1 Videourodynamic Studies Center, Department of Urology, The Second Affiliated Hospital of Guilin Medical University, 541199 Guilin, Guangxi, China
2 Continence Research Clinic, Department of Urology, Shaoyang Central Hospital, 422000 Shaoyang, Hunan, China
3 Department of Urology, Shaoyang Hosptial Affiliated to University of South China, 422000 Shaoyang, Hunan, China
4 School of Pharmacy, Macau University of Science and Technology, 999078 Macau, China
5 Department of Urology, Guilin Hospital of the Second Xiangya Hospital, Central South University, 541001 Guilin, Guangxi, China
6 Department of Operation Room, The Second Affiliated Hospital of Guilin Medical University, 541199 Guilin, Guangxi, China
†These authors contributed equally.
Abstract
Failure to standardize bladder volume in the evaluation of stress urinary incontinence (SUI) may be a contributing factor to the controversy surrounding the diagnostic and prognostic efficacy of urodynamic studies (UDS) in female patients with SUI. This study was conducted to explore the effects of bladder volume on the urethral mobility in female patients with SUI under increased intra-abdominal pressure.
This prospective study enrolled uncomplicated female patients with SUI admitted to the Second Affiliated Hospital of Guilin Medical University and Shaoyang Central Hospital, between January 2021 and January 2024. Relative bladder neck descent (BND), urethral inclination angle (UTA), urethral rotation angle (URA), and posterior urethrovesical angle (PUVA) were compared across different bladder volumes (100 mL, 200 mL, and 300 mL) at resting state or 90 cm H2O of intravesical pressure, generated by Valsava movement, using sonography videourodynamic studies (SVUDS). Analysis of variance (ANOVA) was used to compare numerical data of parameters with a normal distribution.
62 patients were enrolled in this study. There was not a significant difference in UTA and PUVA among the various bladder volumes (100 mL, 200 mL, and 300 mL) at resting state (all p >0.05). However, higher BND (2.23 ± 0.73 cm), UTA (44.7 ± 17.1°), URA (29.4 ± 16.0°), and PUVA (148.7 ± 21.4°) were determined at a bladder volume of 200 mL with the Valsalva movement (VM) reaching 90 cm H2O of intravesical pressure, compared to 100 mL (1.89 ± 0.74 cm, 38.1 ± 17.9°, 23.0 ± 15.5°, and 139.3 ± 19.8°) and 300 mL (1.85 ± 0.74 cm, 37.6 ± 18.8°, 23.8 ± 13.5°, and 143.4 ± 20.8°) (all p <0.05), except for PUVA between 200 mL and 300 mL (p = 0.161).
Higher values of BND, UTA, URA, and PUVA at a bladder volume of 200 mL in the Valsalva state of female patients with SUI, compared to 100 mL and 300 mL, suggest that capacity of 200 mL should be standardized for evaluating female SUI.
Keywords
- female stress urinary incontinence
- urethral mobility
- bladder volume
- Valsalva movement
- sonography videourodynamic studies
There is a global consensus that the high incidence of stress urinary incontinence (SUI), defined by the International Continence Society (ICS) as “the involuntary leakage of urine associated with exertion, or sneezing, or coughing”, leads to significant consumption of healthcare resources and contributes to considerable anxiety and depression in elderly female patients [1]. Both urethral hypermobility (UH) and intrinsic sphincter deficiency (ISD) have been considered to be involved in the pathophysiological process of SUI. The differentiation between UH and ISD has traditionally played an important role in treatment choice for SUI, as ISD with fixed urethra may be a risk factor for transobturator tape (TOT) failure, although conflicting findings have been reported [2]. Urodynamic studies (UDS) have been used to defined ISD as a Valsalva leak point pressure (VLPP) of less than 60 cm H2O and a maximal urethral closure pressure (MUCP) of less than 20 cm H2O, respectively. Therefore, UDS are believed to be prognostic for female patients with complicated SUI, as previous studies have shown both objective and subjective improvements in surgical outcomes for SUI when preoperative UDS is used [3]. Videourodynamic studies (VUDS) are suggested to have the best utility in evaluating the degree of bladder neck/urethra hypermobility, and the Blaivis grading system for UDS was defined using VUDS [4].
However, a decreased in the proportion of female patients with uncomplicated SUI undergoing preoperative UDS has been observed since the publication of the results of the Value of Urodynamic Evaluation (VALUE) study in 2012, which demonstrated that UDS did not improve treatment outcomes or reduce adverse events [5]. However, an identical recommended bladder volume and intravesical pressure have not been reported during preoperative UDS in patients enrolled in the VALUE study [5]. Hence, it has been suggested that the lack of standardization in the performance of UDS and transperineal ultrasound for the evaluation of SUI, as pointed out by several authors, may explain the controversies regarding the value of preoperative UDS in female patients with SUI in the literature [6, 7]. Therefore, uncomplicated female patients with SUI were enrolled in a prospective study. Urethral mobility was determined at different bladder volume (100 mL, 200 mL, and 300 mL) in both resting or Valsalva states using sonography videourodynamic studies (SVUDS) to explore the effects of bladder volume on urethral mobility, providing insights for the standardization of examination methods for SUI.
We enrolled women underwent SVUDS at The Second Affiliated Hospital of Guilin Medical University and Shaoyang Central Hospital between January 2021 and January 2024 into this study. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki, and informed consent was obtained from all subjects. The study was approved by the Medical Ethics Committee of the Second Affiliated Hospital of Guilin Medical University (EFY-GZR2022011) and Shaoyang Central Hospital (2022070).
The inclusion criteria were as follows: (1) uncomplicated female patients with SUI, (2) aged 18 years or older, (3) clear understanding and willingness to participate in the study, and (4) a bladder volume of at least 300 mL reached during SVUDS. The exclusion criteria for this study were as follows: (1) female patients with ISD, (2) urgency urinary incontinence (UUI), (3) mixed urinary incontinence (MUI), (4) neurogenic bladder, (5) previous pelvic or urethral surgery, (6) medications affecting lower urinary tract, (7) severe cardiovascular or pulmonary diseases, and (8) inability to reach a maximum bladder volume of 300 mL or a maximum intravesical pressure of 90 cm H2O during SVUDS. The sample size was calculated using PASS software (version 15.0, NCSS, Kaysville, UT, USA) with 90% power to detect a difference, a 5% level of significance, assuming a mean difference of 0.51 cm in relative bladder neck descent (BND) between 100 mL and 200 mL, and a standard deviation (SD) of 0.64, based on preliminary data from 20 patients. The calculated sample size was at least 42, and 62 female patients were recruited for this study.
The effects of bladder volume on urethral mobility, including BND, urethral inclination angle (UTA), urethral rotation angle (URA), and posterior urethrovesical angle (PUVA), in both resting or Valsalva states, were evaluated using SVUDS. SVUDS combines an ultrasound scan with multichannel UDS (Laborie Aquarius XT, Portsmouth, NH, USA) and can synchronously integrate urodynamic measurements with video or image sequences using its proprietary software (UDS.V14), as described in our previous study [8].
The patient was positioned in a semi-sitting posture, with the hip flexor slightly abducting, and the perineum was carefully disinfected. Intravesical and abdominal pressures were measured using a 6-Fr double-lumen and 8-Fr single-lumen UDS catheter respectively, both connected to a multichannel UDS system. Next, 37 °C normal saline was instilled into the patient’s bladder at a rate of 30 mL/s. Bladder symphyseal distance (BSD) , UTA, URA, and PUVA at bladder volumes of 100 mL, 200 mL, and 300 mL during resting or Valsalva movement (VM), through which 90 cm H2O of intravesical pressure was reached, were measured by a single urologist using transperineal ultrasound (DC-65 Mindray, ShenZhen, Guangdong, China) with a 7.5-MHz linear array probe during SVUDS, as described in previous reports [7, 9, 10]. In this study, BND was defined as the vertical difference in BSD between VM and resting states. Subsequently, comparisons of UTA and PUVA across different bladder volumes (100 mL, 200 mL, and 300 mL) at resting state, as well as BND, UTA, URA, and PUVA at 90 cm H2O of intravesical pressure across different bladder volumes, were performed. Each patient was reexamined three times. All SVUDS were conducted by a urologist in accordance with the good urodynamic practices of the ICS [11].
The data for parameters, including BND, UTA, URA, and PUVA, derived from
different bladder volumes at resting and Valsalva states, were tested for
normality distribution using the Kolmogorov-Smirnov test and are presented as
means
A total of 62 female patients with SUI, aged between 38 years and 82 years old (57.2
| Total N = 62 | ||
| Age (years, mean |
57.2 | |
| POP | 31 (50.0%) | |
| Parity | ||
| 1 | 21 (33.9%) | |
| 2 | 26 (41.9%) | |
| 3 | 13 (21.0%) | |
| 4 | 2 (3.2%) | |
POP, pelvic organ prolapse; SD, standard deviation; N, number.
| 100 mL (n = 62) | 200 mL (n = 62) | 300 mL (n = 62) | F | p-value | |
| UTAR (°) | 15.0 |
14.9 |
15.2 |
0.074 | 0.929 |
| PUVAR (°) | 120.7 |
125.1 |
128.6 |
2.695 | 0.070 |
UTAR, urethral tilt angle at resting; PUVAR, poster posterior urethrovesical angle at resting.
However, significant differences were observed in BND, UTA, URA, and PUVA across
different bladder volumes (100 mL, 200 mL, and 300 mL) when patients performed
Valsalva movement to achieve an intravesical pressure of 90 cm H2O (all
p
| 100 mL (n = 62) | 200 mL (n = 62) | 300 mL (n = 62) | F | p-value | |
| BNDVM (cm) | 1.89 |
2.23 |
1.85 |
5.138 | 0.007 |
| UTAVM (°) | 38.1 |
44.7 |
37.6 |
3.059 | 0.049 |
| URAVM (°) | 23.0 |
29.4 |
23.8 |
3.338 | 0.038 |
| PUVAVM (°) | 139.3 |
148.7 |
143.4 |
3.215 | 0.042 |
BNDVM, bladder neck descent at 90 cm H2O of intravesical pressure when Valsalva movement; UTAVM, urethral tilt angle at 90 cm H2O of intravesical pressure when Valsalva movement; URAVM, urethral rotation angle at 90 cm H2O of intravesical pressure when Valsalva movement; PUVAVM, posterior urethrovesical angle at 90 cm H2O of intravesical pressure when Valsalva movement.
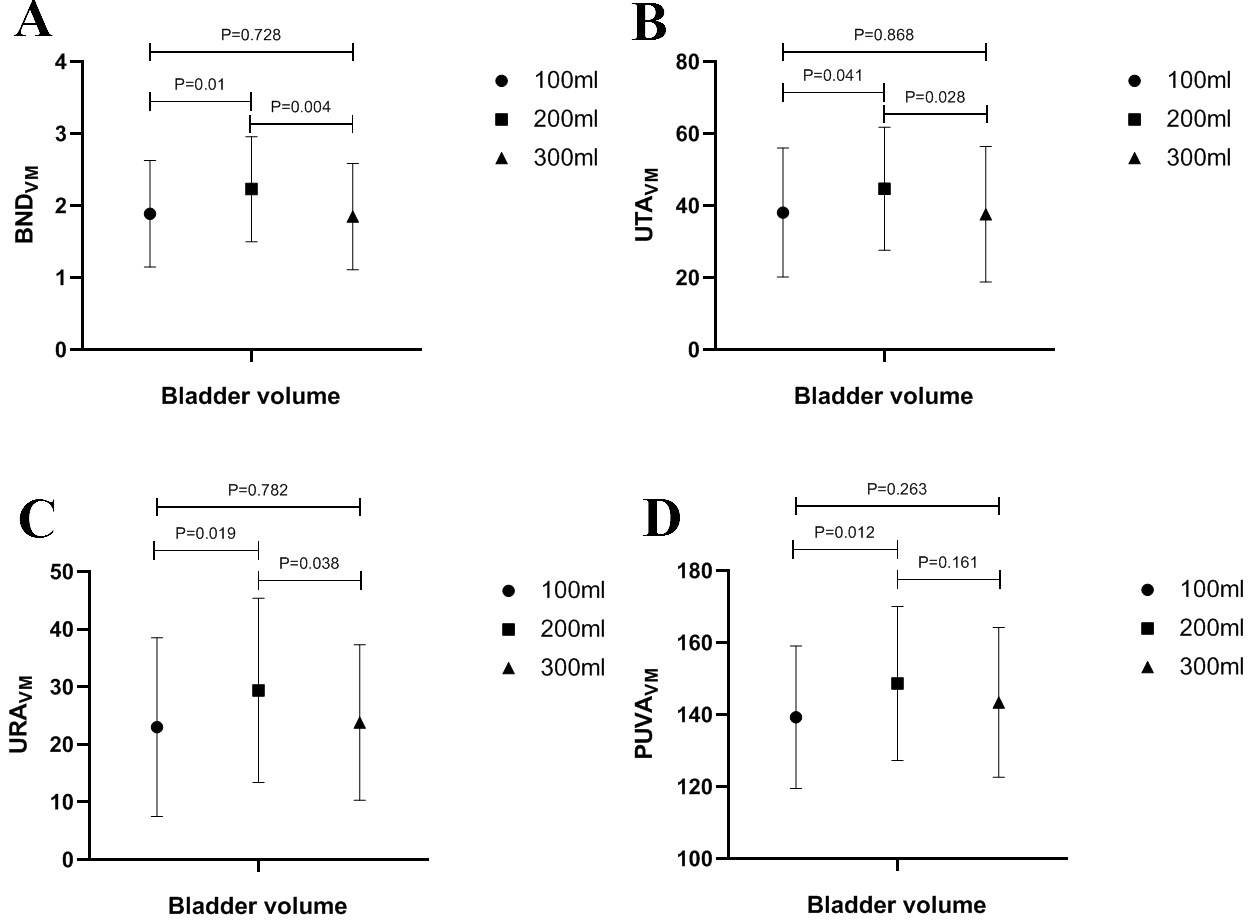 Fig. 1.
Fig. 1.
Comparison of (A) BND𝐕𝐌; (B) UTA𝐕𝐌; (C) URA𝐕𝐌; and (D) PUVA𝐕𝐌 at 90 cm H2O of intravesical pressure when Valsalva movement between 100 mL, 200 mL, and 300 mL of bladder volume. BNDVM, bladder neck descent at 90 cm H2O of intravesical pressure when Valsalva movement; UTAVM, urethral tilt angle at 90 cm H2O of intravesical pressure when Valsalva movement; URAVM, urethral rotation angle at 90 cm H2O of intravesical pressure when Valsalva movement; PUVAVM, posterior urethrovesical angle at 90 cm H2O of intravesical pressure when Valsalva movement.
The reported prevalence of SUI in adult women varies widely, ranging from 23% to 68% globally. The introduction of new treatments relies heavily on demonstrating efficacy and appropriate patient selection, as treatment outcomes for SUI are believed to be closely associated to its classification [12]. However, unsatisfactory prognosis with both conservative and surgical treatments are not uncommon, despite careful diagnosis, appropriate treatment selection, and substantial consumption of healthcare resources [13]. Accordingly, there is a continued need for effective and clear classification systems, as well as ongoing exploration to achieve a comprehensive understanding of the pathogenesis, diagnosis, and treatment of SUI.
Urinary continence in adult women requires several coordinated mechanisms: involuntary tonic contraction of the sphincter and intrinsic urethral smooth muscles during the storage phase at rest; reflexive phasic contraction of the intrinsic muscles in the posterior urethra during physical stress; voluntary phasic contraction of sphincter muscles of bladder outlet when micturition is not appropriate; “coaptation” of urethral wall due to healthy vascularization of the urethral mucosa and submucosa; and an intact nervous system that controls both storage and micturition processes [14]. Beside normal function of the muscle, vascular, and nervous systems, the “hammock hypothesis” has been proposed. This hypothesis suggests that the anterior vaginal wall, integrated with the bony pelvis and relevant ligaments, provides necessary support to counteract the increased intra-abdominal pressure on the urethra through direct transmission of pressure [15]. While direct trauma to those muscular or neurological conditions affecting the sacral spinal cord or Onuf’s nucleus place women at risk of SUI in the form of ISD, impairment of the supportive construction of the “hammock” causes UH. Therefore, it is widely accepted that the involvement of both anatomical and functional etiologies in SUI can been attributed to interconnection between ISD and UH [16].
Although VUDS has been used to differentiate between ISD and UH, controversial outcomes have been reported regarding its role and utility as a diagnostic and prognostic tool for female patients with SUI [17]. However, a lack of standardization in bladder volume during research for diagnosing and classifying SUI has consistently existed. For instance, Dietz and Wilson in 1999 [18] indicated greater mobility of the urethrovesical junction at a 50 mL of bladder volume compared to maximum capacity (mean 355 mL, range 125–470 mL), which may contribute to the conflicting opinions regarding the value of UDS before surgery for SUI [1, 4, 7, 17, 18, 19]. Therefore, a bladder volume of 200 mL may be the most appropriate capacity for evaluating SUI, regardless of whether using UDS or sonography techniques are used. This is supported by the finding in this study that more significant UH was detected at 200 mL compared to 100 mL and 300 mL, when Valsalva movement was performed to achieve 90 cm H2O of intravesical pressure in female patients with SUI. This is the first study to explore the effect of bladder volume on urethral mobility during both resting and Valsalva state, and to identify an appropriate bladder volume for initial standardization in the assessment of SUI.
In this study, the urethral mobility, including BND, UTA, URA, and PUVA, was assessed in female patients with SUI. All the parameters were greater at bladder volume of 200 mL compared to 100 mL and 300 mL during Valsalva movement, while UTA and PUVA remained statistically identical across different bladder volumes at rest. Ji et al. [20] found that BND, URA, and PUVA were all higher in female patients who had undergone hysterectomy compared to those who had not, using transperineal ultrasound (TPUS). Hysterectomy has also been reported to be associated with a higher incidence of UH and SUI. Lin et al. [21] conducted three-dimensional (3D) ultrasound of the pelvic floor in female patients with pelvic floor dysfunction (PFD) and found that elevated BND, UTA, URA, and PUVA were associated with increased incidence of PFD, leading to UH and SUI. Turkoglu et al. [10] reported that the cut-off points for UTA and BND in the diagnosis of stress incontinence were 16° (80% sensitivity, 98% specificity) and 11 mm (90% sensitivity, 98% specificity), both of which were lower than the values found in this study. Thus, it was suggested that more pronounced urethral mobility at a bladder volume of 200 mL was observed compared to 100 mL and 300 mL when subjected to increased intra-abdominal pressure. A bladder volume of 200 mL may therefore be considered an optimal volume for the evaluation of female patients with SUI.
The selection of bladder volume of 100 mL, 200 mL, and 300 mL for evaluating the
effects of bladder volume on urethral mobility was based on our previous studies
and good urodynamic practices of ICS [8, 11].
Therefore, the 100 mL of interval between
different bladder volumes facilitated the determination of the degree of UH
within a limited time, no more than 3.5 min, using ultrasound, due to the bladder
filling rate of 30 mL/min. VLPP is defined as the intravesical pressure at which
urine leakage occurs in absence of detrusor contraction. VLPP values below 60 cm
H2O are typically associated with ISD, while UH is more commonly associated
with VLPP
To explain this finding in the present study, we hypothesized that larger bladder volume (300 mL) may increase the surface cross-sectional area of the bladder while limiting the available pelvic space around bladder. This restriction could, in turn, limit urethral mobility, as the mobility of the bladder neck and urethra is inevitably influenced by the overall mobility of the entire bladder. On the other hand, despite the increased pelvic space around the bladder, the limited surface cross-sectional area of a small bladder (100 mL) may be less able to withstand abdominal pressure, which could result in a reduced degree of urethral mobility, as observed in this study. Therefore, a moderately filled bladder (200 mL) may strike a balance between the surface cross-sectional area and the available pelvic space, leading to greater urethral mobility. However, this hypothesis needs to be validated through simulation research using computer model construction or a physical model in the future.
Several limitations of the present study should be acknowledged. Firstly, the relatively small size of this study should be considered. Secondly, only uncomplicated female patients with SUI were enrolled in this study. Therefore, including a more diverse population, such as female patients with UUI and MUI, could enhance the evaluation of generalizability of our resulted. Thirdly, age bias may arise from the wide age range, spanning from 38 years to 82 years old, in patients enrolled in this study. Finally, urethral mobility of patients was determined only at 90 cm H2O of intravesical pressure, as 60 cm H2O of intravesical pressure is considered the cut-off for ISD. Therefore, future studies will test different intravesical pressures greater than 90 cm H2O and bladder volumes other than 100 mL, 200 mL, and 300 mL.
Increased BND, UTA, URA, and PUVA was presented at 200 mL of bladder volume when female patients with SUI increased the intra-abdominal pressure compared to that of 100 mL and 300 mL. It is recommended that a bladder volume of 200 mL should be adopted as the standard during the evaluation of female SUI, regardless of whether UDS or ultrasound is used.
The data that support the findings of this study are not openly available due to reasons of sensitivity and privacy protection and are available from the corresponding author upon reasonable request. Data is located in controlled access data storage at the second affiliated hospital of Guilin medical university and Shaoyang Central Hospital.
NX, LG, XY, HZ, XG and JW designed research; NX, XY, QT, GP, KW, HZ, and JW performed research; NX, LG, XY, QT, and HZ analyzed data; NX, XY, QT, GP, KW, HZ, and JW wrote the paper; NX, LG, and XG revised the paper. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study protocol was approved by the Medical Ethics Committee of the Second Affiliated Hospital of Guilin Medical University (EFY-GZR2022011) and Shaoyang Central Hospital (2022070). This study was in accord with the ethical principles of the Declaration of Helsinki and informed consents were obtained from all subjects.
We would like to express our gratitude to all those who helped us during the design and implementation of this study, and writing of this manuscript. Thanks to all the peer reviewers for their opinions and suggestions.
The work was supported by Hunan Provincial Natural Science Foundation of China (2024JJ7471), Guangxi Science and Technology Base and Talents Program (AD20159008), Planned projects of Guiding technological innovation of Hunan Province (2021SK52002), Guilin Science and Technology Development Program (20210218-2), Scientific Research Project of Guangxi Health Commission (S2020105), and Guangxi Clinical Key Specialty Construction (Cultivation) Projects sponsored by Guangxi Health Commission.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

