in urogynecology and have between 16–20 years of experience, the route of MUS (retropubic vs. transobturator) was chosen based on the surgeons’ preference. The implant used in all retropubic procedures was the polypropylene GYNECARE TVT EXACT ® Continence System (830041B, Ethicon, Bridgewater, NJ, USA) whereas the GYNECARE TVT ™ Obturator system (810081L, Ethicon, Bridgewater, NJ, USA) was used for the transobturator route.
Statistical analysis was done using the Statistical Packages for Software Sciences (SPSS) version 26 (IBM Corporation, Armonk, NY, USA). Descriptive statistics were presented as numbers and percentages (%) for all categorical variables. A Chi-square test was used to demonstrate the relationship between the type of surgery and postoperative characteristics of patients. Based on the significant results, a multivariate regression analysis was performed to determine the significant independent morbidity predictors of the MUS procedure, with a corresponding odds ratio and 95% confidence interval. Values were considered significant with a p-value of less than 0.05.
During the study period, a total of 166 women underwent MUS surgery at KSUMC. Sixty-one percent (N = 102) of women had a retropubic procedure while 39% (n = 64) of women were operated on with a transobturator approach Fig. 1. The patients baseline sociodemographic, preoperative and primary diagnosis characteristics are outlined in Table 1. There were no significant differences between the 2 groups regarding age (p = 0.559), body mass index (BMI) (p = 0.600), presence of cystocele (p = 0.912), or medical history (p = 0.298).
| Factor | Retropubic N (%) | Transobturator N (%) | p-value§ | ||
| N = 102 | N = 64 | ||||
| Age group | |||||
| 41 (40.2%) | 30 (46.9%) | 1.162 | 0.559 | ||
| 37 (36.3%) | 23 (35.9%) | ||||
| 24 (23.5%) | 11 (17.2%) | ||||
| BMI | |||||
| 8 (7.8%) | 9 (14.1%) | 2.751 | 0.600 | ||
| 38 (37.3%) | 20 (31.3%) | ||||
| 33 (32.4%) | 24 (37.5%) | ||||
| 17 (16.7%) | 8 (12.5%) | ||||
| 6 (5.9%) | 3 (4.7%) | ||||
| Cystocele presence | |||||
| 82 (80.4%) | 51 (79.7%) | 0.012 | 0.912 | ||
| 20 (19.6%) | 13 (20.3%) | ||||
| Medical history | |||||
| 62 (60.8%) | 44 (68.8%) | 1.081 | 0.298 | ||
| 40 (39.2%) | 20 (31.3%) | ||||
| Medical history | |||||
| 37 (36.3%) | 25 (39.1%) | 0.131 | 0.718 | ||
| 24 (23.5%) | 22 (34.4%) | 2.309 | 0.129 | ||
| 22 (21.6%) | 25 (39.1%) | 5.929 | 0.015 ** | ||
| 3 (2.9%) | 5 (7.8%) | 2.034 | 0.263 | ||
| 3 (2.9%) | 0 | 1.917 | 0.285 | ||
| 5 (4.9%) | 2 (3.1%) | 0.307 | 0.579 | ||
| 0 | 1 (1.6%) | 1.603 | 0.386 | ||
| Mixed urinary incontinence (MUI) | |||||
| 73 (71.6%) | 36 (56.3%) | 4.093 | 0.043 ** | ||
| 29 (28.4%) | 28 (43.8%) | ||||
| Stress urinary incontinence | |||||
| 100 (98.0%) | 58 (90.6%) | 1.270 | 0.402 | ||
| 14 (13.7%) | 6 (9.4%) | ||||
| Positive cough test prior to surgery | |||||
| 70 (68.6%) | 56 (87.5%) | 7.658 | 0.006 ** | ||
| 32 (31.4%) | 8 (12.5%) | ||||
§p-value has been calculated using the Chi-square
test; ** Significant at p
The patients’ medical histories included diabetes, hypertension, overactive bladder syndrome, depression, neurosis, spinal degeneration, and prior hysterectomy surgery Fig. 2. The most frequent comorbidity in our study population was diabetes with 37.3%.
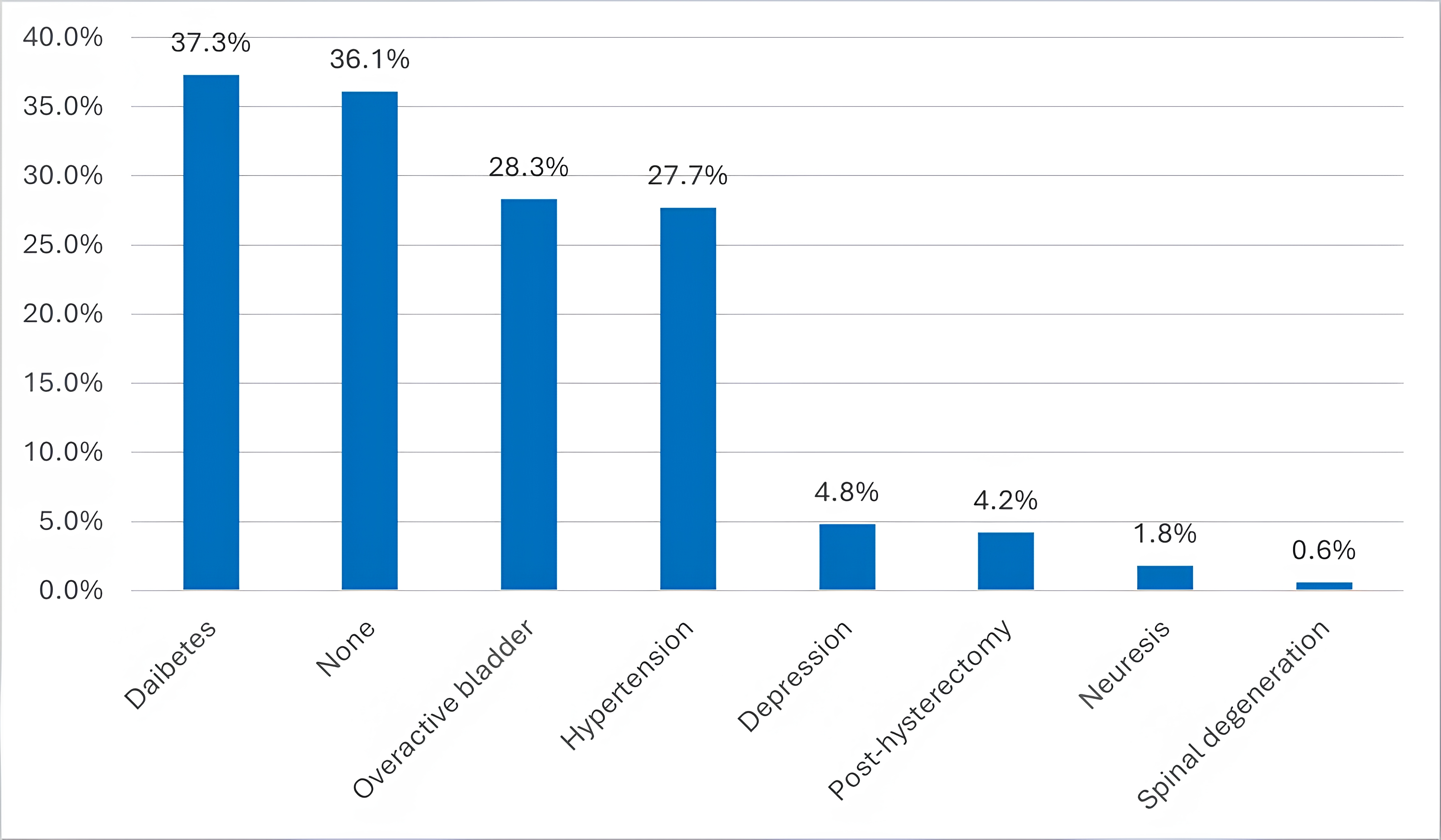 Fig. 2.
Fig. 2.
Patients medical history. This bar chart shows the most frequently encountered comorbidities in our study population.
Intraoperative and early postoperative complications and the length of
hospitalization are demonstrated in Table 2. The retropubic group had a higher
incidence of bladder/urethral perforation (9.8% vs. 0%, p =
0.008) and a longer average hospital stay compared to the transobturator group,
where more patients were discharged within one day (71.9% vs. 41.2%,
p
| Factor | Retropubic N (%) | Transobturator N (%) | p-value§ | ||
| N = 102 | N = 64 | ||||
| Intraoperative complications | |||||
| 89 (87.3%) | 64 (100%) | 8.850 | 0.031 ** | ||
| 2 (2.0%) | 0 | ||||
| 1 (1.0%) | 0 | ||||
| 10 (9.8%) | 0 | ||||
| Average length of hospital stay | |||||
| 42 (41.2%) | 46 (71.9%) | 14.878 | |||
| 60 (58.8%) | 18 (28.1%) | ||||
§p-value has been calculated using the Chi-square
test; ** Significant at p
To evaluate patient discomfort after surgery, a five-point pain scale was used, where 1 represents no feeling of pain & 5 indicates intense pain, most patients in the study stated an average pain score of 1.
Clinical outcomes for both groups are summarized in Table 3, categorized by follow-up appointments at less than 6 months and more than 6 months post-surgery. At the first postoperative appointment, 90 patients (88.2%) in the retropubic group reported satisfaction with the procedure, though 12 patients (11.8%) were dissatisfied. De novo urgency and recurrent SUI were noted in 22 (21.6%) and 20 (19.6%) of these patients, respectively. During the second follow-up for the retropubic group, 89 patients (93.7%) reported good comfort and free voiding. In contrast, the transobturator group showed higher overall satisfaction and lower incidence of pain and urinary symptoms at both follow-up periods.
| Factor | Retropubic N (%) | Transobturator N (%) | p-value§ | ||
| N = 102 | N = 64 | ||||
| Comfort after surgery | |||||
| 12 (11.8%) | 3 (4.7%) | 2.396 | 0.166 | ||
| 90 (88.2%) | 61 (95.3%) | ||||
| Sense of pain* | |||||
| 82 (80.4%) | 38 (59.4%) | 9.725 | 0.008 ** | ||
| 14 (13.7%) | 21 (32.8%) | ||||
| 5 (5.0%) | 5 (7.8%) | ||||
| 0 | 0 | ||||
| Recurrent urinary incontinence | |||||
| 20 (19.6%) | 4 (6.3%) | 5.674 | 0.022 ** | ||
| 82 (80.4%) | 60 (93.8%) | ||||
| Other adverse effects De novo urgency | |||||
| 22 (21.6%) | 10 (15.6%) | 0.893 | 0.345 | ||
| 80 (78.4%) | 54 (84.4%) | ||||
| Groin/pelvic pain | |||||
| 15 (14.7%) | 17 (26.6%) | 3.553 | 0.059 | ||
| 87 (85.3%) | 47 (73.4%) | ||||
| Long term catheterization | |||||
| 1 (1.0%) | 0 | 0.631 | 1.000 | ||
| 101 (99.0%) | 64 (100%) | ||||
| Pain during micturition | |||||
| 7 (6.9%) | 15 (23.4%) | 9.397 | 0.002 ** | ||
| 95 (93.1%) | 49 (76.6%) | ||||
| Comfort after surgery | |||||
| 6 (5.9%) | 8 (12.5%) | 1.455 | 0.228 | ||
| 96 (94.1%) | 56 (87.5%) | ||||
| Sense of pain* | |||||
| 92 (91.1%) | 43 (67.2%) | 16.308 | |||
| 9 (8.9%) | 18 (28.1%) | ||||
| 0 | 3 (4.7%) | ||||
| 0 | 0 | ||||
| Recurrent urinary incontinence | |||||
| 13 (12.7%) | 13 (20.3%) | 1.705 | 0.192 | ||
| 89 (87.3%) | 51 (79.7%) | ||||
| De novo urgency | |||||
| 24 (23.5%) | 15 (23.4%) | 0.000 | 0.989 | ||
| 78 (76.5%) | 49 (76.6%) | ||||
| Overactive bladder | |||||
| 30 (29.4%) | 25 (39.1%) | 1.653 | 0.199 | ||
| 72 (70.6%) | 39 (60.9%) | ||||
| Painful sexual intercourse | |||||
| 10 (9.8%) | 8 (12.5%) | 0.587 | 0.587 | ||
| 92 (90.2%) | 56 (87.5%) | ||||
| Mesh erosion | |||||
| 7 (6.9%) | 3 (4.7%) | 0.329 | 0.566 | ||
| 95 (93.1%) | 61 (95.3%) | ||||
| Need for surgical release | |||||
| 8 (7.8%) | 3 (4.7%) | 0.633 | 0.426 | ||
| 94 (92.2%) | 61 (95.3%) | ||||
| Need for another incontinence surgery | |||||
| 3 (2.9%) | 0 | 1.917 | 0.285 | ||
| 99 (97.1%) | 64 (100.0%) | ||||
*sense of pain data for one patient was missing & was excluded from the
analysis; §p-value has been calculated using the
Chi-square test; ** Significant at p
In the early postoperative period (less than 6 months), the retropubic group experienced significantly more pain during micturition compared to the transobturator group (p = 0.002). Additionally, recurrent urinary incontinence was more frequently reported in the retropubic group at the 6-month follow-up (19.6% vs. 6.3%, p = 0.022).
Table 4 shows important predictors of postoperative morbidity in patients undergoing MUS procedures. The multivariate regression analysis suggests that patients with certain preoperative characteristics, such as a positive cough test, tend to fare better, whereas those with prolonged pain, longer hospital stays, or recurrent incontinence after surgery are at a higher risk for complications.
| Factor | S.E. | AOR | 95% CI | p-value§ | ||
| Overactive bladder | ||||||
| –0.811 | 0.362 | 0.445 | 0.219–0.904 | 0.025** | ||
| Mixed urinary incontinence (MUI) | ||||||
| 0.307 | 0.384 | 1.360 | 0.638–2.898 | 0.425 | ||
| Positive cough test prior to surgery | ||||||
| –1.209 | 0.491 | 0.298 | 0.114–0.779 | 0.014 ** | ||
| Pain more |
||||||
| –1.654 | 0.485 | 0.191 | 0.074–0.492 | 0.001 ** | ||
| Average length of hospital stay | ||||||
| 1.393 | 0.414 | 4.024 | 1.930–8.389 | |||
| Recurrent urinary incontinence | ||||||
| 1.299 | 0.575 | 3.659 | 1.189–11.257 | |||
Our study evaluated the efficacy and safety of MUS procedures at KSUMC from 2016 to 2022. A total of 166 MUS procedures were analyzed involving both a retropubic and transobturator approach to treat SUI. Both groups were comparable in terms of preoperative characteristics and demographics, which is crucial for unbiased outcome comparisons.
Our findings suggest similar success rates in the treatment of SUI with both surgical techniques. At less than 6 months post-surgery, the transobturator procedure demonstrated a higher success rate, with 93.8% of patients reporting no recurrence of urinary incontinence. In contrast, the retropubic procedure showed a success rate of 80.4%. Over a longer follow-up period exceeding 6 months, the retropubic approach showed an increase in effectiveness, with 87.3% of patients reporting no recurrence of urinary incontinence. However, the transobturator approach experienced a decrease in its success rate to 79.7%. These results are similar to findings from the effectiveness and cost-effectiveness of surgical treatments for women with stress urinary incontinence (ESTER) systematic review for the retropubic approach, which reported cure rates of 89.1% for retropubic and 64.1% for transobturator slings from an analysis of 102 different studies [21]. Furthermore, Bostanci et al. [22], estimated that the cure rate of transobturator was 68.7%. Another study indicated that the failure rate of the retropubic approach is 30% [23]. The differences noted in the transobturator tape (TOT) procedure could be due to the fact that the study was conducted at a tertiary center with extensive experience in urogynecology, which may have contributed to the high success rates and low complication rates observed. The specialized care available at KSUMC likely provided optimal conditions for both surgical techniques. All procedures were performed by experienced urogynecology surgeons. The choice of surgical technique often depended on the surgeon’s preference and expertise, which could have influenced the outcomes. Surgeons’ familiarity with and preference for specific techniques may result in better outcomes for those techniques.
Intraoperatively, the retropubic procedure required cystoscopy due to higher complication rates, a finding supported by a similar study [24]. Additionally, we found that intraoperative complications were more frequently observed with the retropubic approach than with the transobturator method. Long term complications commonly noted in recent literature such as mesh erosion were also observed [17]. However, our results revealed a reassuringly low rate of mesh complications following MUS surgery, where only 11 patients (6.6%) required surgical release (8 retropubic, 3 transobturator). Notably, the pain associated with the transobturator approach, the surgical route of which is located near the obturator canal, generally resolved within six months postoperatively. At long term follow-up, most patients reported high comfort levels and satisfaction with the surgical outcome. The reported pain scores were also very low for most patients. The incidence of recurrent SUI was similar in both groups signifying the effectiveness of both procedures.
There are several factors that may have influenced our results that are specific to the Saudi population. Being overweight and obese are significant risk factors for urinary incontinence and have a notably high prevalence in Saudi Arabia [25]. This could have had an impact on the outcome of SUI treatment in our study. Despite this, both techniques showed high efficacy which indicates the procedures are effective treatment options even in populations with high obesity rates. Our results support the continued use of MUS procedures as an effective treatment for SUI, aligning with longstanding recommendations in the urogynecological literature [26].
This study benefits from being conducted in a tertiary centre like KSUMC, with access to multiple subspecialties and extensive experience in urogynecology. All diagnoses of SUI were confirmed objectively via a urodynamic exam, and follow-up was complete for all patients, ensuring reliable data. However, limitations include the non-randomized, retrospective design and the study being conducted in a single centre, which may not represent the entire Saudi population. Additionally, the choice of surgical technique varied according to surgeon preference, and standardized measuring tools such as the 1 hour pad test or International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) were not used which could have given a more objective measure of outcome.
Our retrospective cohort study assessed the efficacy and safety of MUS procedures, for the treatment of SUI in a Saudi female population. Both retropubic and transobturator MUS techniques are effective for managing SUI, with the transobturator approach offering advantages in terms of lower complication rates and quicker recovery. Future studies could benefit from a multicentric, randomized design to further validate and expand upon our findings. We recommend the establishment of a comprehensive registry for all urological tape procedures. This would facilitate systematic follow-up visits and the collection of outcome data, thereby enhancing the evidence base regarding the long-term efficacy and safety of tape surgery.
The dataset collected and analyzed during the current study are not publicly available due to privacy and ethical restrictions as they contain confidential patient information. However, data are available from the corresponding author, Dr. Abdulrahman Bogis, on reasonable request and subject to approval by the Institutional Review Board at King Saud University, Riyadh, Saudi Arabia.
MA and GAS designed the research study. GAS, HAM and LA conducted the surgeries. DB collected the data. GAS, HAM and LA provided expertise and advice on urodynamic assessments and surgical techniques. AB analyzed the data. MA, DB, LA, HAM, AB and GAS drafted the initial manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was approved by the Institutional Review Board at King Saud University, Riyadh, Saudi Arabia (E-23-7864). The purpose and aim of the study were explained to all recruited participants, and a signed informed consent form was obtained from all patients before the study was started. Participation was voluntary and complete anonymity was ensured. All the study procedures were performed in accordance with the Declaration of Helsinki.
We gratefully acknowledge the assistance from clinical staff at King Saud University Medical City (KSUMC) for helping this study run smoothly.
This research received no external funding.
The authors declare no conflict of interest.
During the preparation of this work the authors used ChatGpt-4.0 in order to check spelling and grammar. After using this tool, the authors reviewed and edited the content as needed and takes full responsibility for the content of the publication.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.


