1 Department of Obstetrics and Gynecology, School of Medicine, Iran University of Medical Sciences, 1449614535 Tehran, Iran
2 Department of Faculty of Pharmacy, Islamic Azad University, 1941933111 Tehran, Iran
3 Endometriosis Research Center, Iran University of Medical Sciences, 1449614535 Tehran, Iran
4 Health Promotion Research Center, Zahedan University of Medical Sciences, 9816743463 Zahedan, Iran
5 Community Medicine, School of Medicine, Zahedan University of Medical Sciences, 9816743463 Zahedan, Iran
Abstract
Background: Hysteroscopy is a valuable surgical technique, but some
complications are related to cervical dilatation. Sublingual trinitroglycerin
(TNG) is a vasodilator that can facilitate cervical dilation. In our study, we
compared its effectiveness to that of misoprostol. Methods: This
randomized controlled trial study was conducted on 199 women of reproductive age
who were referred to Rasoul Akram Hospital. Patients were randomly divided into
two groups: TNG and misoprostol. Next, they were examined for clinical and
practical indicators of cervical preparation. The data was analyzed using SPSS
software. Results: Demographic characteristics exhibited no significant
differences between the groups. The mean size of the largest dilator inserted
without resistance showed not statistically significant difference between the
TNG and misoprostol groups (6.26
Keywords
- cervical ripening
- misoprostol
- hysteroscopy
- trinitroglycerin
With advancements in surgical techniques and the availability of minimally invasive procedures, the volume of outpatient surgeries has significantly increased in recent years [1]. Outpatient surgeries, including hysteroscopy, play a crucial role in women’s health care [2]. Hysteroscopy is a valuable surgical technique used to diagnose and treat cervical and intrauterine lesions. Adequate dilation of the cervix is necessary to safely and accurately access the uterine cavity with a hysteroscope, ensuring a clear view for diagnosis and therapeutic interventions [2, 3]. Cervical dilation poses a challenge for surgeons during hysteroscopy, particularly in nulliparous and menopausal patients, those with cervical stenosis, and when using a resectoscope for procedures such as myomectomy, polypectomy, removal of intrauterine septa, or excision of masses. In these cases, appropriate and sufficient cervical dilation is essential. Research on hysteroscopy has shown that complications such as pain, vasovagal reactions, and infections can be associated with cervical dilation [2, 4]. Therefore, some of the complications related to hysteroscopy can be attributed to the process of cervical dilation.
To facilitate hysteroscopy, it is important to prepare and soften the cervix beforehand. Sublingual or vaginal misoprostol can be used for this purpose [5]. Misoprostol, a prostaglandin analog, helps contract uterine smooth muscles and dilate the cervix. However, it may also induce side effects [6, 7]. When preparing for hysteroscopy, it is crucial to consider the use of drugs with minimal side effects and optimal performance. Trinitroglycerin (TNG), a vasodilator known for its proven relaxation properties, can serve this purpose effectively [8]. Study has demonstrated the positive impact of TNG on the uterus, with observations showing reduced complications and postoperative pain during patient follow-up [9].
TNG, also known as glyceryl trinitrate (GTN), is a vasodilator. It is used for various medical conditions, including heart failure, hypertension, anal fissures, dysmenorrhea (painful periods), and to treat and prevent angina (chest pain) caused by myocardial ischemia, including that resulting from a heart attack. It can be taken orally, sublingually, applied topically to the skin, or administered by intravenous injection. GTN is a prodrug that requires denitration, with the nitrite anion or a related species further reduced to produce the active metabolite nitric oxide (NO). Organic nitrates that undergo these two steps within the body are referred to as nitrovasodilators. Thus, production of NO from exogenous sources such as GTN increases the level of cyclic guanosine monophosphate (cGMP) within the cell and stimulates dephosphorylation of myosin, initiating the relaxation of smooth muscle cells in blood vessels. Misoprostol is a synthetic prostaglandin E1 analogue. It functions by reducing stomach acid secretion and increasing mucosal defenses. Additionally, it acts as a uterotonic agent, inducing smooth muscle contractions in the uterus and cervical dilation. Misoprostol is available in tablet form and can be administered vaginally, rectally, orally, or sublingually [10].
Given the widespread availability, lower costs, and low complications associated with TNG, this research aims to investigate the effects of sublingual TNG in cervical preparation and compare it to misoprostol, considering their medicinal properties.
This randomized controlled trial study was conducted on women of reproductive age who visited Rasoul Akram Hospital, Iran University of Medical Sciences, between September 2023 and January 2024. The study protocol received approval from the Ethics Committee of Iran University of Medical Sciences (code: IR.IUMS.REC.1402.180), and it was registered on the IRCT website (code: IRCT20191123045476N4). Prior to enrollment, written informed consent was obtained from all participants. A total of 199 eligible women meeting the inclusion criteria for hysteroscopy were selected (Fig. 1).
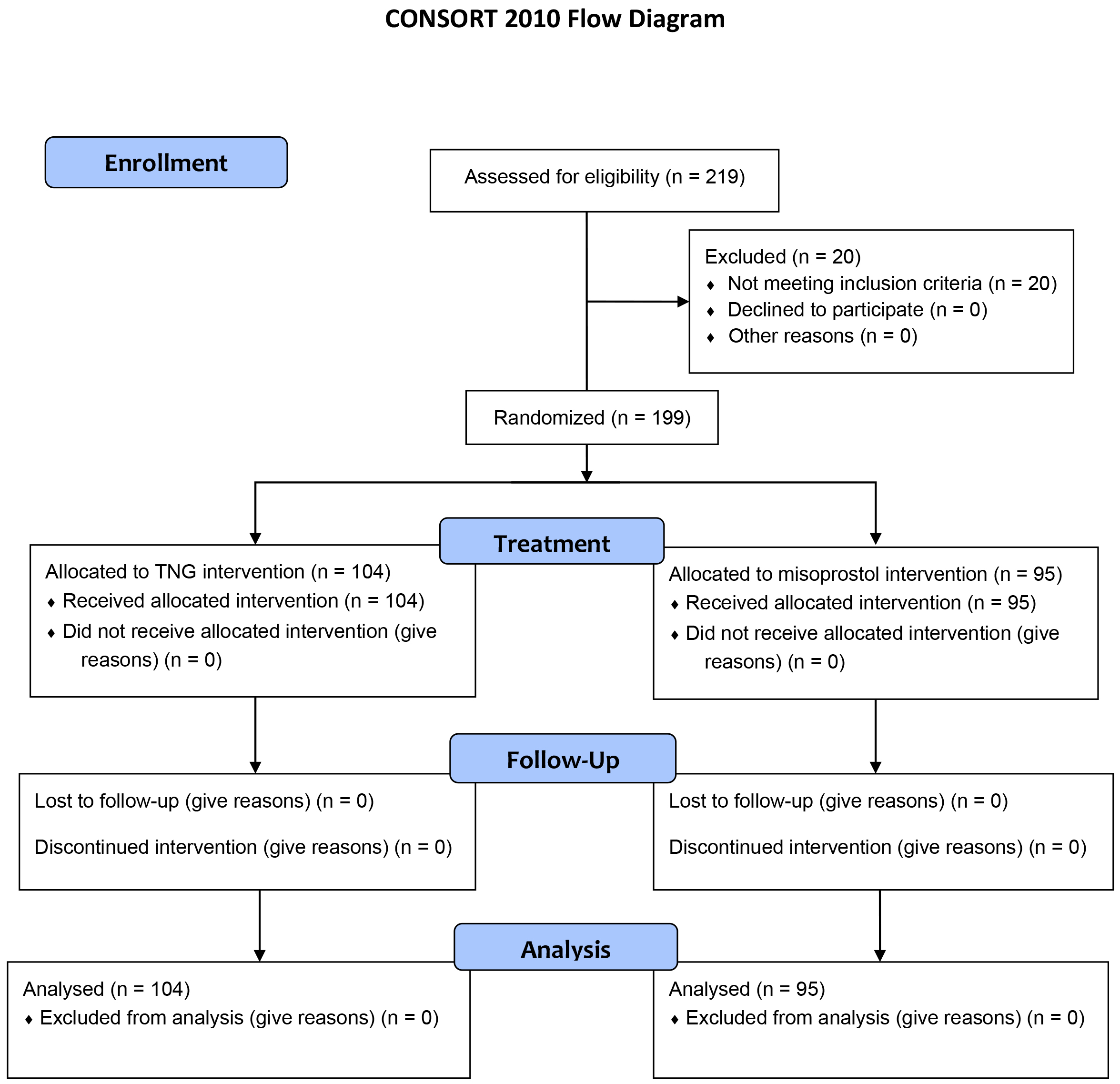 Fig. 1.
Fig. 1.Flowchart of the patients included in the studied. The patients were divided into two study groups and received TNG or misoprostol intervention. TNG, trinitroglycerin; CONSORT, consolidated standards of reporting trials.
The inclusion criteria for this study were as follows: women of reproductive age between 15 and 50 years old, informed consent from the patients, scheduling for hysteroscopy, absence of recent or current pelvic infection, no history of cervical surgery or confirmed cervical malignancy, absence of TNG sensitivity, no pre-existing heart diseases, no severe bleeding, and stable patient condition.
The exclusion criteria for this study were as follows: systolic blood pressure below 90 mm Hg, reduced intravascular volume, heart valve diseases, history of vaginal delivery, contraindication to the use of TNG as determined by the anesthesiologist, sensitivity to any preservative food colors, use of anti-hypertensive drugs, history of intracranial hemorrhage, glaucoma, hyperthyroidism, and unwillingness to participate in the study.
In this randomized controlled trial study, a type I error of 0.05, a type II error of 0.2, and an effect size of 0.41 were used to calculate the sample size for two independent groups in the t-test. The total required sample size was determined to be 190 participants, with 95 participants assigned to each group. Ultimately, 104 participants were assigned to the TNG group, while 95 participants were assigned to the misoprostol group.
The patients were divided into two groups and then randomized into 6 permutation blocks. We made six sequences; these were AABB, BBAA, ABBA, BABA, ABAB, BAAB, and we randomized them. In this randomization, group A represented TNG treatment, and group B indicated misoprostol treatment. After obtaining informed consent, group A comprised 104 patients who received general anesthesia. In the operating room, under the permission of the anesthesiologist, pearl TNG (400 µg) was administered sublingually 30 minutes before the surgery. The TNG dose was repeated every 5 minutes, up to 2 doses, when necessary [11].
For the misoprostol group (group B), consisting of 95 patients, one tablet of misoprostol (200 µg) was administered sublingually 6 hours before the surgery to avoid the complication of excessive dilatation and interfering with uterine expansion [11].
Cervical dilation was measured in both groups using calibrated dilators. Prior to transferring the patient to the operating room, potential side effects of the interventions, including abdominal cramps, vaginal bleeding, pulse, nausea, and headache, were evaluated and recorded.
The demographic data of the patients, as well as information regarding cervical dilation and side effects, were recorded using a pre-designed data collection form. Subsequently, the collected data were registered for statistical analysis.
Data analysis was conducted based on group assignment and intention-to-treat
(ITT) principles. The primary outcome of this study was dilator size and uterine
bleeding, while the secondary outcomes included drug side effects, pathology, and
variations in pulse rate and blood pressure. Student t-test,
Mann–Whitney U test, Chi-square test, and Fisher’s exact test were used to
compare basic essential and outcome variables among groups. The estimated effect
size was expressed as an odds ratio (OR) with a 95% confidence interval (95%
CI) and (r = z/
The study included 199 women with an average age of 38.18 years. The majority of women who were candidates for hysteroscopy reported abnormal uterine bleeding (n = 90, 45.2%). However, no statistically significant differences were observed between the two intervention groups for this parameter (p = 0.38). Table 1 presents the baseline characteristics of the study participants, separately for each intervention group. There were no statistically significant differences reported in age, body mass index (BMI), and remaining baseline characteristics between the two groups.
| Variable | Total | TNG Group | Misoprostol Group | p-value | |
| N = 199 | N = 104 | N = 95 | |||
| Age, years | 0.39 | ||||
| Mean (SD) | 38.18 (6.6) | 37.7 (6.5) | 38.7 (6.7) | ||
| Median (IQR) | 39.0 (9.0) | 37.5 (9.0) | 40.0 (9.0) | ||
| BMI (kg/m |
0.74 | ||||
| Mean (SD) | 26.9 (3.6) | 26.9 (3.3) | 26.8 (4.0) | ||
| Gravidity | 0.57 | ||||
| Mean (SD) | 1.34 (1.3) | 1.28 (1.3) | 1.40 (1.4) | ||
| Median (IQR) | 1 (2.0) | 1 (2.0) | 1 (2.0) | ||
| Parity | 0.19 | ||||
| Mean (SD) | 0.82 (0.9) | 0.7 (0.9) | 0.91 (0.9) | ||
| Median (IQR) | 0 (2.0) | 0 (2.0) | 1 (2.0) | ||
| History of Cesarean section (N, %) | 95 (47.7%) | 44 (42.3%) | 51 (53.7%) | 0.10 | |
| History of abortion (N, %) | 60 (30.2%) | 36 (34.6%) | 24 (25.3%) | 0.15 | |
| Past medical history (N, %) | 56 (28.1%) | 25 (24.0%) | 31 (32.6%) | 0.17 | |
| Cause of hysteroscopy (N, %) | |||||
| Diagnostic | 94 (47.2%) | 56 (53.8%) | 38 (40.0%) | 0.051 | |
| Operative | 26 (13.1%) | 15 (14.4%) | 11 (11.6%) | 0.55 | |
| Abnormal uterine bleeding | 90 (45.2%) | 44 (42.3%) | 46 (48.4%) | 0.38 | |
| Polyp | 58 (29.1%) | 27 (26.0%) | 31 (32.6%) | 0.30 | |
| Myoma | 13 (6.5%) | 6 (5.8%) | 7 (7.4%) | 0.64 | |
| Another | 4 (2.0%) | 2 (1.9%) | 2 (2.1%) | 0.65 | |
| Pulse rate before intervention | 0.06 | ||||
| Mean (SD) | 80.7 (7.1) | 80.2 (6.6) | 81.33 (7.7) | ||
| Median (IQR) | 82.0 (8.0) | 80.0 (9.0) | 82.0 (6.0) | ||
| Diastolic blood pressure before intervention | 0.99 | ||||
| Mean (SD) | 71.9 (8.4) | 72.08 (8.7) | 71.76 (8.0) | ||
| Median (IQR) | 70.0 (5.0) | 70.0 (11.0) | 70.0 (5.0) | ||
| Systolic blood pressure before intervention | 0.05 | ||||
| Mean (SD) | 113.4 (12.1) | 111.8 (13.3) | 115.1 (10.5) | ||
| Median (IQR) | 110.0 (10.0) | 110.0 (8.75) | 110.0 (10.0) | ||
Side effects were reported by 66 (33.2%) of the participants (Table 2). The
misoprostol group had a significantly higher rate of side effects (53.7%)
compared to the TNG group (14.4%; p
| Variable | Total | TNG Group | Misoprostol Group | p-value | OR (95% CI) |
| N = 199 | N = 104 | N = 95 | |||
| Drug side effect | 66 (33.2%) | 15 (14.4%) | 51 (53.7%) | 0.14 (0.07–0.28) | |
| Abdominal cramp | 46 (32.1%) | 4 (3.8%) | 42 (44.2%) | 0.05 (0.01–0.14) | |
| Nausea | 17 (8.5%) | 6 (5.8%) | 11 (11.6%) | 0.14 |
0.46 (0.16–1.31) |
| Vomiting | 4 (2.0%) | 1 (1.0%) | 3 (3.2%) | 0.35 |
0.29 (0.03–2.91) |
| Headache | 11 (5.5%) | 9 (8.7%) | 2 (2.1%) | 0.04 |
4.40 (0.92–20.9) |
| Palpitation | 1 (0.5%) | 0 (0%) | 1 (0.5%) | 0.47 |
— |
| Diarrhea | 2 (1.0%) | 0 (0%) | 2 (2.1%) | 0.22 |
— |
| Uterine bleeding before hysteroscopy | 25 (12.6%) | 2 (1.9%) | 23 (24.2%) | 0.06 (0.01–0.26) |
There was no statistically significant difference in the mean size of the
largest dilator inserted without resistance between the TNG and misoprostol
groups (6.26
Based on our findings, there was no statistically significant difference in the incidence of uterine bleeding as a complication of the intervention between women receiving TNG and misoprostol (3 cases, 2.7% vs. 1 case, 0.9%; p = 0.62). Additionally, there were no statistically significant differences in systolic blood pressure (p = 0.20), diastolic blood pressure (p = 0.46), and pulse rate (p = 0.62) after the intervention. In terms of pathological findings, the most common uterine pathology observed were polyps in both the TNG group (n = 40, 38.5%) and the misoprostol group (n = 47, 49.5%), with no statistical significance observed between the two groups (p = 0.11). No hysteroscopic complications, such as uterine perforation, cervical laceration, and false tract, were found in our study (Table 3).
| Variable | Total | TNG Group | Misoprostol Group | p-value | Effect size | |
| N = 199 | N = 104 | N = 95 | ||||
| Pulse rate after intervention | 0.03 | |||||
| Mean (SD) | 82.0 (7.4) | 81.92 (6.9) | 82.2 (7.9) | 0.620 |
||
| Median (IQR) | 82.0 (8.0) | 82.0 (8.0) | 83.0 (10.0) | |||
| Diastolic blood pressure after intervention | 0.05 | |||||
| Mean (SD) | 74.4 (7.8) | 74.8 (7.5) | 73.9 (8.1) | 0.460 |
||
| Median (IQR) | 75.0 (10.0) | 75.0 (10.0) | 75.0 (10.0) | |||
| Systolic blood pressure after intervention | 0.08 | |||||
| Mean (SD) | 119.4 (43.9) | 121.09 (60.0) | 117.6 (10.5) | 0.206 |
||
| Median (IQR) | 120.0 (10.0) | 116.0 (10.0) | 120.0 (10.0) | |||
| Dilator number | 0.09 | |||||
| Mean (SD) | 6.41 (2.0) | 6.26 (2.0) | 6.57 (2.1) | 0.200 |
||
| Median (IQR) | 6.0 (3.0) | 6.0 (3.0) | 6.0 (2.0) | |||
| Uterine bleeding after hysteroscopy, N (%) | 4 (1.8%) | 3 (2.7%) | 1 (0.9%) | 0.620 |
2.79 (0.28–27.30) | |
| Final pathology diagnosis, N (%) | ||||||
| Polyp | 87 (43.7%) | 40 (38.5%) | 47 (49.5%) | 0.110 |
0.63 (0.36–1.12) | |
| Myoma | 9 (4.5%) | 5 (4.8%) | 4 (4.2%) | 1.000 |
1.14 (0.29–4.41) | |
| Proliferative | 42 (21.1%) | 27 (26.0%) | 15 (15.8%) | 0.070 |
1.87 (0.92–3.78) | |
| Secretory | 32 (16.1%) | 21 (20.2%) | 11 (11.6%) | 0.090 |
1.93 (0.87–4.25) | |
| Hysteroscopic complication | 0 | 0 | 0 | — | — | |
Cervical stenosis was observed in 2 cases (33.3%) in TNG group and 4 cases (66.7%) in the misoprostol group. Chi-square test between the groups showed that there was no statistically significant difference (p = 0.37).
Hysteroscopy plays a crucial role in diagnosing uterine diseases such as endometrial polyps and intrauterine fibroids, which may require myomectomy [12]. Therefore, understanding strategies to minimize complications is crucial. This research aims to compare the effectiveness of sublingual TNG and sublingual misoprostol in cervical preparation. According to the findings of the present study, side effects were reported by 33.2% of the participants. The misoprostol group experienced a significantly higher rate of side effects (53.7%) compared to the TNG group (14.4%). In comparison to sublingual misoprostol, sublingual TNG was significantly associated with fewer side effects. Abdominal cramps were the most common side effect observed in this study. Previous reviews have consistently reported a higher occurrence of side effects with misoprostol.
In a 2010 study by El-Khayat et al. [13], the effectiveness of misoprostol and isosorbide mononitrate for cervical ripening in candidates undergoing hysteroscopy was investigated. The study concluded that isosorbide mononitrite was more effective than misoprostol in cervical ripening and presented fewer side effects [13]. Shahraki et al. [14] examined the effects of vaginal isosorbide mononitrite and vaginal misoprostol prior to hysteroscopy. They found that the misoprostol group experienced a shorter duration of dilation, achieved a better degree of dilation, and reported greater abdominal pain [14]. Li et al. [15] compared the effects of misoprostol and isosorbide mononitrate in pregnancy termination, with a misoprostol group. They reported that the misoprostol group achieved greater cervical dilation and experienced less bleeding. Singh et al. [16] administered 400 µg of vaginal misoprostol 3–4 hours before hysteroscopy, achieving maximum cervical dilation prior to the procedure.
A similar study was conducted to assess cervical preparation in full-term pregnancies. Post drug administration, the group receiving vaginal misoprostol exhibited significantly higher levels of cervical readiness and higher Bishop score compared to the TNG group. The incidence of pre-delivery side effects was 14.9% in the misoprostol group and 39.2% in the TNG group, demonstrating statistical significance in both cohorts. In this study, misoprostol exhibited a lower incidence of side effects compared to TNG. The study focused on examining the impact of sublingual TNG and misoprostol following hysteroscopy, with our methodology differing from in that of a prior study [17] in this aspect.
According to a systematic review, misoprostol is deemed suitable for cervical preparation. However, all studies (100%) reported the occurrence of few side effects [18]. Chung et al. [19], in their review, similarly concluded that misoprostol is effective for cervical preparation. They also emphasized the significance of exploring alternative drugs with potentially higher efficacy [20]. Another study highlighted the significance of determining the optimal dosage of misoprostol for improved cervical preparation [21]. In the current study, headache emerged has the most commonly reported side effect in the TNG group, with a significantly higher incidence (8.7%) compared to the misoprostol group (2.1%). Several studies have associated the administration of TNG with headaches in women, indicating a higher risk of headaches in those receiving TNG [22, 23]. Amorim et al. study [24], which focused on examining preterm labor, reported a higher incidence of headache complications in pregnant women who were administered TNG compared to those receiving nifedipine.
These findings underscore the concern regarding headaches in women receiving TNG, a phenomenon also observed in the present study. The occurrence of headaches is associated with changes in women’s blood pressure. Research indicates that TNG is known to lower blood pressure, and fluctuations in blood pressure can lead to headaches and dizziness [25]. Monitoring blood pressure before administering TNG may potentially be effective in managing women’s conditions.
Furthermore, the current study revealed a significantly higher incidence of muscle cramps in the misoprostol group (44.2%) compared to the TNG group (3.8%). There was also a statistically significant difference in uterine bleeding before hysteroscopy as a side effect of misoprostol between the two intervention groups. Study has indicated that vasodilators can increase blood flow to the endometrium. TNG acts on the smoth muscles of blood vessels by interacting with niacinic acid, which possesses the ability to relax blood vessel walls and induce vessel dilation. Consequently, nitric oxide promotes increased blood flow and reduces uterine blood pressure. Additionally, aspirin can have positive effects on the uterus [26, 27].
Numeous studies have reported the relative side effects associated with misoprostol. A survey conducted on patients undergoing hysterectomy revealed that the predominant complication was bleeding, with an incidence of 93.23% in the misoprostol group and 69.7% in the non-misoprostol group. Only 1.5% of patients in the misoprostol group reported side effects. The total incidence of complications was higher in the misoprostol group compared to the non-misoprostol group [28]. Inácio et al. [28] examined the effects of oral or vaginal misoprostol and observed that both administration routes resulted in higher levels of cervical dilation compared to the misoprostol group. While the degree of cervical dilation and dilation time were comparable between both misoprostol administration groups, the incidence of nausea and vomiting was higher in the oral misoprostol group [28]. A study by Mulayim et al. [29] showed that sublingual administration of misoprostol before hysteroscopy resulted in a shorter duration of cervical dilation compared to the group receiving misoprostol [30]. In a study by Hameed and Farhan [31], it was observed that the time required to achieve the cervical dilatation was significantly shorter, and complications were fewer in the normal saline infiltration group compared to the misoprostol group.
In the current study, the frequency of cervical stenosis was 33.3% in TNG group and 66.7% in misoprostol group. Vitale et al. [32] showed that, despite the availability of miniaturized instruments that have made the management of cervical stenosis more feasible, it remains a complex task, even for experienced hysteroscopists.
According to the findings of the present study, there were no significant differences in age, BMI, and other characteristics among the groups. Additionally, the impact of sublingual TNG on bleeding and pain after hysteroscopy was found to be comparable to that of misoprostol, with no significant differences observed. These findings suggest that TNG can be serve as an alternative to misoprostol in hysteroscopy. One limitation of the current study was the non-cooperation of some women, despite thorough explanations regarding the safety of the tests provided at the beginning of the study. Women were requested to participate in the study voluntarily and willingly. One strength of our research was the adequate sample size in both investigated groups.
When comparing the two investigated groups, it was observed that sublingual TNG resulted in significantly fewer side effects compared to sublingual misoprostol. However, headaches were more common in the group receiving TNG than in the misoprostol group. Considering the impact and efficacy of sublingual TNG in preparing the cervix before hysteroscopy, which is comparable to that of sublingual misoprostol, TNG can be utilized to facilitate the procedure. This approach can also help reduce the costs and complications associated with cervical dilation prior to hysteroscopy.
The underlying data supporting the results of our study can be found in the manuscript.
SM contributed in writing of the original draft and in conceptualization of the work. MM and KT performed the conceptualization. RD and SS contributed in analysis data. SR was involved in conception and design, acquisition of data and writing the review and editing the paper. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study protocol received approval from the Ethics Committee of Iran University of Medical Sciences (code: IR.IUMS.REC.1402.180), and it was registered on the IRCT website (code: IRCT20191123045476N4). Prior to enrollment, written informed consent was obtained from all participants.
The authors thank Rasoul Akram Hospital Clinical Research Development Center (RCRDC), Iran University of Medical Sciences, for its editorial assistance.
The authors gratefully acknowledge the financial support by the Iran University of Medical Sciences (1401-4-65-24853).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

