1 Department of Obstetrics and Gynecology, The Third Clinical Institute Affiliated to Wenzhou Medical University/Wenzhou People's Hospital/Wenzhou Maternal and Child Health Care Hospital/The Third Affiliated Hospital of Shanghai University, 325000 Wenzhou, Zhejiang, China
Abstract
Background: This study aimed to investigate the effects of
low-frequency electrical stimulation combined with abdominal acupoint massage on
the recovery of gastrointestinal function following cesarean section.
Methods: A total of 60 postoperative patients were randomly assigned to
either the control group (group A, n = 30) or the observation group (group B, n =
30) between January 2021 to December 2021. The control group received
conventional interventions, while the observation group received a nursing
intervention consisting of low-frequency electrical stimulation combined with
abdominal acupoint massage starting at 10–12 hours after the operation. The
primary outcomes included the time to first bowel sound, time to flatus, time to
defecation, and time to lactation. The secondary outcomes included postoperative
visual analogue scale (VAS) pain scores, the rate and severity of abdominal
distension, and serum levels of prolactin (PRL) and vasoactive intestinal peptide
(VIP). Results: The observation group had significantly earlier
restoration of bowel sounds, passage of first flatus, and first defecation than
the control group (p
Keywords
- low-frequency electrical stimulation
- acupoint massage
- gastrointestinal function
Cesarean section is one of the most common abdominal surgeries. According to a
2008 report by the World Health Organization (WHO), the global rate of cesarean
sections is approximately 20%, thus indicating that means that nearly 13 million
women undergo cesarean section every year. The reported incidence of intestinal
obstruction after cesarean section is 5%; therefore, approximately 650,000 women
suffer from intestinal obstruction annually [1]. Postoperative intestinal
obstruction not only increases discomfort after surgery but also hinders
breastfeeding [2, 3]. Because it would lead to insufficient nutrient absorption by
the mothers, which would affect lactation and lead to breastfeeding failure.
Additionally, it can lead to additional medical expenses. In the United States
alone, postoperative intestinal obstruction is estimated to increase medical
expenditures by approximately
Currently, the treatment of gastrointestinal reactions mostly relies on medication [5]. However, during cesarean section, the use of drugs is often limited due to their potential impact on the fetus through breast milk. Low-frequency electrical stimulation is a safe, effective, and well-accepted clinical treatment method [6]. It can protect and regulate the gastrointestinal tract by activating the endogenous antioxidant stress system and promoting the secretion of endogenous opioid peptides [7]. Acupoint massage therapy, as part of traditional Chinese medicine treatment, is widely used in China to alleviate and improve symptoms of gastrointestinal disorders [8]. However, the application of low-frequency electrical stimulation combined with abdominal acupoint massage in cesarean section surgery is relatively limited. This study aims to incorporate low-frequency electrical stimulation combined with abdominal acupoint massage after cesarean section to observe whether this approach can prevent and treat gastrointestinal reactions that occur during the perioperative period.
Ethical approval for this study was obtained from the Research Ethics Committee of Wenzhou People’s Hospital (Zhejiang, China; reference number 2020-260) and this study was registered with the ISRCTN registry (https://www.isrctn.com/), registration number: ISRCTN16533743. Informed consent was obtained from all patients scheduled to undergo elective cesarean section under spinal anesthesia. A total of 60 women were included in the study. The inclusion criteria were American Society of Anesthesiologists physical status I or II and a normal singleton pregnancy with at least 37 weeks of gestation. The exclusion criteria included emergency surgery, previous bowel surgery, chronic digestive disease, diabetes, hypertension, and contraindications to low-frequency electrical stimulation, such as skin damage at relevant acupoints, local tumors, and pacemaker installation.
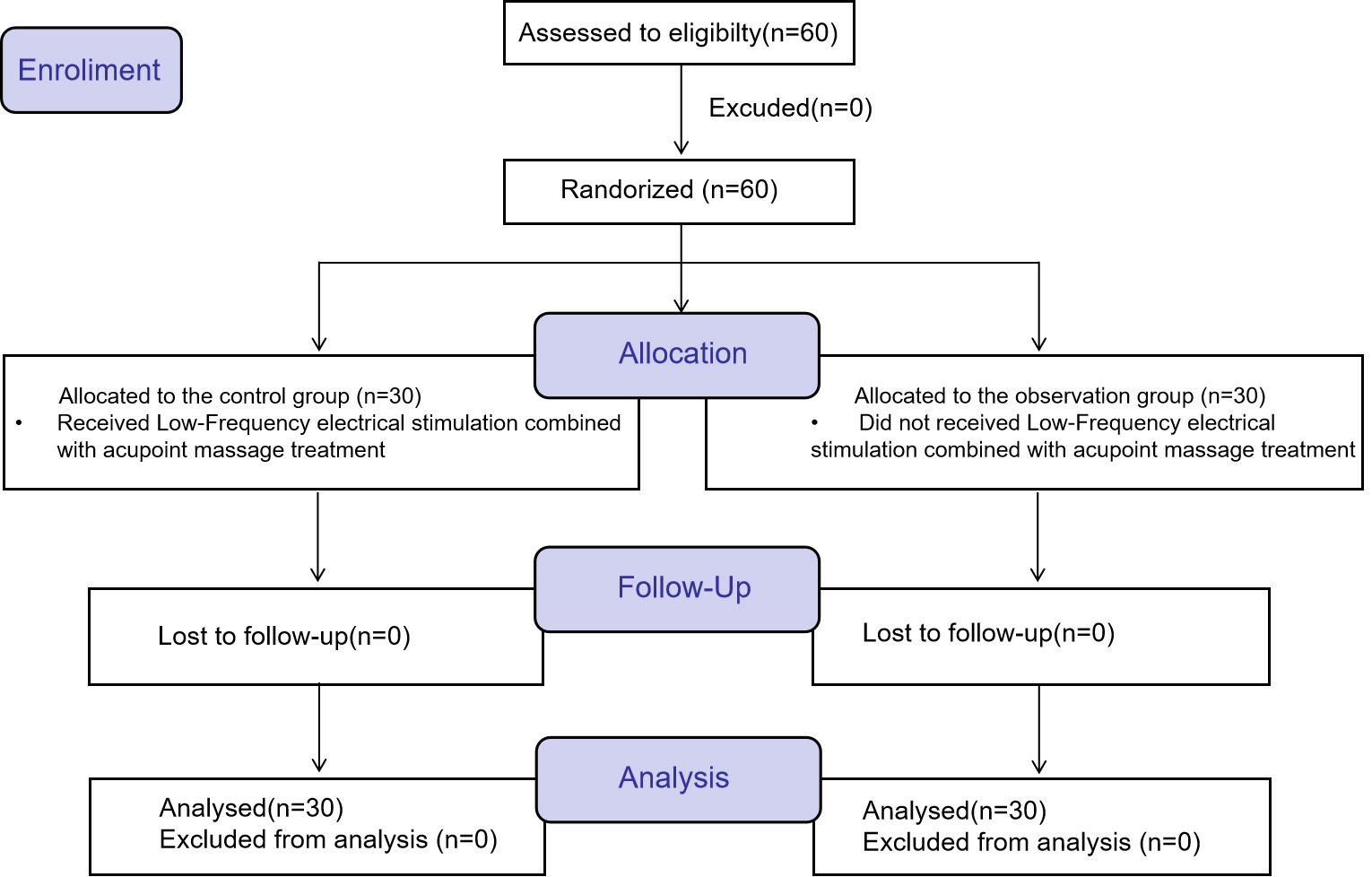
The study population consisted of 60 patients admitted to the obstetrics department of our hospital from January 2021 to December 2021. An administrative staff member handled patient enrollment, and patients randomly draw a number card from an opaque envelope prepared in advance, ranging from 1 to 60. Then, based on the random numbers generated by Excel, the patients were automatically assigned patients into 1 of the 2 groups. Patients were allocated into the control group (group A, n = 30) or the observation group (group B, n = 30) using a 1:1 ratio. All data were collected post-intervention. All subjects and investigators involved in recruitment, data collection, and statistical analysis were blinded to randomization status throughout the study. Only the operator knew about the interventions the subjects received, but she had no involvement in the study process. Patients flow diagram is shown in Fig. 1.
 Fig. 1.
Fig. 1.Patients flow diagram.
The control group received routine postoperative care after cesarean section without any specific interventions. The patient’s mouth was scrubbed with a cotton swab dipped in normal saline, and the dressing on the abdominal wound was changed daily. Local pressure was applied 6 hours after the operation to reduce bleeding or oozing. The vulva was scrubbed with iodophor twice a day. The indwelling urinary catheter was cleaned to prevent urinary tract infection and removed 48 hours after the operation. No food was allowed until bowel function resumed.
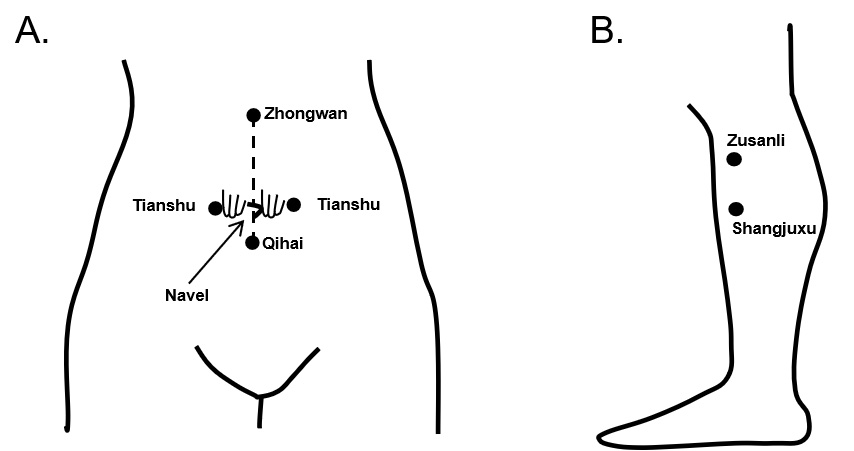
For the observation group, in addition to general postoperative care, low-frequency electrical stimulation treatment using the Myotrac Infiniti System (S4, Nanjing Weisi Medical Technology Co., Ltd., Nanjing, Jiangsu, China) was initiated 8–12 hours after surgery. Circular electrode patches were attached to both sides of the sacrococcygeal for low-frequency pulse and electrical stimulation treatment. The parameters were set as follows: frequency of 60 Hz, waveform width of 300 s, working for 6 s, resting for 3 s, waveform rising for 2 s, waveform falling for 0 s, and the current intensity was adjusted based on the maximum intensity that could be tolerated by the patient. The treatment was administered twice a day for 30 minutes per session until bowel function returned to normal. Abdominal acupoint massage was performed after low-frequency electrical stimulation. Prior to the massage, the patient was instructed to empty their bladder, assume a supine position, relax the abdomen, loosen clothing, and maintain warmth. The operator used rubbing and pushing techniques to massage in a clockwise direction from the Zhongwan (CV12) acupoint to the Tianshu (ST25) acupoint on the left, then to the Qihai (CV6) acupoint, the Tianshu (ST25) acupoint on the right, and back to the Zhongwan (CV12) acupoint. This circular massage was performed for approximately 5 minutes. Care was taken to avoid massaging the area 5 cm above and below the abdominal cesarean section wound to prevent subcutaneous hematoma caused by muscle fiber traction. Then, the kneading method was used to massage the Zhongwan (CV12) acupoint, the Tianshu (ST25) acupoint on both sides, and the Qihai (CV6) acupoint 30 times each. Finally, the pressing method was used to press the Juxu acupoint on both sides for approximately 3 seconds. Then, the kneading method was used to massage clockwise 30 times. This massage should be performed once daily, using even force and gentle movements, as long as the patient does not feel pain. During the massage, the patient should be instructed to cooperate with inhalation and exhalation.
The Zhongwan (CV12) acupoint is located in the upper abdomen at the midpoint between the lower sternum and the navel, approximately 4 inches above the navel. The Tianshu (ST25) acupoint is located in the middle abdomen, with three finger widths to the left and right of the navel. The Qihai (CV6) acupoint is located 1.5 inches below the umbilicus on the midline of the abdomen. The Shangjuxu (ST37) acupoint is located on the front and outer side of the calf, approximately 3 inches below the Zusanli (ST36) acupoint (Fig. 2).
 Fig. 2.
Fig. 2.Locations of acupoints. (A) Zhongwan (CV12) acupoint, Tianshu (ST25) and Qinhai. (B) Shangjuxu (ST37) acupoint.
The primary outcomes were the time to first bowel sound, time to first flatus, time to first defecation, and time to lactation, calculated from the end of surgery. Secondary outcomes included the postoperative visual analogue scale (VAS) pain score, the rate and severity of abdominal distension, and the serum levels of prolactin (PRL) and vasoactive intestinal peptide (VIP). The blood samples used were fasting peripheral venous blood, with PRL detected by radioimmunoassay using PRL antibody (AS1003.1, Immundiagnostik AG, Bernsheim, Germany) and VIP detected using enzyme linked immunosorbent assay (CSB-E08354h, Cusabio Biotech Co., Ltd., Wuhan, Hubei, China).
The sample size was calculated based on the recovery time of initial sounds of
12 subjects (6 in each group) from the pilot study before conducting this study.
The time to recovery time of intestinal sounds was 22.7
The general characteristics of the two groups were compared in Table 1. There
were no statistically significant differences in the baseline characteristics
between the two groups (p
| Group | n | Age (years) | Gestation age (weeks) | Total number of pregnancies | Total number of deliveries |
| Group A | 30 | 29.5 |
39.0 |
1.67 |
1.43 |
| Group B | 30 | 30.6 |
39.2 |
1.83 |
1.60 |
| p | 0.441 | 0.429 | 0.308 | 0.283 |
Data regarding the primary outcomes are shown in Table 2. The time to recovery
time of intestinal sounds, first flatus, first defecation, and first lactation
were significantly earlier in the observation group than in the control group
(p
| Group | n | Recovery time of intestinal sounds (h) | First flatus (h) | First defecation (h) | First lactation (h) |
| Group A | 30 | 23.6 |
38.5 |
50.2 |
38.7 |
| Group B | 30 | 19.2 |
25.3 |
39.5 |
31.2 |
| p |
Data regarding the secondary outcomes are shown in Table 3. The VAS scores in
the observation group were significantly lower than those in the control group
(p
| Group | n | 24 h | 48 h | 72 h |
| Group A | 30 | 6.86 |
4.63 |
3.73 |
| Group B | 30 | 4.33 |
2.80 |
1.73 |
| p |
| Group | n | The proportion of abdominal distension (%) | Levels | ||
| Light | Medium | Heavy | |||
| Group A | 11 | 36.7 | 6 | 4 | 1 |
| Group B | 4 | 13.3 |
3 | 1 | 0 |
| Group | n | PRL (ng/mL) | VIP (pg/mL) | ||
| Before treatment | After treatment | Before treatment | After treatment | ||
| Group A | 30 | 233.45 |
274.25 |
305.34 |
253.48 |
| Group B | 30 | 230.67 |
320.98 |
310.93 |
220.88 |
| p | 0.808 | 0.471 | |||
PRL, prolactin; VIP, vasoactive intestinal peptide.
Cesarean section is one of the most common surgical procedures in obstetrics and gynecology, and its prevalence is increasing worldwide year by year [9]. Early postoperative rehabilitation measures for such a large patient group should be widely considered. The recovery of postoperative gastrointestinal function is an important indicator of postoperative rehabilitation. After abdominal surgery, gastrointestinal motility is weakened, and delayed recovery of gastrointestinal function not only increases the patient’s discomfort but also prolongs hospitalization and increases costs. For patients undergoing cesarean section, gastrointestinal dysfunction is not conducive to breastfeeding or the establishment of a good parent‒child relationship [10].
Gastrointestinal dysfunction is a common postoperative complication after
various abdominal surgeries, including cesarean section. The main symptoms
include difficulty passing gas and defecation, abdominal pain, and distension
[11]. According to Traditional Chinese Medicine (TCM), it is believed that the
proper function of the stomach and intestines relies on the unobstructed descent
of Qi. If there is a blockage in the communication between the upper and lower
Qi, it can lead to the stagnation of Qi in hollow organs (Fu), resulting in
gastrointestinal dysfunction, including symptoms such as abdominal distension,
constipation, and other manifestations [12]. The acupuncture treatment method
used by the observation group in the study is to intervene by using the
traditional Chinese medicine theory of acupoint massage to regulate the human
meridians. Its main function is to stimulate acupoints, achieving the balance of
qi and blood, and yin and yang. Among them, the Tianshu (ST25) acupoint belongs
to the Mu point of the Large Intestine Meridian and has the effects of
strengthening the spleen, stomach, and regulating qi; the Shangjuxu (ST37)
acupoint belongs to the combination point of the lower large intestine, which has
the function of regulating the intestines and stomach, promoting the circulation
of the internal organs and resolving stagnation; the Zhongwan (CV12) acupoint is
a acupoint for the stomach, which can be used to treat all visceral diseases; the
Qihai (CV6) acupoint can regulate the Qi of the lower burner and replenish it
[13, 14, 15, 16]. According to traditional Chinese medicine theory, the combination of the
Tianshu (ST25) Qihai (CV6), Tianshu (ST25), Shangjuxu (ST37) and Zhongwan (CV12)
acupoints have a good effect on gastrointestinal disease [17, 18]. This study
shows that the time for the passage of first flatus, the first defecation, and
the time for bowel sounds to return to normal in the observation group were
significantly shorter than those in the control group (p
Gastrointestinal function relies on the coordinated regulation of
gastrointestinal hormones and the nervous system. VIP is an inhibitory
gastrointestinal hormone. Previous studies have shown that massage the Zhongwan
(CV12) acupoint can increase the release of peptidergic neurotransmitters such as
motilin and gastrin, thereby partially restoring suppressed gastric electrical
activity, relieving gastrointestinal dysfunction, and promoting the recovery of
gastrointestinal motility [19]. This study found that the serum VIP level in the
observation group after treatment was significantly lower than that in the
control group (p
In summary, the utilization of low-frequency electrical stimulation combined with abdominal acupoint massage can effectively enhance early lactation in mothers, expedite the restoration of gastrointestinal function, decrease the occurrence of postoperative adverse reactions such as abdominal distension, increase PRL levels, and inhibit VIP levels. These mechanisms contribute to its therapeutic effects. Limitations of our study include the relatively small sample size (although this was a pilot study), which does suggest the need for a larger prospective multicenter study involving more patients with follow-up, and the subjective nature of the questionnaire.
The data that support the findings of this study are available from the Wenzhou People’s Hospital but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Wenzhou People’s Hospital.
XZ conceived the study. XZ and MC searched the literature and collected the data. XZ and MC performed the statistical analysis. XZ drafted the manuscript. MC reviewed the manuscript. Both authors contributed to editorial changes in the manuscript. Both authors have read and approved the final paper. Both authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This study was approved by the Research Ethics Committee of Wenzhou People’s Hospital (Zhejiang, China; reference number 2020-260). Informed consent was obtained from all patients.
Not applicable.
This work was supported by funds from the basic scientific research projects of Wenzhou City (No. Y20201005).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.