1 Center of Reproductive Medicine, Hangzhou Women’s Hospital, 310008 Hangzhou, Zhejiang, China
Abstract
Background: Missed miscarriage patients with residual tissue in the uterine cavity after medical abortion can be treated by surgery and expectant therapy. Because surgery may cause damage to the endometrium, expectant treatment is preferred clinically. However, the individual probability of expulsion of residual tissue from the uterus remains unelucidated. The present study used logistic regression analysis and nomogram to create a scoring system for quantitatively evaluating the individual probability of residual tissue expulsion in patients with missed miscarriage. Methods: A cohort of 126 patients with missed miscarriage who had residual tissue after medical abortion were included in the trial after receiving their informed consent. Of these patients, 102 and 24 patients had successful and failed expectant treatment, respectively. Results: Logistic regression analysis showed that gravidity, residual tissue size, and residual tissue with blood supply significantly affected the probability of expulsion of residual tissue after medical abortion. A special nomogram was constructed for predicting the probability of successful expulsion. At the maximum Youden index of 0.696, the area under the curve (AUC) of the receiver operating characteristic curve (ROC) was 0.849; this corresponded to a score of 77.78 and probability of residual tissue expulsion of 71%. Conclusion: A scoring system was established based on a nomogram. The success rate of residual tissue expulsion from the uterine cavity was significantly improved at the total score of 77.78 points after assigning influence weights to each influencing factor and an AUC of 0.849.
Keywords
- missed miscarriage
- medical abortion
- residual tissue expulsion
- expectant treatment
- nomogram
Missed miscarriage, also known as late miscarriage, is a pregnancy loss in which a dead fetus or embryo is retained in the maternal uterine cavity without timely spontaneous expulsion, which occurs in approximately 15% of clinical pregnancies [1]. A curettage cannot be easily performed in this condition because the dead embryo or placenta is degenerated or mechanized and adheres closely to the uterine wall.
Conventional treatment of induced abortion includes medication, surgery, and
expectant treatment. Surgical abortion has a higher rate of complete abortion
than medication [2]. However, surgical abortion can damage the basal layer of the
endometrium, resulting in fibrous connective tissue hyperplasia and dysplasia of
endometrial regeneration, resulting in endometrial repair disorder or cavity
adhesions and thereby severely affecting embryo implantation [3]. Endometrial
damage is exacerbated by curettage in patients with missed miscarriage, and a
high number of curettages (
Presently, although many studies have reported on the factors affecting incomplete abortion, the prediction of the probability of successful expulsion of residual tissue from the uterine cavity has not yet been established [8, 9, 10, 11]. Hamel et al. [12] developed and evaluated a clinical model that can predict the probability of successful medical abortion for patients with missed miscarriage, which is based on body mass index, misoprostol pretreatment, presence of symptoms of abdominal pain or vaginal bleeding, and number of previous curettages. Lu et al. [13] investigated the factors that contribute to complete abortion after medical abortion in patients with missed miscarriage, including the size of residual tissue and blood supply. By using recursive partitioning analysis, patients with similar probabilities of complete abortion were classified into individual groups, and the probability of each group was calculated. However, the precise probability could not be derived for each patient.
Nomograms are a common predictive tool for assessing patient prognosis. By integrating diverse predictive and decision variables, individual numerical probabilities of clinical events are generated to meet the requirement for personalized medicine [14]. Based on recent methodological guidelines for prognostic modeling [15, 16], in the present study, we developed a scoring system through logistic regression analysis and a nomogram and assessed the feasibility of prediction with receiver operating characteristic (ROC) curves and calibration curves. This approach can enable to quantitatively evaluate the individual probability of expulsion of residual tissue from the uterus and to provide personalized guidance to patients with missed miscarriage.
This prospective study included 126 women diagnosed to have missed miscarriage with residual pregnancy tissue in the uterine cavity after medical abortion at Hangzhou Women’s Hospital (Zhejiang, China) between March 2021 and March 2023. The patients’ age ranged from 25 to 45 years, with gestational age at 6 to 12 weeks. Among these 126 patients, spontaneous expulsion of residual tissue occurred in 102 patients, while in 24 patients, residual tissue was removed by curettage or hysteroscopy.
The inclusion criteria were as follows: (1) patient met the diagnostic criteria for missed miscarriage [17] and received the following medication regimen: three doses of mifepristone (H10950347, Zhejiang Xianju Pharmaceutical Co., LTD., Xianju, Zhejiang, China) 150 mg totally + misoprostol (H20000668, Huarun Zizhu Pharmaceutical Co., LTD., Beijing, China) 600 µg on the third day. After 3 h of oral misoprostol administration, if there was no expulsion of the pregnancy sac, misoprostol (400 µg) was given orally; (2) there were contraindications to medical abortion, such as cardiovascular disease, glaucoma, asthma, and allergy; (3) patients underwent routine vaginal ultrasonography on the first day after medical abortion. Patients with ultrasound findings suggestive of residual tissue in the uterine cavity were included in this study. Patients were excluded from the study if they showed more vaginal bleeding than menstrual bleeding during the expectant treatment or a previous diagnosis of irregular menstruation.
Menstruation resumed around 30 days after abortion. After the first menstruation, ultrasound was performed to confirm the expulsion of residual tissue from the uterine cavity. Women with no residual tissue in the uterine cavity were considered to have successful outcome of the expectant treatment.
The following clinical factors were analyzed: age, gravidity, parity, and number of miscarriages; history of missed miscarriage, cesarean section, hysteroscopy, and fetus protection; in vitro fertilization (IVF) or natural conception; gestational age; week at which pregnancy was terminated; period at which embryo growth stopped; residual tissue size (mean value of three diameters of residual tissue); and residual tissue with blood supply or no blood supply.
Univariate logistic regression analysis was performed sequentially for all factors and outcome (expulsion of residual tissue from the uterine cavity). The posterior elimination method was used for the screening of relevant variables with a screening threshold of 0.1. Subsequently, multivariate logistic regression analysis was performed for the screened relevant variables and outcome. The factors influencing the expulsion of residual tissue from the uterine cavity were then determined.
According to the coefficients of the multivariate logistic regression analysis, quantitative evaluation was performed for the influence the weight of each relevant influencing factor on the probability of successful expulsion of intrauterine residual tissue after medical abortion in patients with missed miscarriage [18, 19, 20]. Influence weights were assigned to each influencing factor, and the scores obtained for each factor were then summed. Subsequently, based on the total scores, a nomogram was constructed according to the regression model, and the corresponding total scores were marked on the total score scale in the nomogram. Finally, a vertical line was drawn on the scale to determine the probability of successful expulsion of residual tissue. The corresponding value indicated the probability of successful expulsion of residual tissue after medical abortion in the patient with missed miscarriage.
The total score of the nomogram was used as the independent variable and analyzed by the logistic regression method with the outcome variable. A ROC curve was then plotted. The area under the ROC curve (AUC) value was used to validate the feasibility of prediction, and the Youden index was used to determine the threshold value.
All data were statistically analyzed by SAS version 9.4 software (Raleigh, NC, USA). Univariate and multivariate logistic regression analyses were
conducted, and a nomogram was constructed. ROC and calibration curves were used
to internally validate the feasibility of the predictions, and the threshold
value was determined using the Youden index. Differences were considered
statistically significant at p
The continuous variable was tested and conforms to a normal distribution. The
univariate analysis of clinically relevant factors in both groups of patients
showed that gravidity, residual tissue size, and residual tissue with blood
supply significantly influenced the expulsion of residual tissue from the uterine
cavity after medical abortion in patients with missed miscarriage (p
| Characteristics | No residual | With residual | χ |
p | |
| (n = 102) | (n = 24) | ||||
| Age | 32.074 |
32.915 |
0.044 | 0.965 | |
| Gravidity | 4.424 | 0.035 | |||
| 1 | 54 (52.941%) | 6 (25.000%) | |||
| 48 (47.059%) | 18 (75.000%) | ||||
| Parity | 2.961 | 0.085 | |||
| 0 | 74 (72.549%) | 14 (58.333%) | |||
| 28 (27.451%) | 10 (41.667%) | ||||
| Number of abortions | 0.110 | 0.740 | |||
| 0 | 70 (68.627%) | 14 (58.333%) | |||
| 32 (31.373%) | 10 (41.667%) | ||||
| History of missed miscarriage | 3.638 | 0.056 | |||
| No | 94 (92.157%) | 16 (66.667%) | |||
| Yes | 8 (7.843%) | 8 (33.333%) | |||
| History of cesarean section | |||||
| No | 94 (92.157%) | 22 (91.670%) | |||
| Yes | 8 (7.843%) | 2 (8.333%) | |||
| History of hysteroscopy | 0.043 | 0.836 | |||
| No | 88 (86.274%) | 22 (91.667%) | |||
| Yes | 14 (13.725%) | 2 (8.333%) | |||
| History of fetus protection | 2.741 | 0.098 | |||
| No | 46 (45.098%) | 14 (58.333%) | |||
| Yes | 56 (54.902%) | 10 (41.667%) | |||
| IVF | |||||
| No | 94 (92.157%) | 22 (91.667%) | |||
| Yes | 8 (7.843%) | 2 (8.333%) | |||
| Gestational age | 9.543 |
9.656 |
0.687 | 0.493 | |
| Week of pregnancy stopped | 7.001 |
7.082 |
0.130 | 0.897 | |
| Period of embryo stopped | 2.542 |
2.504 |
0.242 | 0.809 | |
| Residual size | 1.551 |
2.483 |
4.267 | ||
| Residual with blood supply | 12.498 | ||||
| No | 62 (60.784%) | 4 (16.667%) | |||
| Yes | 40 (39.216%) | 20 (83.333%) | |||
Data are presented as n (%) and mean
IVF, in vitro fertilization; SD, standard deviation.
Multivariate analysis was conducted using the forward Wald method by including
the significant univariate factors into the equation. The results showed that
gravidity (odds ratio [OR] = 3.252, 95% confidence interval [CI]: 1.674–6.316),
residual size (OR = 7.465, 95% CI: 2.093–26.619), and residual with blood
supply (OR = 7.086, 95% CI: 2.024–24.806) were the critical factors that
influenced the expulsion of residual tissue after medical abortion in patients
with missed miscarriage (all p
| Variables | No residual | With residual | OR | 95% CI | p | aOR | 95% CI | Adjusted p | |
| (n = 102) | (n = 24) | ||||||||
| Gravidity | |||||||||
| 1 | 54 (52.941%) | 6 (25.000%) | 3.375 | (1.239–9.196) | 0.017 | 3.252 | (1.674–6.316) | ||
| 48 (47.059%) | 18 (75.000%) | ||||||||
| Residual size | 1.551 |
2.483 |
3.284 | (1.833–5.883) | 7.465 | (2.093–26.619) | 0.002 | ||
| Blood supply | |||||||||
| No | 62 (60.784%) | 4 (16.667%) | 7.750 | (2.467–24.348) | 7.086 | (2.024–24.806) | 0.002 | ||
| Yes | 40 (39.216) | 20 (83.333%) | |||||||
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval.
Blood supply, residual tissue with blood supply.
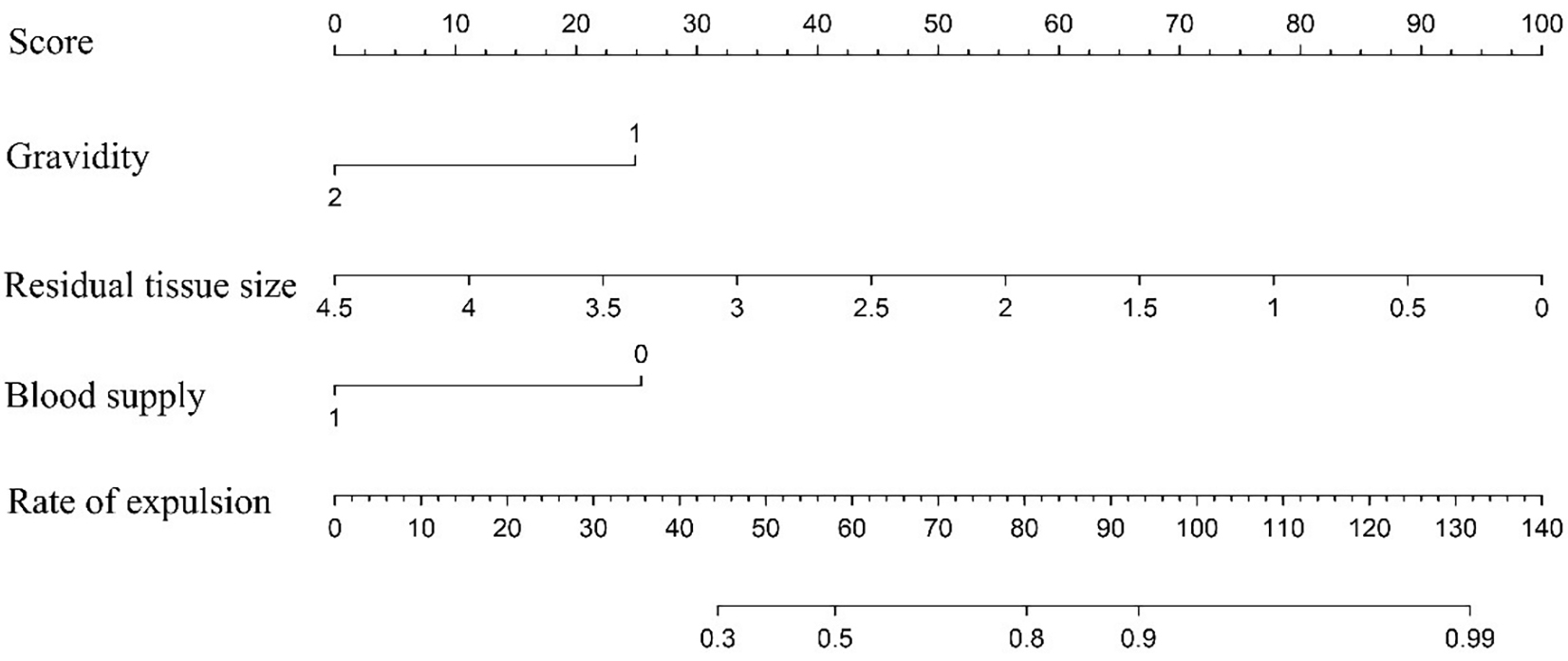
After assigning influence weights to the influencing factors [21], the influence
of each factor was determined as follows: 24.88 points for first pregnancy; 0
points for
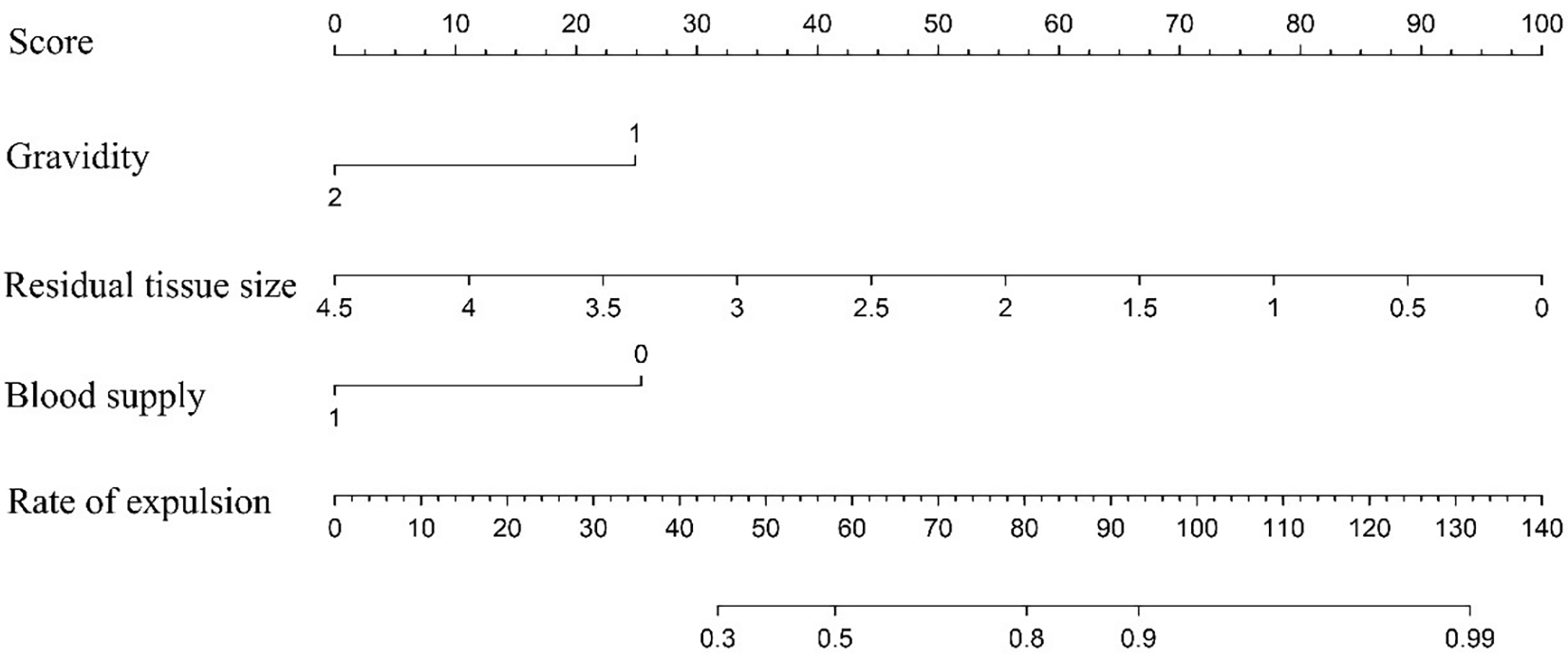 Fig. 1.
Fig. 1.Nomogram for predicting the probability of successful expulsion of residual pregnancy tissue after medical abortion for patients with missed miscarriage. Each factor (gravidity, residual tissue size, and residual tissue with blood supply) was assigned a score on the point scale, which was determined by drawing a vertical line from the factor scale to the point scale. The estimated probability of successful expulsion was calculated by adding points to generate total points and locating this score on the total point scale.
| Factors | Coefficient | State | Score | |
| Gravidity | ||||
| 1 | –1.552 | 1 | 24.88 | |
| 0 | 0 | |||
| Residual size (1.7 |
–1.387 | 1 cm | 11.11 | |
| Blood supply | ||||
| No | –1.584 | no (= 0) | 25.38 | |
| Yes | 0 | yes (= 1) | 0 | |
Blood supply, residual tissue with blood supply.
The corresponding nomogram was then constructed to predict the probability of successful expulsion of residual pregnancy tissue after medical abortion for patients with missed miscarriage (Fig. 1).
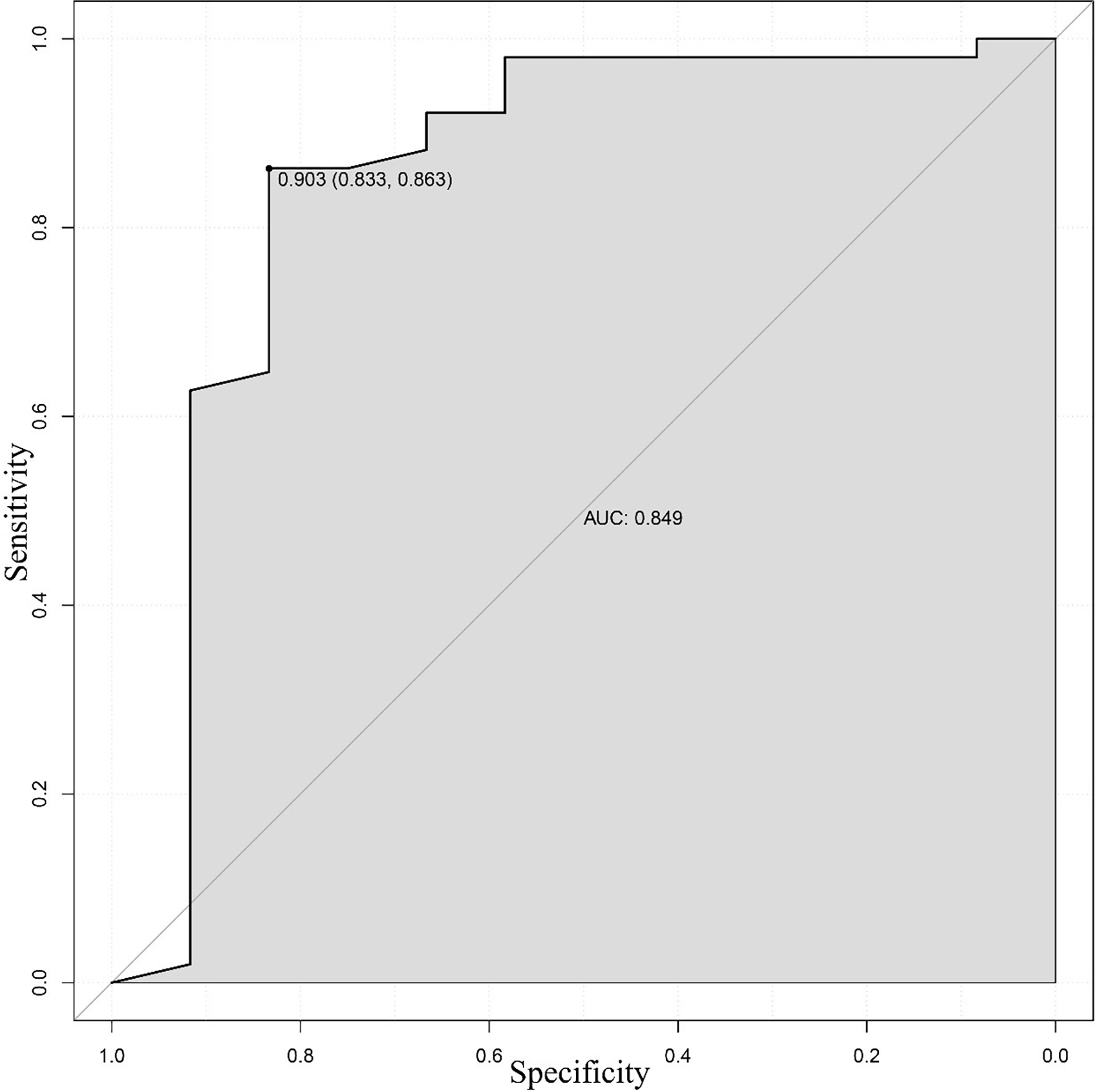
At the maximum value of the Youden index (0.696), the AUC value of the ROC was 0.849, which corresponded to a score of 77.78 and probability of successful expulsion of 71% (Fig. 2).
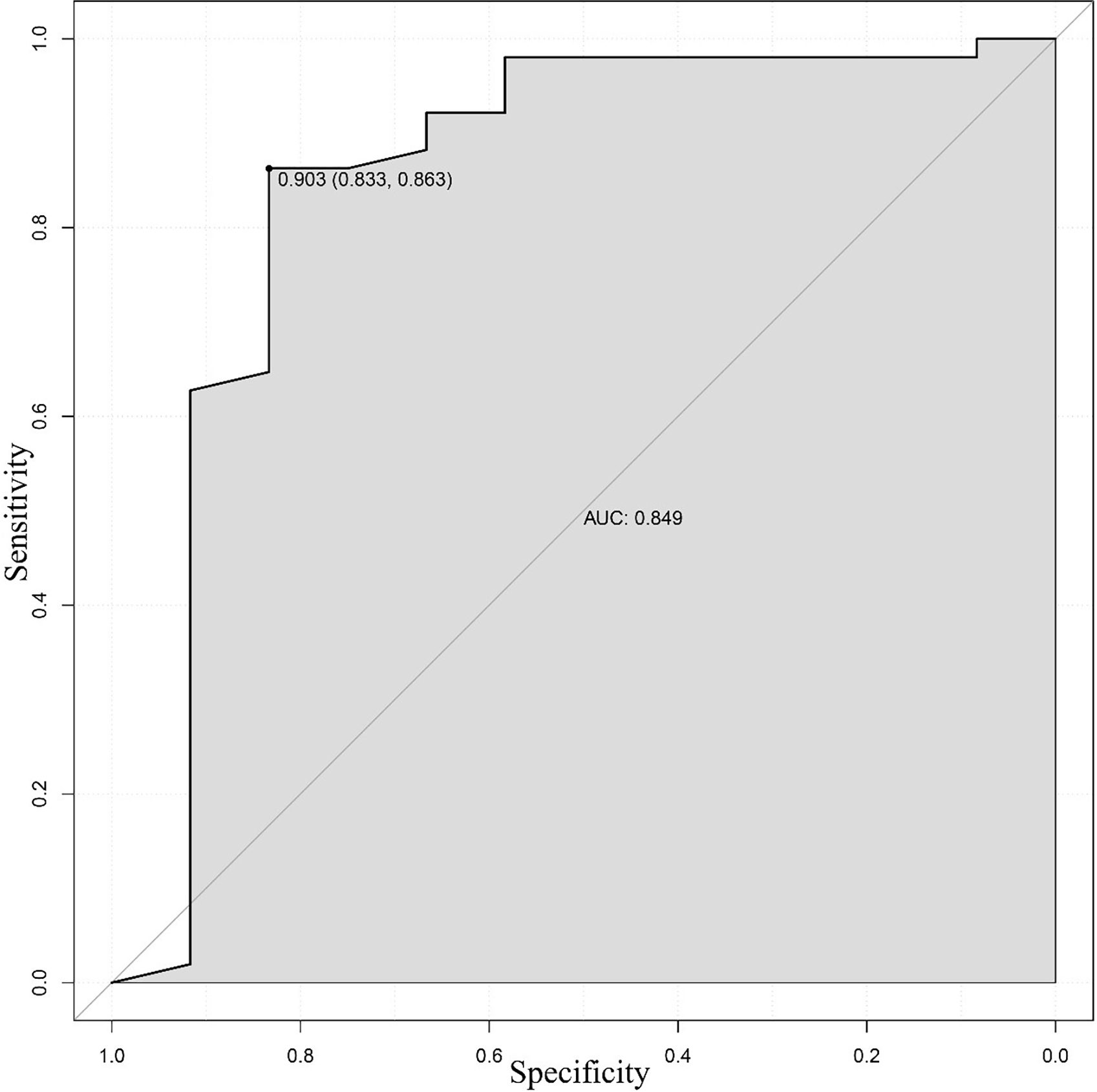 Fig. 2.
Fig. 2.Receiver operating characteristic curve (ROC) curve of the nomogram for predicting the probability of successful expulsion of residual tissue from the uterine cavity. The area under the curve (AUC) value of 0.849 indicated reasonable discriminative performance.
Many studies have reported the predictors of success of medical abortion or
incomplete abortion. However, inconsistencies were observed in defining the
precise predictors of success of medical abortion, mainly because of differences
in study populations, dosage and administration route of misoprostol,
administration regimen, and the timing and criteria for the ultrasonographic
assessment of a complete abortion [22]. In some studies, an endometrial thickness
of
In the present study, ultrasonography was performed on the first day after
medical abortion in patients with missed miscarriage. Based on ultrasonography
findings and clinical factors, univariate and multivariate logistic regression
analyses were conducted to determine the predictive factors for the expulsion of
intrauterine residual tissue from the uterine cavity of these patients. The
possibilities for the expulsion of the residual tissue from the uterine cavity
were then explored. We found that three factors, namely gravidity, residual
tissue size, and residual tissue with blood supply, significantly affected the
expulsion of residual tissue from the uterine cavity after medical abortion for
patients with missed miscarriage (all p
The current study suggests that low gravidity, smaller residual size, and
residue tissue with no blood supply are the favorable factors for the expulsion
of residual tissue from the uterine cavity after medical abortion. A multicenter
randomized controlled clinical trial also showed that nulliparity was associated
with the success rate of medical abortion, thus suggesting that the
responsiveness of the uterus to misoprostol varies with the growth and extension
of the uterus in past pregnancies [25]. Reeves et al. [26] showed that
five or more deliveries (absolute risk: 11.90%, OR: 4.60%) and gestational age
of
Fernlund et al. [27] conducted a secondary analysis of published
prospective clinical trials and showed that the success rate of expectant
treatment for anembryonic miscarriages increased with gestational age and
crown-rump length, but further increased with the decrease in the diameter of the
gestational sac. The authors also found that lower levels of serum progesterone
(P) or serum
In another prospective study, residual tissue width and blood supply were found
to be significant predictors (p
To date, few studies have investigated the precise probability of expulsion of residual tissue from the uterine cavity. The main advantage of using a nomogram is the ability to estimate individualized risks based on patient and disease characteristics and to generate individual probabilities of clinical events [30, 31]. Therefore, in the present study, we established a scoring system based on a nomogram. For example, a patient was assigned a value for each variable through the rating scale, and the variable was assigned a total score of 90, which corresponds to a probability of residual expulsion of 88% according to the nomogram. Thus, the total score of the influencing factors was 90, which was higher than the threshold value of 77.78, and the probability of successful natural expulsion of residual tissue from the uterus was approximately 88%. Based on these values, the patient was recommended to wait for the natural expulsion of residual tissue and to presently avoid the clearance of the uterus [32, 33].
The present study has some limitations. First, serum HCG and progesterone levels of the patients were not tested because the results of these tests require a waiting period and prompt clinical management of these patients is required for informed decision-making. Second, the sample size was too small, and we hope that subsequent studies will be conducted with a larger sample size. We also plan to use this scoring system in clinical settings and determine its clinical validity by comparing the curettage rate, complications after abortion such as endometritis and uterine adhesions, and clinical pregnancy rate.
In summary, a scoring system based on the developed nomogram was established to quantitatively evaluate the probability of expulsion. At the total score of 77.78 for the assigned weights, the AUC of the ROC curve was 0.849, and the probability of successful expulsion of residual tissue from the uterine cavity was 71% for patients with missed miscarriage after medical abortion.
Obtain availability of data and materials through corresponding author email.
HHZ: Conceptualization, data curation, data analysis, writing - original draft. MYJ: Conceptualization, data curation, obtained informed consent. JH: Data analysis, writing - review and editing. ZYL: The acquisition, analysis, or interpretation of data for the work. HYZ: Conceptualization, formal analysis, data analysis, writing - review and editing. All authors approved the final version of the manuscript to be published. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work to take public responsibility for appropriate portions of the content and agreed to be accountable for all aspects of the work in ensuring that questions related to its accuracy or integrity.
The present study was approved by the Ethics Committee of Hangzhou Women’s Hospital (no.: [2021] medical ethics (007) No.12), and informed consent was obtained from all the included participants.
We thank International Science Editing for editing this manuscript.
The study was supported by the project from Zhejiang Province Science and Technology Program [2022KY1018].
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.