1 Department of Medical Genetics, West China Second University Hospital, Sichuan University, 610041 Chengdu, Sichuan, China
2 Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), Ministry of Education, 610041 Chengdu, Sichuan, China
†These authors contributed equally.
Abstract
Background: There is currently no specific requirement for operator’s attires performing amniocentesis, especially for repetitive amniocenteses. We investigated the contamination status on the surface of operators with or without long-sleeved surgical gowns during repetitive amniocenteses to examine whether they are different. Methods: In a prospective cohort study, consecutive samples were collected from the surface of amniocentesis operators with short-sleeved scrubs (bare arms) or with long-sleeved surgical gowns on 4 sites (including the left and right proximal medial forearm, and the left and right ventral wrist). There were 7 time spots during each sampling period. Results: The highest colony count among all plates was 65 colony forming units (cfu)/plate. We observed 85.3% (382/448) and 65.1% (255/392) plates with 0 colony count from operators with bare arms and in surgical gowns, respectively. Moreover, the bacterial load of the group with surgical gowns had an increasing trend with time while the other group showed a contrary trend. Conclusions: All colony counts observed were within the hygiene specification of the National Health Commission of China. Instead of attires, other measures with high-quality evidence including surveillance of hand hygiene and control of indoor air bacterial load should be given more attention.
Keywords
- amniocentesis
- surgical gown
- surgical scrub
- surgical site infection
- colony count
- operating room
Amniocentesis is one of the most common invasive procedures in prenatal diagnosis and is typically performed between 17 and 23 weeks of gestation, aiming to obtain fetal cells from amniotic fluid for fetus’ genetic tests [1]. In countries with large population such as China, the birth rate remains high, which leads to the fact that obstetrics and gynecology institutions handle a large load of prenatal diagnostic procedures, including amniocentesis. Thus, in large prenatal diagnostic centers in China, facing the need for efficiency, amniocenteses are usually performed repetitively in a specific operating room during the same time period rather than performed as a bedside or outpatient procedure. Although amniocentesis is regarded as a relatively safe operation with a risk of pregnancy loss of less than 1% [2], other complications such as preterm labor, spontaneous abortion, missed abortion, premature rupture of membranes, amniotic leakage, vaginal bleeding, and antenatal hospital admission also potentially exist [3, 4]. There is no strong evidence exploring the relationship between operator surface contamination and puncture site infection risk or complications of amniocentesis. In addition, specific requirements for operator’s attires performing amniocentesis are absent in China’s relevant specifications.
In our pre-surveys of different institutions, we found that there were differences in operator’s attires and the differences were mainly in wearing long-sleeved surgical gowns. We believed that what to wear when performing amniocentesis in considering the comfort of repetitive procedures in the operating room with the avoidance of potential consequences of operator’s surface contamination was worth investigating.
In this study, two types of attires currently used in operating rooms during repetitive amniocenteses were selected and researched. The first type is to wear only a short-sleeved scrub which was bare below the elbow while the other is to put a sterile long-sleeved surgical gown on the top of the short-sleeved scrub. Both scrubs and gowns are worn throughout the operating time period rather than replaced after each amniocentesis. Standard surgical hand antisepsis was performed after garbing the short-sleeved scrub regardless of the attire type. Operators repeatedly performed five steps of putting on sterile gloves, detecting and positioning by ultrasound, puncturing, taking off gloves, and using alcoholic hand-rub for hand disinfection. Pregnant patients entered the operating room in sequence, and amniocenteses were repetitively performed. The only difference in routine between these two groups existed at the last step: the operators of the bare arms group rubbed the entire forearms, wrists, and hands while the disinfection area of the operators in surgical gowns was limited to their hands due to the coverage on forearms and wrists.
Thus, we aimed to investigate the surface contamination of amniocentesis operators during repetitive amniocenteses in these two kinds of attires at a tertiary level referral prenatal diagnostic center in China and in order to determine whether they are different from the perspective of surface bacterial loads.
The prospective cohort study was performed at a tertiary level referral prenatal diagnostic center in Western China. This center provides more than 10,000 amniocenteses annually, which is among the highest in China. Over 60 cases of amniocenteses are performed daily in this center during two periods. In March 2022, bacterial loads were obtained from obstetricians performing amniocenteses at this center.
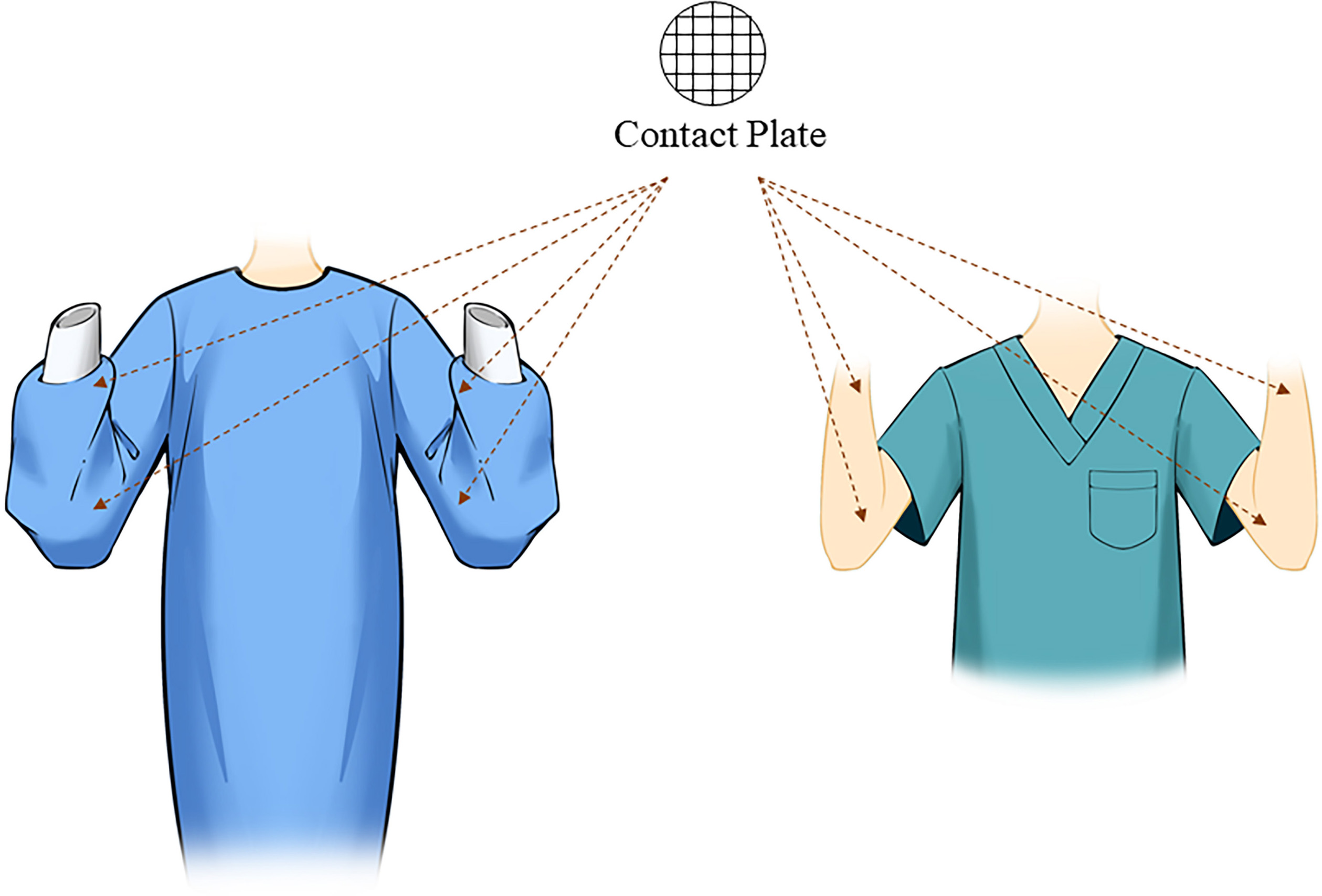
In a whole sampling procedure, bacterial loads at time spot 0 (T0) were sampled before the first amniocentesis, right after the operator had performed hand antisepsis and put on the surgical gown (surgical gowns group only). Then, samplings were repeated after every 5 cases of amniocenteses (about constant 20 minutes for operating 5 cases) until the last samplings were performed after the 30th case of amniocentesis, separately naming these time spots of sampling as T1–T6. There were four sampling sites for each operator, including the left proximal medial forearm, the right proximal medial forearm, the left ventral wrist, and the right ventral wrist (Fig. 1). At each time spot from T0–T6, samples were obtained from each location. Accordingly, 28 samplings in total were conducted in each sampling period. RODAC contact plates (diameter of 5.5 cm; #722011, BKMAMLAB, Changde, Hunan, China) were used for sampling by directly contacting the operators’ surface (skin for those with bare arms and fabric for those in surgical gowns) for 10 seconds. Incubating at 37 °C for 48 hours, the plates were observed at the microbiology laboratory for bacterial loads (recording as colony forming units (cfu)/plate).
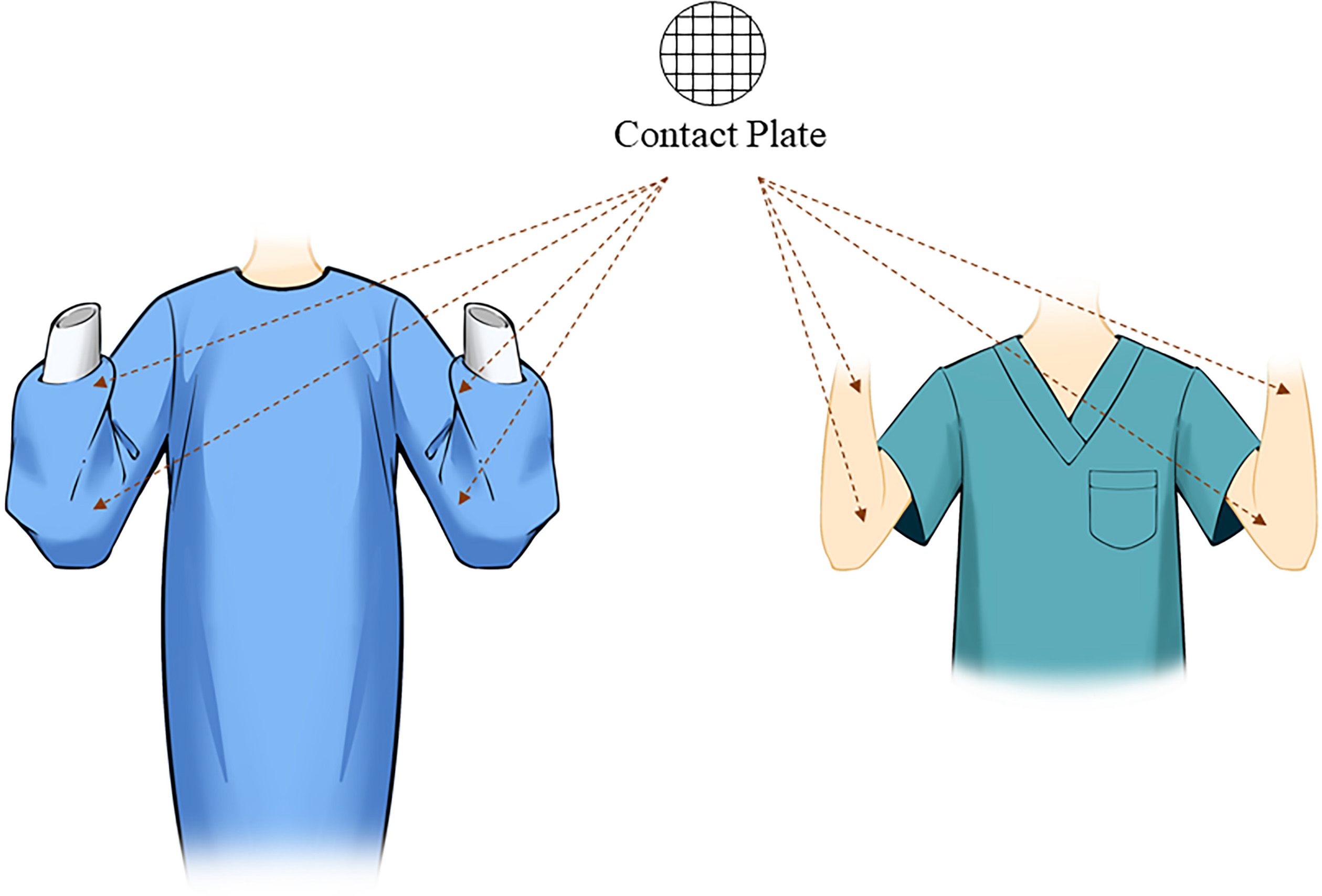 Fig. 1.
Fig. 1.The schema of sampling sites on the surface of operators with two kinds of attires. Four same sites on wrists and forearms were sampled from amniocentesis operators in both groups.
After collecting all data in Microsoft Excel sheets, statistical analyses were
performed with IBM SPSS Statistics 23 (IBM SPSS statistics, Chicago, IL, USA).
For the descriptive analysis of all variables, surface colony counts of different
attires, time spots, and sampling sites were performed as median and
interquartile range. The comparisons of basal bacterial loads between different
attires and sampling sites were measured by Mann-Whitney U-test. Within each
group of attire, comparisons at various time spots were carried out using
Friedman test, and post-hoc tests were analyzed by Nemenyi test if statistical
significance existed. All statistical tests were bidirectional, and
In our study, there were 7 time spots, 4 sampling sets, and separately 14 sampling periods for operators in surgical gowns and 16 sampling periods for operators with bare arms, which means k equals to 7 and N equals respectively to 56 and 64. According to Demšar, q0.05 here equals to 2.949, which means CD equals to 1.20 for the surgical gowns group and 1.13 for the bare arms group.
Data were obtained for statistical calculation from 840 contact plates during 30 sequential operating periods for amniocentesis (16 from operators with bare arms and 14 from operators in surgical gowns). Bacterial loads according to attires, sampling sites, and time spots are shown in Table 1. The bacterial loads were generally at a low level for both attires; 85.3% (382/448) and 65.1% (255/392) plates were respectively observed with 0 colony count from operators with bare arms and in surgical gowns. The highest colony count was 65 cfu/plate, observed from a plate of operators with bare arms, which was sampled on the forearm at T0. Meanwhile, the maximum for operators in surgical gowns was 43 cfu/plate which was sampled on the forearm at T6.
| Time spots | Median colony count (IQR) (cfu/plate) | |||
| Operators with bare arms | Operators in surgical gowns | |||
| Forearms | Wrists | Forearms | Wrists | |
| T0 | 1 (2) | 0 (4.25) | 0 (0) | 0 (0) |
| T1 | 0 (1.75) | 0 (1) | 0 (0) | 0 (0) |
| T2 | 1 (3) | 0 (1) | 0 (0) | 0 (0) |
| T3 | 0 (1.75) | 0 (1) | 0 (0) | 0 (0) |
| T4 | 0 (1.75) | 0 (0) | 0 (1) | 0 (0) |
| T5 | 0 (1) | 0 (0) | 0 (1) | 0 (0) |
| T6 | 0 (1) | 0 (0) | 0 (1) | 0 (0) |
IQR, interquartile range; cfu, colony forming units.
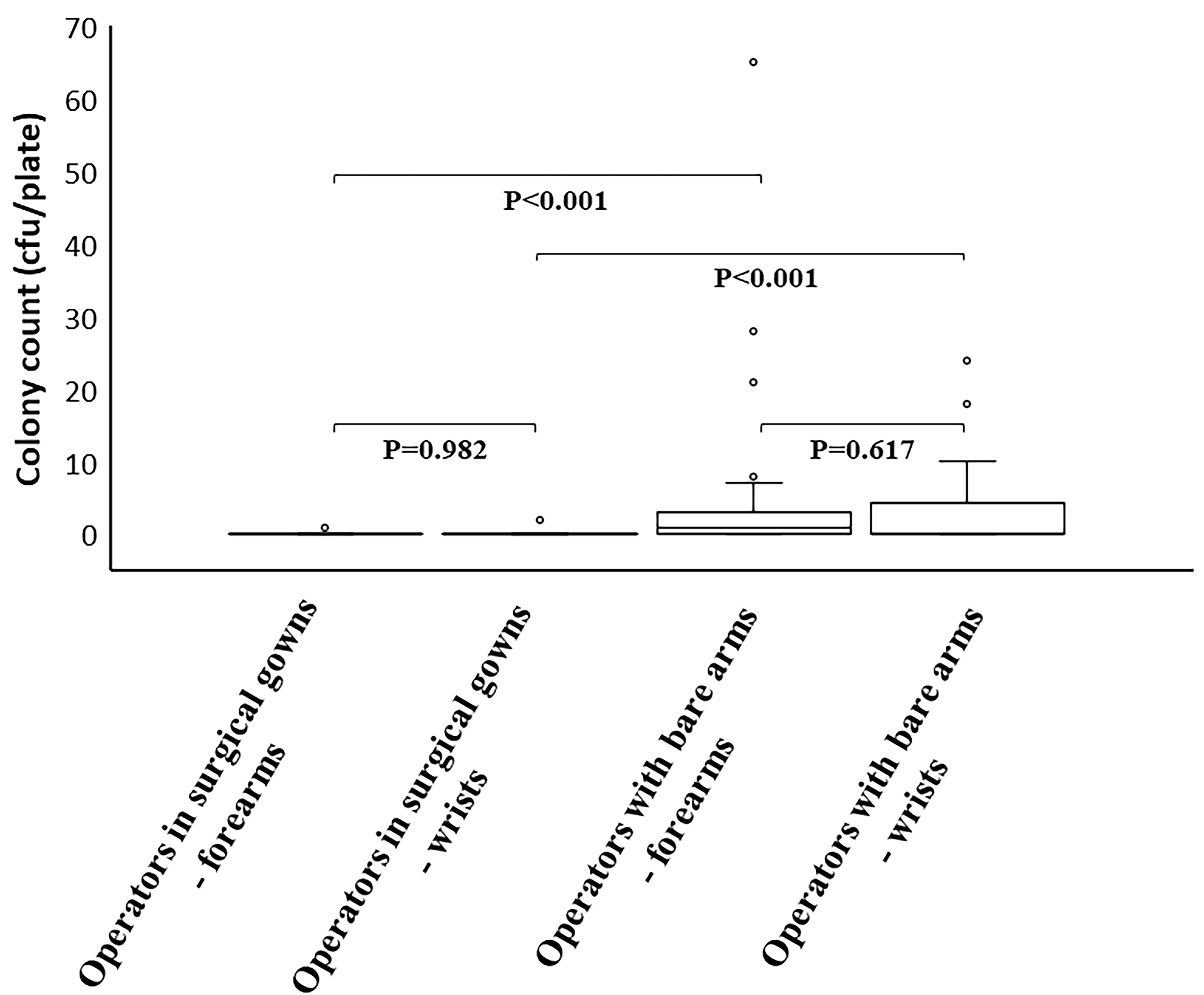
Regarding the basal sterile status of different attires, focusing on the surface
of proximal medial forearms, a lower bacterial load was obtained from the
operators in surgical gowns than from operators with bare arms (p
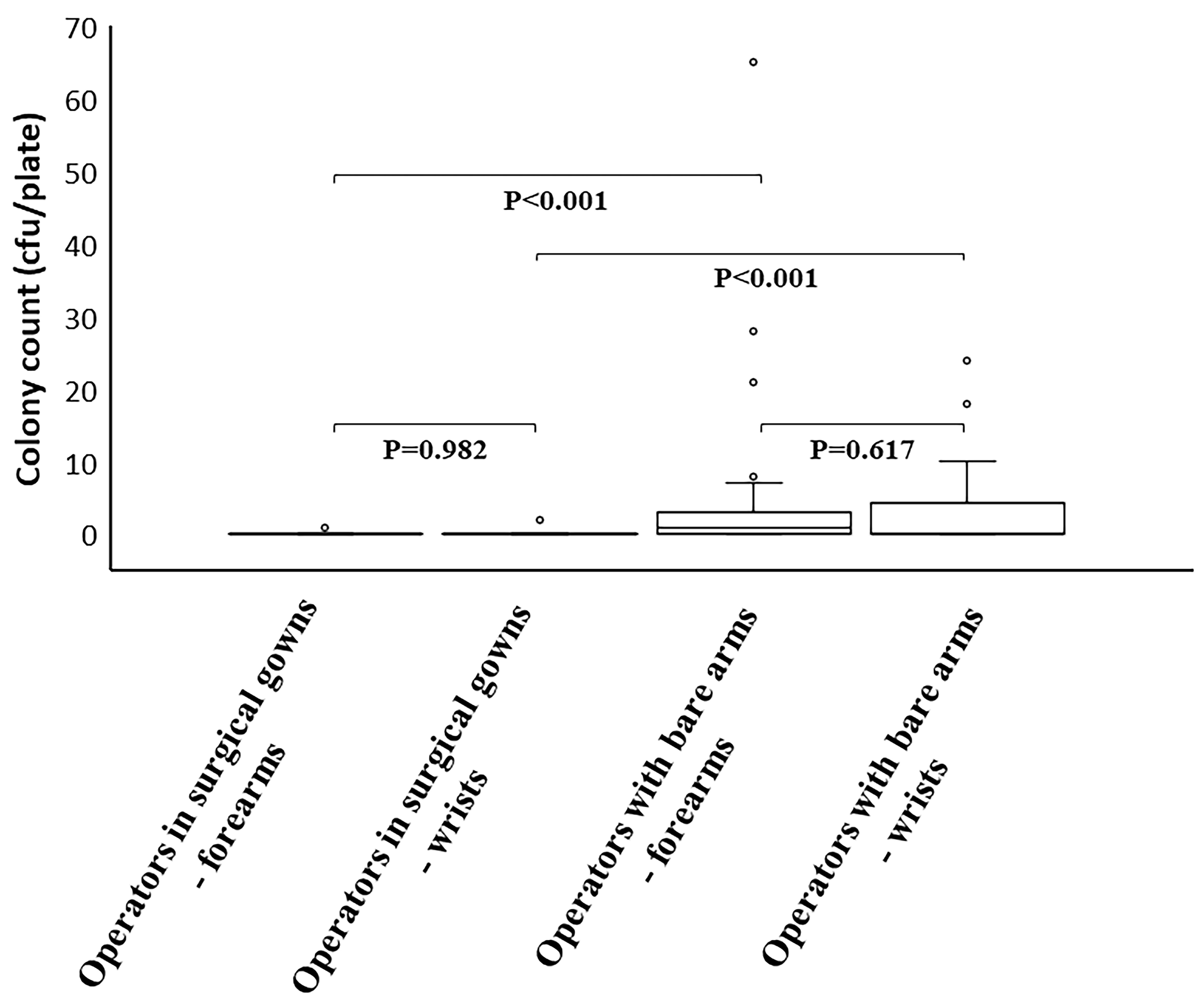 Fig. 2.
Fig. 2.Comparisons of surface bacterial loads before the first operation. At time spot 0 (T0), surface bacterial loads of the same sites on different attires and different sites on the same attires were compared.
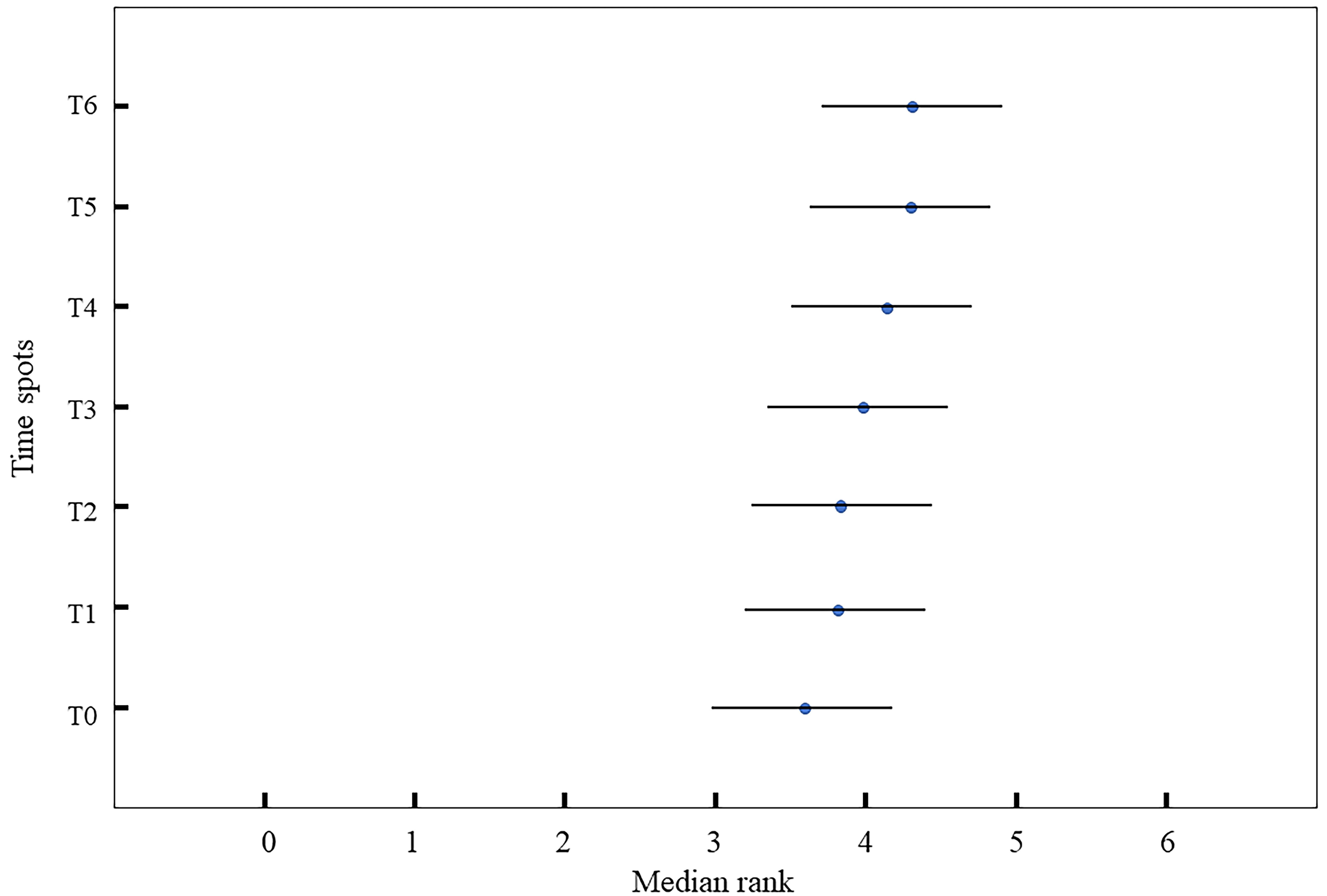
In the group of operators wearing surgical gowns, statistically significant differences were found in bacterial loads at different time spots (Friedman test, p = 0.004). Overall, the surface colony counts increased gradually with the increase in operation duration. However, according to the later post-hoc test, there was no significant difference in bacterial load between any two time spots (Fig. 3).
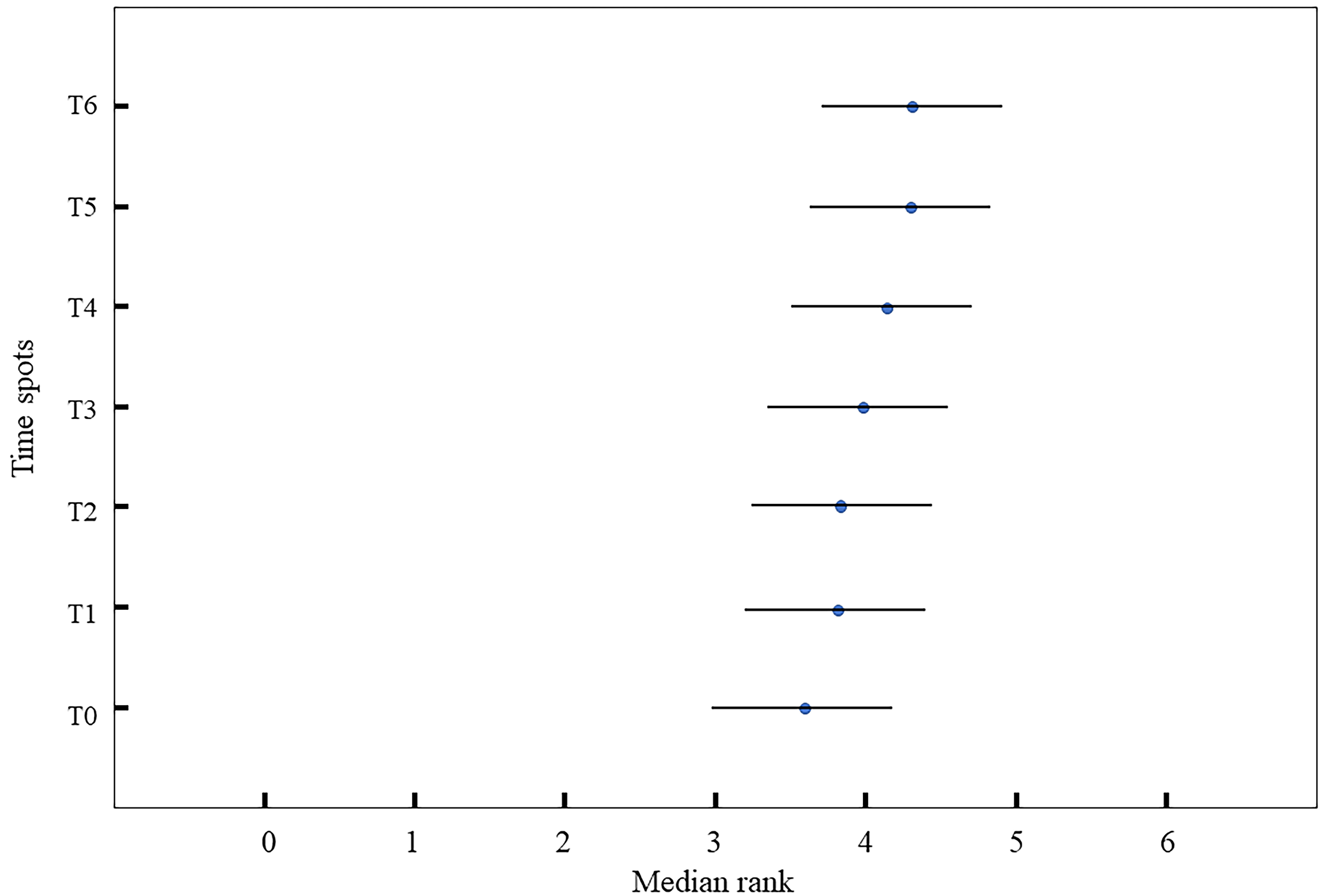 Fig. 3.
Fig. 3.Comparison of surface bacterial loads at different time spots in the surgical gowns group. The results of Nemenyi test of the surgical gowns group are displayed. The blue dots represent the average ranks of time spots as listed, and the length of each horizontal line is equal to the value of critical difference (CD).
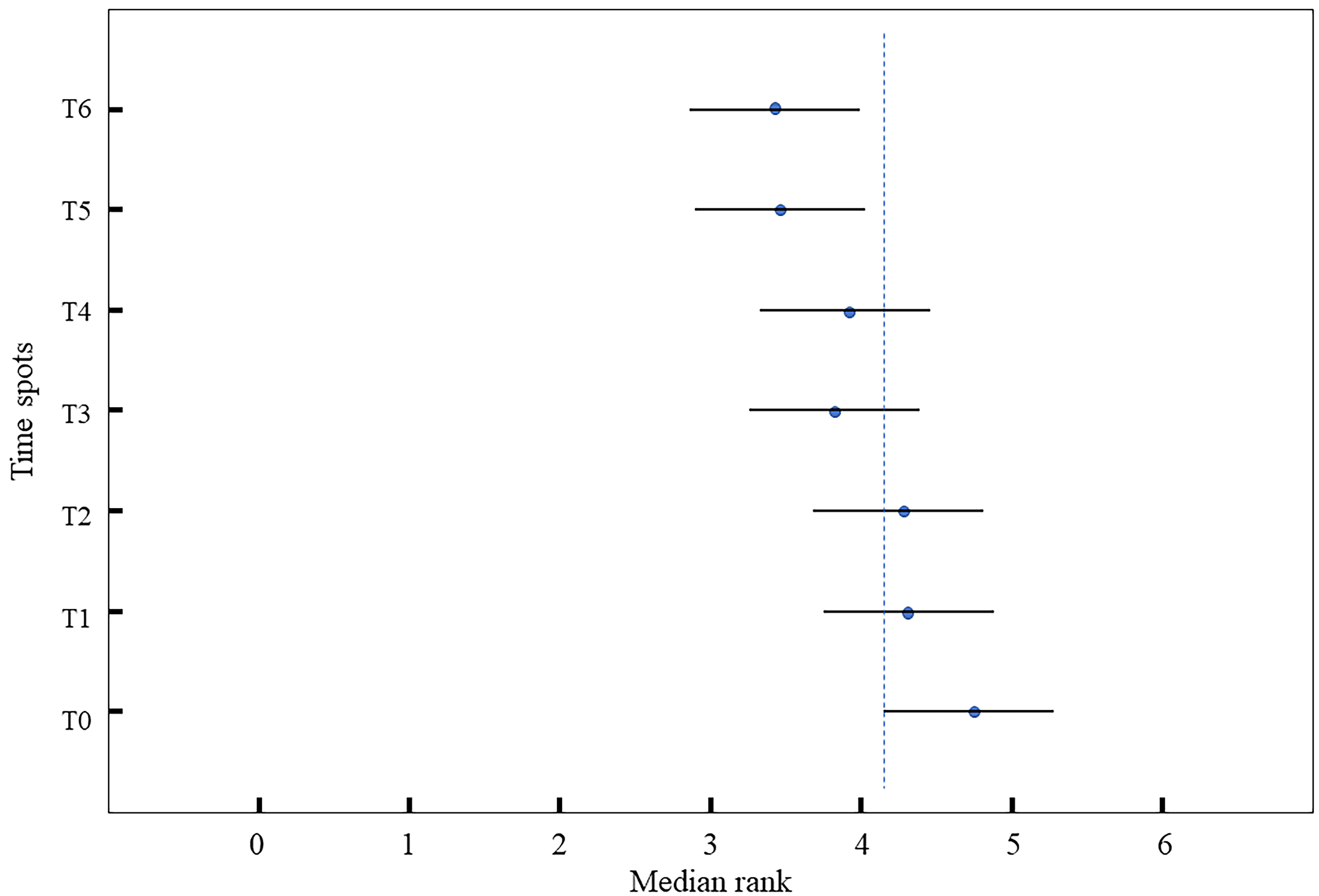
Bacterial loads of the bare arms group showed the result that the colony count
significantly differed at the timeline (Friedman test, p
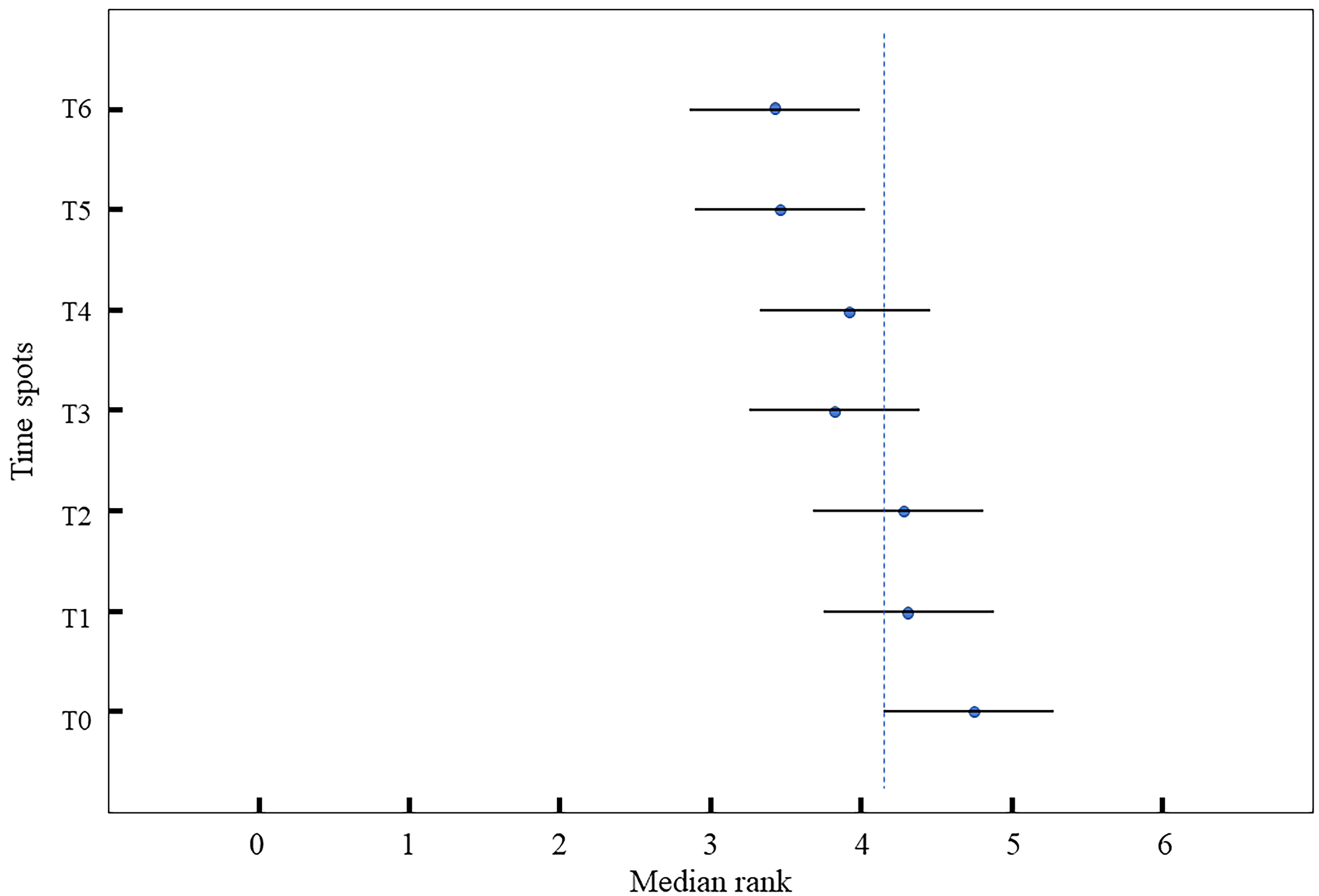 Fig. 4.
Fig. 4.Comparisons at different time spots in the bare arms group. The results of Nemenyi test of the bare arms group are displayed. The blue dots represent the average ranks of time spots as listed, and the length of each horizontal line is equal to the value of CD. The blue dotted line indicates that the gap of average rank is greater than the value of CD between T0 and T6, and between T0 and T5.
Overall, the obtained bacterial loads in the present study appeared to be low
with 75.8% (637/840) of all plates showing no colony count after incubation for
48 h. According to the specification of hand hygiene for healthcare workers from
the National Health Commission of China, effective surgical hand antisepsis
should achieve the monitored bacterial colony count
Before the first procedure, the gowns group significantly had fewer colonies than the bare arms group, regardless of sampling sites. In the case of surgical gowns with apparently good sterility, it is possible since the original bacterial loads and hand hygiene effects varied for each individual. This circumstance could draw attention to the implementation of standard surgical hand-washing procedures to prevent potential contamination. Additionally, for both attires, there was no difference between forearms and wrists observed at the baseline. In later analyses, the same results were observed at each time spot in both groups except that the colony counts of forearms were significantly higher than those of wrists in the group of surgical gowns at T2, T5, and T6. What we found was inconsistent with the current perspective since the wrists of medical practitioners are considered to have a higher risk of being contaminated [7]. Our observation could be explained that due to some specific working gestures including performing ultrasound examinations of the abdomen in pregnant patients, doctors performing amniocentesis have more chance to contaminate forearms and elbows than those performing other medical procedures. The surface of surgical gowns’ elbows and wrists potentially faces a higher risk of being contaminated.
There have long been debates about what to wear while participating in other medical activities, especially in perioperative procedures [8, 9, 10]. Regarding attires in the restricted areas of the operating room, the United States’ Association of Perioperative Nurses (AORN) and the United Kingdom’s National Institute for Health and Care Excellence (NICE) provide completely contradictory recommendations: the former suggests to wear a long-sleeved scrub whereas the latter advocates “bare below the elbows” [11, 12]. Each opinion lacks sufficient and high-quality evidence, which implies that it is tough to specify the relationship between attire, contamination, and infection in the operating room [13, 14]. Obviously there is a huge difference between puncture and normal surgery, and the gowns would definitely be changed after a single case of surgery. For operators in surgical gowns in this present study, the mean colony counts gradually raised from T0 to T6. Although the sterility in all of our samplings is quantified, it still indicated that the effectively sterile duration time of disposable surgical gowns should be noted. A longer duration of amniocenteses than we studied might lead to over contamination of surgical gowns. However, the result was quite surprising that the colony counts of bare-arm operators continuously decreased as time accumulated, which might be a consequence of frequent hand disinfection including the disinfection of the forearm and wrist using alcoholic hand-rub.
In informal interviews with some operators participating in our study, we found that some of them preferred wearing just short-sleeved scrubs for comfort after several hours of continuous work. However, some of them would still prefer to choose a surgical gown, either for the sake of protecting themselves more sufficiently or out of a desire to reduce the irritation of alcoholic hand-rub on a larger area of skin. Therefore, in the case that neither attire is contaminated beyond the standard, it is invalid and pointless to argue about how to dress when performing amniocentesis. With more attention to other infection control measures with stronger evidence, such as high-quality hand hygiene and avoidance of frequent door opening and closing [15, 16, 17], the attire could become an issue that depends on the individual choices of operators.
Some limitations exist in this study. First, this is a study collecting data from a single center, which limits the generalizability of the results. Besides, bacterial loads on the surface of amniocentesis operators were potentially influenced by other covariates including sampling methods, bacterial load of pregnant patient’s skin and cloth, temperature, and humidity. Furthermore, surface bacteria of the operator may not have a direct effect, but rather an indirect effect on operation-related infections by influencing environmental bacterial concentrations. Finally, for the reason of the discrepant number of pregnant patients to be examined at each period, samplings in the present study were done only during two hours of repetitive amniocenteses (30 continuous cases). Hence, our findings might not apply well to longer repetitive operations and particularly inhibit specifying the appropriate wearing length of surgical gowns.
Our data showed eligible bacterial loads on the surface of operators during 30 repetitive amniocenteses both with or without sterile surgical gowns, indicating that both types of attires are proper when performing amniocentesis. For operators in surgical gowns, the extension of operative time might potentially induce the contamination of attires. While dress code could be considered as an individual option, surveillance of hand hygiene and other efficient measures to prevent contamination in the operating room need to be taken into account.
Data are already provided as part of the submitted article.
JW: methodology, formal analysis, writing — original draft, visualization; YS, LS, XL, FZ, QZ, JW, XZ, MY and DX: investigation, resources; TH and SL: conceptualization, supervision, project administration. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
All subjects gave their informed consent for inclusion before they participated in the study, and all physicians agreed to be included in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of West China Second University Hospital of Sichuan University (approval number: 2022(300)).
We gratefully acknowledge the assistance of the amniocentesis operators participating in this study.
This work was supported by National Key Research and Development Program of China (2022YFC2703302).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.