1 Department of Surgery, Oncology and Gastroenterology (DISCOG), University of Padova, 35124 Padova, Italy
2 Medical Oncology 2 Unit, Istituto Oncologico Veneto IOV-IRCCS, 35128 Padova, Italy
3 Department of Women's and Children's Health, University of Padua, 35128 Padua, Italy
Abstract
Background: One main issue to be considered in young patients diagnosed
with early breast cancer (BC) is the impact of oncological treatments on
fertility and future chances of conception. Current guidelines recommend a
comprehensive addressing of oncofertility as part of the management of
premenopausal BC patients, including counselling on available assisted
reproduction technologies and fertility preservation (FP) strategies. The
COVID-19 pandemic represented a potential hurdle to the integration of these
procedures into clinical practice. This study aims to describe the time-related
evolution in addressing oncofertility issues. Methods: This
retrospective mono-institutional observational study considered 206 patients who
received neoadjuvant chemotherapy, adjuvant chemotherapy (CT) or adjuvant
endocrine therapy (ET), diagnosed with breast cancer at the age of 40 or younger
in the years 2014–2015 and 2020–2021. Time-related evolution in addressing
oncofertility during oncological consultations and adoption of a fertility or
ovarian function preservation (OFP) method were analyzed comparing the two
different timeframes. Results: Comparing the two cohorts 2014–2015 and
2020–2021, we found a significant difference in the presence of fertility
discussion records (37.4% vs 57.9%, p
Keywords
- early breast cancer
- young breast cancer patients
- oncofertility
- fertility counseling
- fertility preservation
- ovarian function preservation
- pregnancy after breast cancer
- cancer survivorship
- COVID-19
Breast cancer (BC) is the most common malignancy worldwide, accounting for 2.26 million cases in 2020 [1]. Of these, at least 10% of newly diagnosed cases occur in women aged less than 45 years [2], and a relevant proportion of cases impact premenopausal women, representing about 55% of all BC diagnoses in low- and middle-income countries and about 25% of all cases in high-income countries [3].
In the last decades, breast cancer mortality has consistently declined, thanks to the advance in (neo)adjuvant systemic treatments [4]. However, both chemotherapy and endocrine treatments commonly prescribed for the disease may affect the reproductive function of young breast cancer patients [5, 6]. One main issue to be considered in this patient population is the possible impact of oncological treatments on their fertility and on future chances of conception [6].
Pregnancy after breast cancer has been discouraged for a long time, in the belief that the exposure to increased estrogen levels during gestation could promote reactivation and proliferation of dormant micrometastatic disease, hence favoring breast cancer relapses [7]. However, recent studies have shown not only that pregnancy after breast cancer is safe, but according to some reports BC survivors who give birth might even have a better prognosis than nulliparous BC survivors [8, 9, 10]. In a recent metanalysis by Lambertini et al. [9], who evaluated a population of 112,840 patients with prior breast cancer, BC survivors achieving a pregnancy had a better disease-free survival and overall survival compared to BC survivors without subsequent pregnancies.
Based on recent evidence, a comprehensive addressing of oncofertility issues is now recommended as part of the correct management of premenopausal BC patients, including counselling on available assisted reproduction technologies (ART) and fertility preservation (FP) strategies [6, 11]. These latter in particular comprise oocyte, ovarian tissue or embryos cryopreservation, while the administration of gonadotropin-releasing hormone (GnRH) analogues concomitantly to chemotherapy, which is recommended for all pre-menopausal women to avoid primary ovarian failure (POF) and its symptoms, is not considered as an alternative to cryopreservation techniques [6, 12].
The COVID-19 pandemic represented a potential hurdle to the integration of this approach into clinical practice, together with straining healthcare systems in general, and impacting on breast cancer screening, early-diagnosis and treatment [13]. In the COVID-19 era a reduction in FP and ART procedures was registered in some countries, possibly relating to both hospitals’ issues—such as the reorganization of services, the reduction of multidisciplinary consultations, the shortage of commodities—and patients’ concerns, such as the desire to limit hospital visits to the minimum in the fear of getting infected, or a loss of interest in pursuing parenting desires [14].
In this context, a better picture of the current state of oncofertility issues management in oncology clinical practice could be gained through the evaluation of real-world data.
This retrospective observational mono-institutional study includes patients who
were referred to Istituto Oncologico Veneto (Padova, Italy), being diagnosed at
40 years or younger with non-metastatic breast cancer, who underwent
(neo)adjuvant treatments. The aim of the study is to describe the time-related
evolution in addressing oncofertility issues during oncological consultations,
and the evolution of the adoption of FP/ovarian function preservation (OFP)
techniques, as reflected by medical charts, by comparing the two different
timeframes 2014–2015 and 2020–2021. Data were collected in a previously
scheduled database and information about age, parity, treatments,
clinicopathologic tumor features, medical records about fertility issues
discussion, and the use of FP and/or OFP techniques were extracted. The primary
objective of this study is to assess the difference in the rate of a documented
discussion regarding oncofertility issues in medical charts or adoption of a
FP/OFP method between two cohorts of patients diagnosed in 2014–2015 and
2020–2021, respectively. The secondary end-point was to investigate the impact
of patient-related characteristics (such as age
The study considered 206 patients who received neoadjuvant chemotherapy, adjuvant chemotherapy (CT) or adjuvant endocrine therapy (ET), diagnosed with breast cancer at the age of 40 or younger in the years 2014–2015 (n = 99, 48.1% of total patients) and 2020–2021 (n = 107, 51.9% of total patients). For 68.4% of patients overall, the treating clinician recorded in the medical charts either having discussed fertility issues, or the adoption of an ovarian function/fertility preservation (OFP/FP) technique, or both (Table 1). Since embryos preservation is not allowed in Italy at the current time and ovarian tissue is still an experimental technique practiced in few dedicated centers, in our analysis fertility preservation consisted exclusively in oocyte cryopreservation, representing the best-established technique in this setting. Ovarian function preservation consisted in GnRH analogue (GnRHa) administration during chemotherapy. Even though this was not a standard procedure in 2014–2015, several studies dating back even to 2003 had already suggested the potential benefit of GnRH analogues for the purpose of ovarian function preservation [15].
| Study population | ||||
|---|---|---|---|---|
| N total = 206 | ||||
| n | % | |||
| Median age at diagnosis (range) | 37 (23–40) | |||
| Age | 79 | 38.3 | ||
| 127 | 61.7 | |||
| Parity | no | 72 | 35.0 | |
| yes | 107 | 51.9 | ||
| HR status | Negative (ER and PgR |
59 | 28.6 | |
| Positive (ER and/or PgR |
147 | 71.4 | ||
| Chemotherapy | no | 31 | 15.0 | |
| yes | 175 | 85.0 | ||
| Endocrine therapy | no | 60 | 29.1 | |
| yes | 146 | 70.9 | ||
| Documented fertility discussion and/or fertility/ovarian function preservation technique application | no | 65 | 31.6 | |
| yes | 141 | 68.4 | ||
| Documented fertility discussion | 99 | 48.1 | ||
| Fertility/ovarian function preservation technique applied | 138 | 67.0 | ||
| Ovarian function preservation only | 112 | 54.4 | ||
| Fertility preservation | 26 | 12.6 | ||
| None/not reported | 68 | 33.0 | ||
Summary of the characteristics of the overall study population: demographic and tumour characteristics, documented fertility discussion and/or OFP/FP techniques application. HR, hormone receptor; ER, estrogen receptor; PgR, progesteron receptor. “Ovarian function preservation only” refers to the exclusive use of GnRH analogue during chemotherapy administration.
Despite there was no difference in age and in the type of anticancer systemic
treatment received in the two cohorts (Table 2), we found a significant
difference in the presence of fertility issues discussion records (37.4% of
patients in the 2014–2015 cohort vs 57.9% in the 2020–2021 cohort,
p
| Cohort | Cohort | |||||
|---|---|---|---|---|---|---|
| 2014–2015 | 2020–2021 | |||||
| N total = 99 | N total = 107 | |||||
| n | % | n | % | |||
| Median age at diagnosis (range) | 37 (23–40) | 37 (24–40) | ||||
| Chemotherapy | no | 14 | 14.1 | 17 | 15.9 | |
| yes | 85 | 85.9 | 90 | 84.1 | ||
| Endocrine therapy | no | 32 | 32.3 | 28 | 26.2 | |
| yes | 67 | 67.7 | 79 | 73.8 | ||
| Documented fertility discussion and/or fertility/ovarian function preservation technique application | no | 44 | 44.4 | 21 | 19.6 | |
| yes | 55 | 55.6 | 86 | 80.4 | ||
| Documented fertility discussion | 37 | 37.4 | 62 | 57.9 | ||
| Fertility/ovarian function preservation technique applied | 54 | 54.5 | 84 | 78.5 | ||
| Ovarian function preservation only | 49 | 49.5 | 63 | 58.9 | ||
| Fertility preservation (with or without GnRH analogue) | 5 | 5.1 | 21 | 19.6 | ||
| None/not reported | 45 | 45.5 | 23 | 21.5 | ||
Summary of the characteristics of the two cohorts identified in the study population based on the time of breast cancer diagnosis (2014–2015 vs 2020–2021): documented fertility discussion and/or OFP/FP techniques application. GnRH, gonadotropin-releasing hormone. “Ovarian function preservation only” refers to the exclusive use of GnRH analogue during chemotherapy administration.
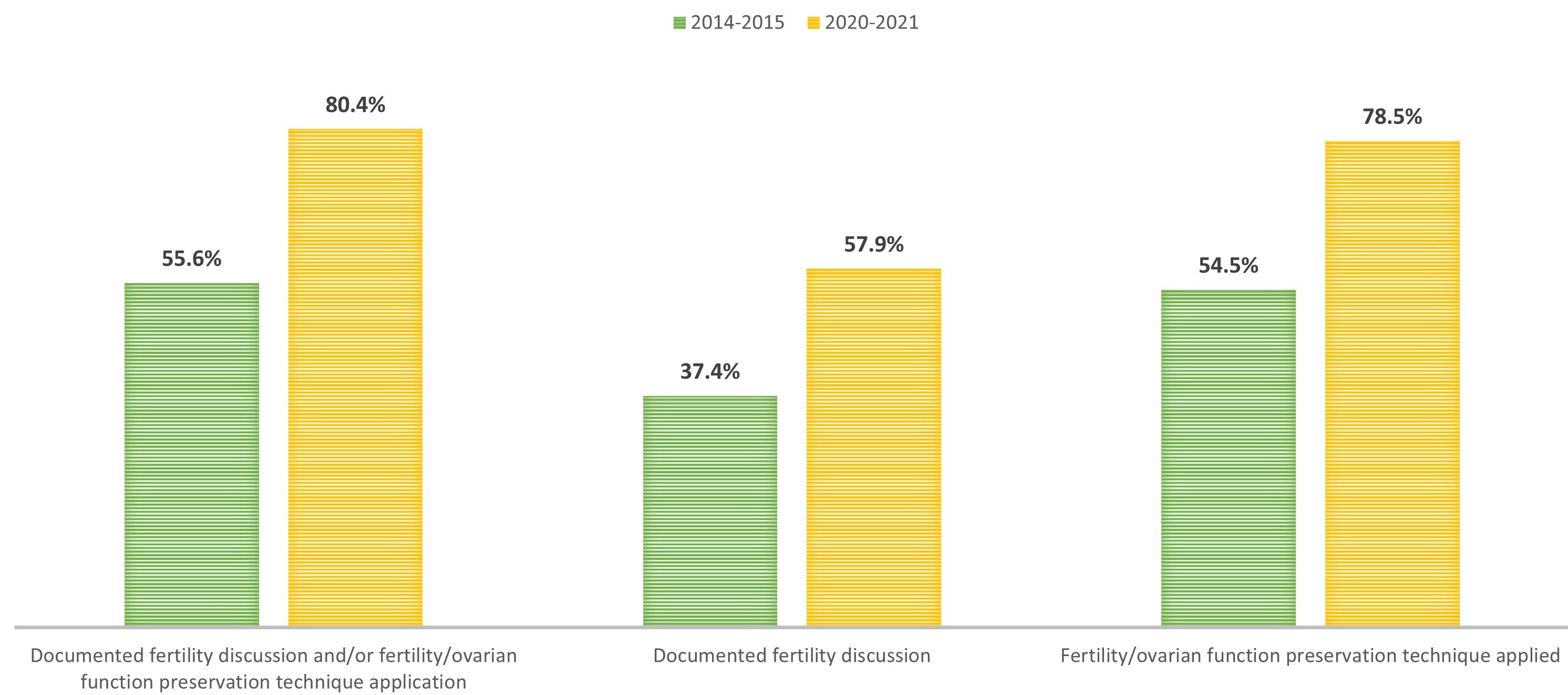 Fig. 1.
Fig. 1.Documented fertility discussion and/or fertility/ovarian function preservation technique application based on time of breast cancer diagnosis. Comparison between the two cohorts of patients who received the diagnosis of BC in the years 2014–2015 or 2020–2021, with respect to the rate of presence of a documented discussion of fertility issues in medical dossiers or of application of a technique of ovarian function/fertility preservation, and with respect to each of the two interventions (oncofertility discussion or OFP/FP; columns from left to right).
We then analyzed the rate of OFP and FP separately in the two time cohorts, as shown in Fig. 2. When the analysis was restricted to the 175 patients undergoing chemotherapy, OFP only was more frequent in 2020–2021 as compared to 2014–2015 (57.6% of patients in 2014–2015 cohort vs 70% in 2020–2021, p = 0.03).
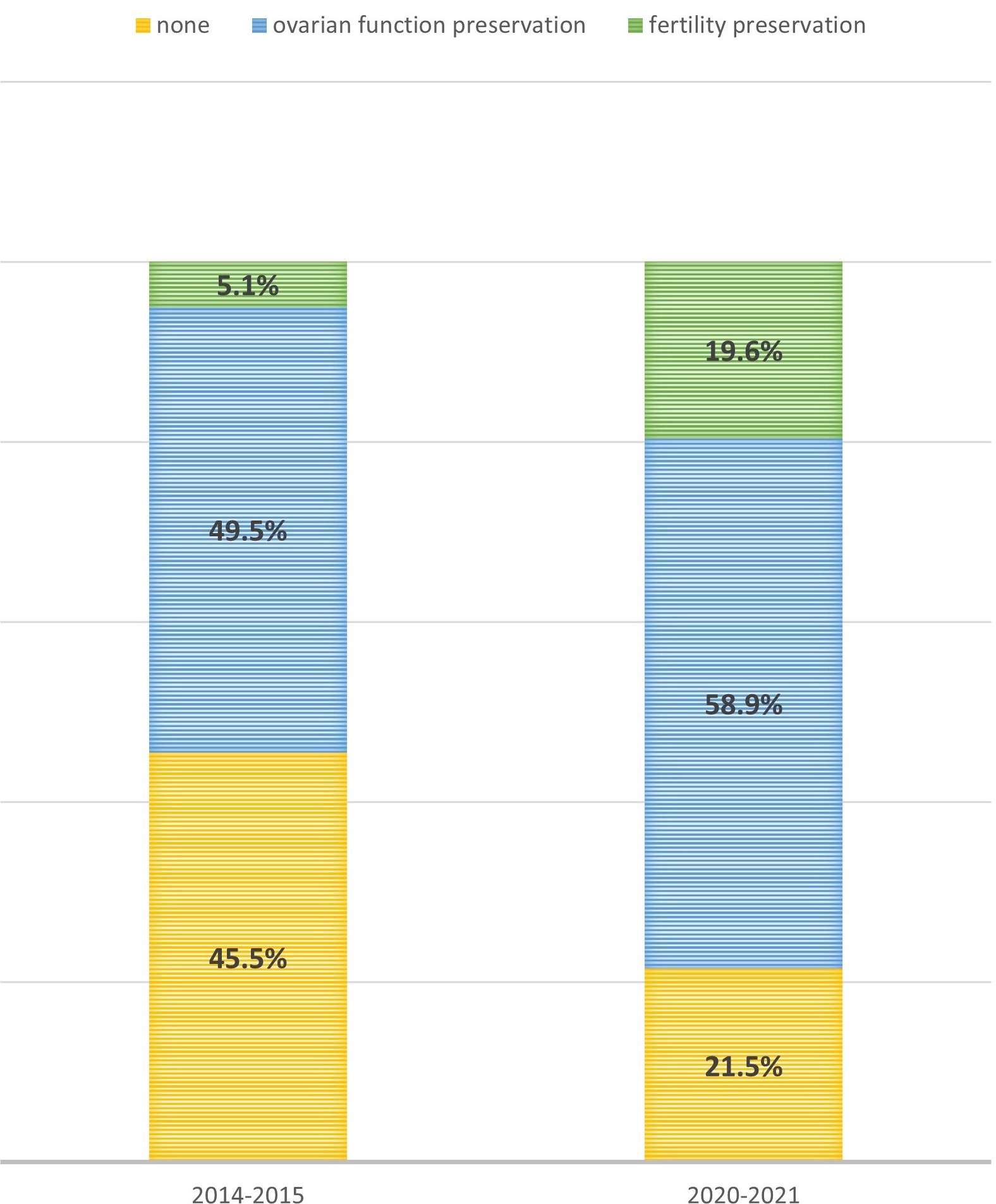 Fig. 2.
Fig. 2.Fertility/ovarian function preservation techniques application based on time of breast cancer diagnosis. Comparison between the two cohorts of patients who received the diagnosis of BC in the years 2014–2015 or 2020–2021, with respect to the proportion of patients who underwent a full fertility preservation procedure (green), only ovarian function preservation in patients undergoing chemotherapy (blue), or neither (yellow).
Similarly, we observed a significant difference in the rate of FP techniques
(
We then investigated the possible influence of age at diagnosis and parity on
the rate of discussions on fertility issues and on the use of OFP/FP techniques.
In our study population, age resulted to influence clinicians’ approach towards
counseling and/or OFP/FP strategies (87.3% of
| N = 79 | N = 127 | ||||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Documented fertility discussion and/or fertility/ovarian function preservation technique application | 69 | 87.3 | 72 | 56.7 | |
| Documented fertility discussion | 54 | 68.4 | 45 | 35.4 | |
| Fertility/ovarian function preservation technique applied | 66 | 83.5 | 72 | 56.7 | |
| Ovarian function preservation only | 49 | 62.0 | 63 | 49.6 | |
| Fertility preservation (with or without GnRH analogue) | 17 | 21.5 | 9 | 7.1 | |
| None/not reported | 13 | 16.5 | 55 | 43.3 | |
Comparison of the rate of documented fertility discussion and/or of ovarian function/fertility preservation technique application between patients aged 35 years or less and patients older than 35 at the time of the diagnosis of breast cancer. GnRH, gonadotropin-releasing hormone. “Ovarian function preservation only” refers to the exclusive use of GnRH analogue during chemotherapy administration.
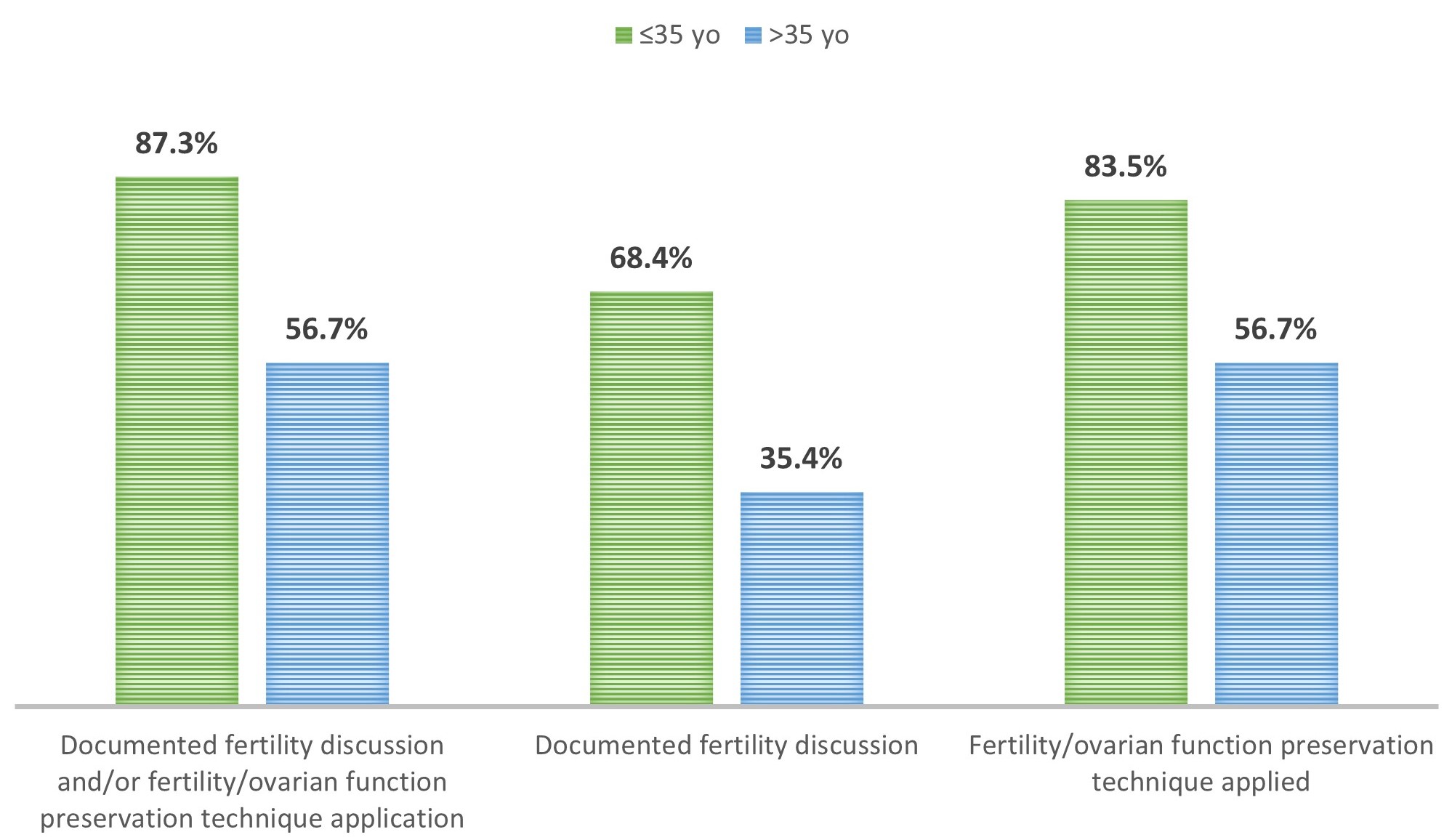 Fig. 3.
Fig. 3.Documented fertility discussion and/or fertility/ovarian function preservation technique application based on age at the time of breast cancer diagnosis. Comparison between the two cohorts of patients who received the diagnosis of BC at the age of 35 or less or beyond the age of 35, with respect to the rate of documented discussion of fertility issues in medical dossiers or of ovarian function/fertility preservation technique application, and with respect to each of the two interventions (oncofertility discussion or OFP/FP; columns from left to right).
In detail, if patients’ age turned out to not significantly influence the rate
of GnRH analogues prescription during chemotherapy (65.3% of patients
 Fig. 4.
Fig. 4.Fertility/ovarian function preservation techniques application based on age at the time of breast cancer diagnosis. Comparison between the two cohorts of patients who received the diagnosis of BC at the age of 35 or less or beyond the age of 35, with respect to the proportion of patients who underwent a full fertility preservation procedure (green), only ovarian function preservation in patients undergoing chemotherapy (blue), or neither (yellow).
The influence of age was confirmed in both 2014–2015 and 2020–2021 cohorts,
except for the rate of OFP/FP techniques application. In fact, in the 2020–2021
cohort, age resulted less influential in the choice of using an OFP/FP strategy
(prescribed in 87.0% of
| 2014–2015 | 2020–2021 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| p-value | p-value | |||||||||
| N = 33 | N = 66 | N = 46 | N = 61 | |||||||
| n | % | n | % | n | % | n | % | |||
| Documented fertility discussion and/or fertility/ovarian function preservation technique application | 27 | 81.8% | 28 | 42.4% | p |
42 | 91.3% | 44 | 72.1% | p = 0.01 |
| Documented fertility discussion | 19 | 57.6% | 18 | 27.3% | p |
35 | 76.1% | 27 | 44.3% | p |
| Fertility/ovarian function preservation technique applied | 26 | 78.8% | 28 | 42.4% | p |
40 | 87.0% | 44 | 72.1% | p = 0.18 |
Rate of documented discussion of fertility issues in medical dossiers or ovarian function/fertility preservation technique application preservation in patients aged 35 years or less and patients older than 35 at the time of the diagnosis of breast cancer, split into two cohorts according to the year of diagnosis (2014–2015 vs 2020–2021).
We retrieved information regarding parity before BC diagnosis for 179 patients.
In this group, we recorded a higher rate of documented fertility discussion
and/or OFP/FP techniques application in patients who had not had children before
BC diagnosis (80.6% of patients without vs 64.5% of patients with
children, p = 0.02). This significant difference was confirmed for both
fertility discussion documentation (69.4% of patients without vs 36.4%
of patients with children, p
| No previous children | Previous children | ||||
|---|---|---|---|---|---|
| N = 72 | N = 107 | ||||
| n | % | n | % | ||
| Documented fertility discussion and/or fertility/ovarian function preservation technique application | 58 | 80.6 | 69 | 64.5 | |
| Documented fertility discussion | 50 | 69.4 | 39 | 36.4 | |
| Fertility/ovarian function preservation technique applied | 57 | 79.2 | 67 | 62.6 | |
| Ovarian function preservation only | 33 | 45.8 | 67 | 62.6 | |
| Fertility preservation (with or without GnRH analogue) | 24 | 33.3 | 0 | 0.0 | |
| None/ not reported | 15 | 20.8 | 40 | 37.4 | |
Rate of documented discussion of fertility issues in medical dossiers and/or of ovarian function/fertility preservation technique application in patients who had already gave birth at least once before the diagnosis of breast cancer and in patients nulliparous at diagnosis, respectively. “Ovarian function preservation only” refers to the exclusive use of GnRH analogue during chemotherapy administration.
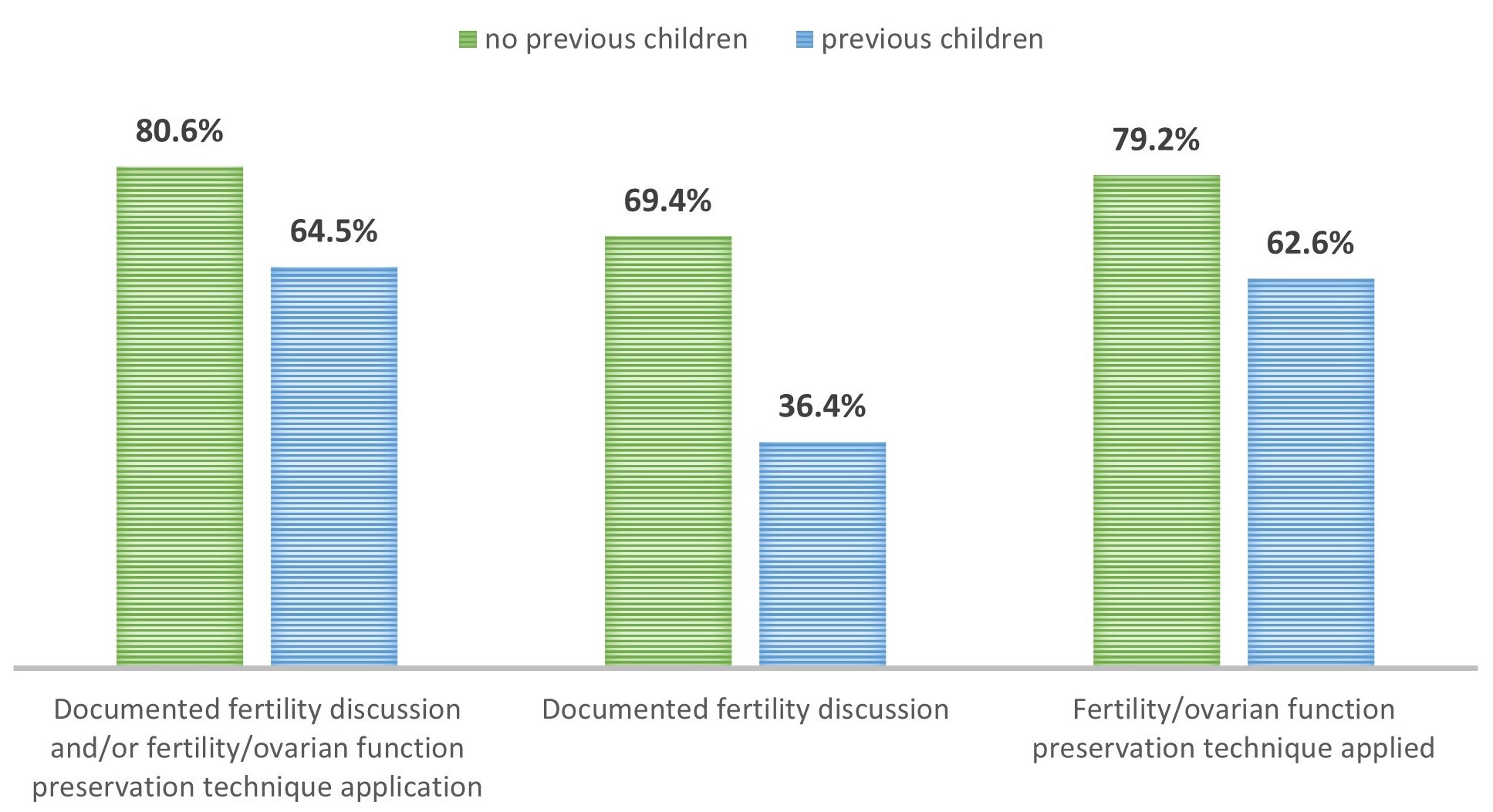 Fig. 5.
Fig. 5.Documented fertility discussion and/or fertility/ovarian function preservation technique application by parity. Comparison between the two cohorts of patients who received the diagnosis of BC while nulliparous or after having already gave birth, respectively, with respect to the rate of documented discussion of fertility issues in medical dossiers or of application of a technique of ovarian function/fertility preservation, and with respect to each of the two interventions (oncofertility discussion or OFP/FP; columns from left to right).
Parity had a significant influence on the exclusive use of GnRH analogues during
chemotherapy, with a significant difference observed in the rate of OFP (55.9%
of patients without vs 70.5% of patients with children, p =
0.03), and in the use of oocyte cryopreservation in patients undergoing
(neo)adjuvant treatments (33.3% of patients without vs no patients with
children, p
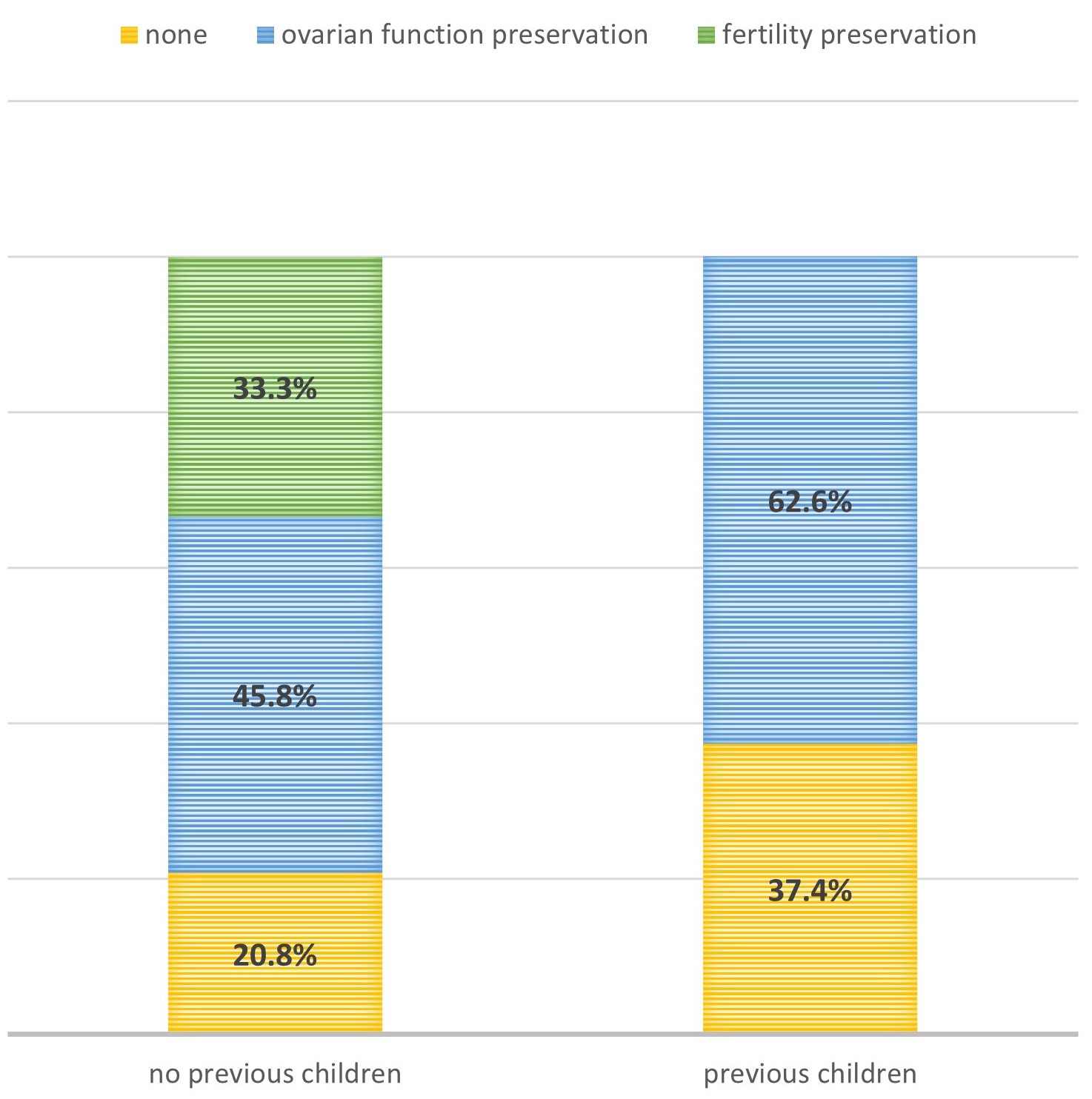 Fig. 6.
Fig. 6.Fertility/ovarian function preservation technique applied by parity. Comparison between the two cohorts of patients who received the diagnosis of BC while nulliparous or after having already gave birth, respectively, with respect to the proportion of patients who underwent a full fertility preservation procedure (green), only ovarian function preservation in patients undergoing chemotherapy (blue), or neither (yellow).
Interestingly, when considering each of the two cohorts separately, parity had a more limited impact in 2020–2021. Indeed, in the most recent timeframe, parity did not influence the application of an OFP/FP strategy (80.4% of patients without vs 78.3% of patients with children, p = 0.93) (Table 6).
| 2014–2015 | 2020–2021 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No previous children | Previous children | p-value | No previous children | Previous children | p-value | |||||
| N = 26 | N = 47 | N = 46 | N = 60 | |||||||
| n | % | n | % | n | % | n | % | |||
| Documented fertility discussion and/or fertility/ovarian function preservation technique application | 20 | 76.9 | 21 | 44.7 | p |
38 | 82.6 | 48 | 80.0 | p = 0.73 |
| Documented fertility discussion | 17 | 65.4 | 10 | 21.3 | p |
33 | 71.7 | 29 | 48.3 | p = 0.02 |
| Fertility/ovarian function preservation technique applied | 20 | 76.9 | 20 | 43.5 | p |
37 | 80.4 | 47 | 78.3 | p = 0.93 |
Rate of documented discussion of fertility issues in medical dossiers and/or of ovarian function/fertility preservation technique application in patients with or without previous offspring at the time of the diagnosis of breast cancer, split into two cohorts according to the year of diagnosis (2014–2015 vs 2020–2021).
Finally, we investigated whether the setting in which patients received chemotherapy (neoadjuvant vs adjuvant) could influence the use of OFP/FP or the strategy chosen by clinicians. The setting of CT administration had no significant influence on the use of OFP/FP techniques (74.2% of patients receiving neoadjuvant vs 78.2% of patients receiving adjuvant treatment, p = 0.88), nor on the strategy chosen (oocyte cryopreservation used in 9.3% of patients receiving neoadjuvant vs 15.4% of patients receiving adjuvant CT, p = 0.25).
In none of the evaluated medical records issues related to the COVID-19 pandemic were mentioned as a factor impacting patients’ and clinicians’ shared decisions regarding OFP/FP strategies.
Oncofertility counseling in young patients is nowadays a well-established clinical practice, as recommended with agreement by the main oncology guidelines [6, 16], which have themselves evolved following the expanding evidence that pregnancy after breast cancer does not increase the risk of relapse [8, 9]. This might explain our results, which show a rise in clinicians’ sensitivity to the topic over time, with a significantly higher rate of well documented counseling in 2020–2021 with respect to 2014–2015, also translating into a significant increase in OFP/FP application. Our data are cohesive with literature data such as results from the PREgnancy and FERtility (PREFER) study [17], even though we observed lower rates of OFP/FP application than the PREFER authors did (94.9% vs 78.5%), probably due to the different study designs (being PREFER a prospective trial with a selected population, while we report a retrospective analysis of real-world data).
The data we present show how the application of oocyte cryopreservation has significantly increased over time, not being considered anymore as a prerogative of younger patients, but rather being now applied in an unbiased way even in older patient groups. These results find explanation on multiple bases. First, there is conflicting evidence on the role of GnRH-analogues for fertility preservation [16]. In this regard, guidelines have been updated over time, with major changes brought about by the American Society of Clinical Oncology (ASCO) guidelines update in 2018, discouraging the prescription of ovarian function suppression alone for the purpose of FP. This different approach is reflected by our results, which show an increased application of established FP techniques over time, such as oocyte cryopreservation. Secondly, the steady increase in the median age at first childbirth [18] might explain our observation of a progressive increase in physicians’ care in addressing oncofertility issues in patients older than 35. Of note, since for hormone-receptor positive BC patients it is safer to undergo adjuvant hormone therapy for at least two years before planning a pregnancy [19], it is important to offer FP counseling even to those patients who may not receive gonadotoxic chemotherapy, but who could still experience infertility due to age-related ovarian function insufficiency intervening meanwhile. Consistently, in our analysis 5 patients from the 2020–2021 cohort underwent oocyte cryopreservation before starting an adjuvant treatment of exclusively endocrine type; indeed, these patients were all 35 or older.
Our study also describes a significantly rising trend of FP discussion in patients who already had children, showing an encouraging higher awareness of clinicians in offering counseling without any bias, in keeping with the most recent guidelines issued by ASCO, by the European Society of Medical Oncology (ESMO), as well as by its Italian counterpart Associazione Italiana di Oncologia Medica (AIOM) [6, 16, 20].
Moreover, data about cryopreservation refusals (3 patients in the 2014–2015 cohort and 6 patients in the 2020–2021 cohort) are still relevant, denoting how, beyond guidelines recommendations, the ultimate correct therapeutic path is based on sharing a mutual clinician-patient decision that must include women’s concerns and desires. Considering how some refusals were due to the fear of delaying oncologic treatments onset, in the future it will be fundamental to corroborate recent evidence from the PREFER trial, showing how oocyte preservation doesn’t correlate with worse outcomes in terms of relapse and survival rates [16].
Finally, we evaluated the potential impact of the COVID-19 pandemic on the approach to oncofertility. Despite the hurdles imposed by the pandemic on health systems, and the concerns related to a possible in-hospital spread of the virus, our analysis doesn’t seem to show any negative influence of the COVID-19 pandemic on the application of FP processes. This finding suggests a fair response of healthcare systems to the new difficulties, and strengthens the evidence of a high awareness of both clinicians and patients to this important topic. Being oncofertility currently recognized as a full-fledged essential part of clinical practice in oncology, it is of paramount importance that Oncology Departments work together with the other involved units to build dedicated FP services, with the aim of providing and coordinating dedicated programs for these patients, in the context of a sound multidisciplinary approach [11].
This study on real-world data shows how fertility preservation issues of early breast cancer patients are addressed in clinical practice at a large Italian Cancer Center, and demonstrates a progressive evolution in the way clinicians approach them. Our data suggest that oncofertility has gained a greater relevance in the practice of oncology across the last eight years, with more breast cancer patients receiving a dedicated counseling, and in a progressively less biased way with respect to age or parity at diagnosis. No significant negative impact of the COVID-19 pandemic on fertility preservation techniques application in this setting was observed.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
MVD, VG, RT, CB, OA and ACC designed the research study. CB, ACC, LM, AA, CS, TG, GF, EDL, CAG, EM, CF, GMV, performed the research. CB and MVD analyzed the data. CB, OA and ACC wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
In the present study patients’ data were collected after approval by the respective Institutional Review Boards and in accordance with the Declaration of Helsinki (approval number: 2023-08 with protocol ID: 21516). According to the recently updated Italian Law regarding observational studies, the informed consent is no longer needed for retrospective data collections, hence no informed consent was obtained from patients for this study.
The authors wish to acknowledge the contribution of all the Colleagues of the Oncologia 2 Unit of Istituto Oncologico Veneto in Padova and thank patients who accepted to take part in the study.
This project was supported by the Veneto Institute of Oncology IOV-IRCCS (Grant: “5×1000 anno di riferimento 2015-Genomica dei tumori e immunoterapia nell’era dei big data, fase 2” to VG).
VG reports personal fees from Amgen, Exact Science, Eli Lilly, Gilead, MSD, Sanofi, Pfizer, Novartis, Merk Serono, GSK, outside the submitted work. MVD reports personal fees from Eli Lilly, Roche, Gilead, Daiichi-Sankyo, MSD, Exact Sciences, Novartis, Pfizer, Seagen, outside the submitted work. The other authors declare no conflict of interest.
Loris Marin is serving as one of the Guest editors of this journal, and Alessandra Andrisani is serving as one of the Editorial Board members and Guest editors of this journal We declare that Loris Marin and Alessandra Andrisani had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to Ferdinando Antonio Gulino.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.






