1 Department of Women’s and Children’s Health, University of Padua, 35100 Padua, Italy
2 Department of Surgical, Microsurgical and Medical Sciences, Gynecologic and Obstetric Clinic, University of Sassari, 07100 Sassari, Italy
3 Department of Health Promotion, Mother and Child Care, Internal Medicine and Medical Specialties (PROMISE), University of Palermo, 90134 Palermo, Italy
4 Clinica Medica 3, Department of Medicine-DIMED, University Hospital of Padova, 35100 Padova, Italy
Academic Editor: Ariel Weissman
Abstract
Objective: Many women worldwide are diagnosed with cancer in prepubertal, postpubertal and childbearing age. Oncological treatments can compromise future fertility through different mechanisms mainly depending on the type of treatment and the age of the patient. International societies recommend that cancer patients should receive information regarding the effects of oncological treatments on their reproductive health and cancer survivors should not be discouraged from becoming pregnant. About a quarter of these patients still do not receive an adequate counselling and young cancer survivors may face several barriers to conceiving a pregnancy due to the concerns from gynaecologists and oncologists. This review aims to investigate the infertility risk for female cancer patients who undergo oncological treatments and to provide an overview of actual and future fertility preservation possibilities for female cancer patients. Mechanism: We examined the current and future possibilities of preserving fertility for women with cancer in the available literature. Findings in brief: Different fertility preservation techniques have been developed in order to ensure the possibility for cancer survivors to complete their family planning after cancer. Oocyte/embryo freezing and ovarian tissue cryopreservation are the established choices, but the research is still going on to increase the success rate of these techniques and to develop other techniques to overcome actual limitations. Patients with a systemic oncological disease such as leukaemia could particularly benefit from the new experimental techniques which involve the creation of an artificial ovary or the in vitro growth of follicles or even the obtaining of mature oocytes from stem cells. All these techniques would allow the achievement of pregnancy without the risk of reintroducing malignant cells within autologous cryopreserved ovarian tissue transplantation. Regarding the concerns over pregnancy in cancer survivors, research is rapidly advancing and reassuring data are increasing. Conclusions: The rate of utilisation of gametes, embryos or ovarian tissue previously stored for fertility preservation is still low and the motivations can be various. Further data are needed in order to reassure both women and oncologists about the safety of pregnancy in cancer survivors and in order to increase the rate of women experiencing pregnancy after cancer.
Keywords
- cancer
- oncofertility
- fertility preservation
- pregnancy after cancer
In 2020 almost 2 million women were diagnosed with cancer in childbearing age and almost 9000 in prepubertal age worldwide [1]. Among prepubertal females the malignancies with the highest incidence are lymphoproliferative diseases whereas breast cancer is the most common cancer in women of childbearing age [1]. In recent decades, the early diagnosis and the advancements of oncological treatments have allowed a higher rate of survival after cancer [2]. At the same time, the age of first pregnancy for women has progressively moved forward for social and cultural reasons [3]. This has meant that many women have not yet completed or even started their reproductive project when they are diagnosed with cancer. Oncological therapies such as surgery [4, 5], radiotherapy [6] and pharmacological treatments [7, 8, 9], can have a negative effect on the ovarian reserve with different mechanisms and therefore they can compromise fertility at different levels. For this reason, interest in oncofertility has exponentially increased in recent decades, in order to ensure these women a good quality of life and the possibility of conceiving. All the international societies of reproductive medicine and oncology recommend that cancer patients of childbearing age with a good prognosis quod vitam are offered a consultation with a reproductive medicine specialist that can explain them the possible impact of different cancer approaches over fertility and that can also suggest them the most suitable methods for preserving fertility [10, 11, 12]. The elective fertility preservation techniques are the cryopreservation of embryos/oocytes and the cryopreservation and reimplantation of ovarian tissue, which is no longer considered an experimental technique by the American Society of Reproductive Medicine since 2019 [11]. The latter method is the only option for prepubescent patients and for patients who need to start cancer therapy quickly. In addition, fertility sparing surgery is envisaged when possible and ovariopexy is recommended in the case of pelvic radiation therapy [13]. If it is not possible to undergo any of the aforementioned elective fertility preservation techniques, the use of the gonadotropin-releasing hormone agonist (GnRHa) for the preservation of ovarian function is recommended [10].
The purpose of this review is to summarise the state of the art of oncofertility. Particular attention will be paid to future therapeutic possibilities, to fertility preservation in prepubertal patients and to pregnancies in cancer survivors.
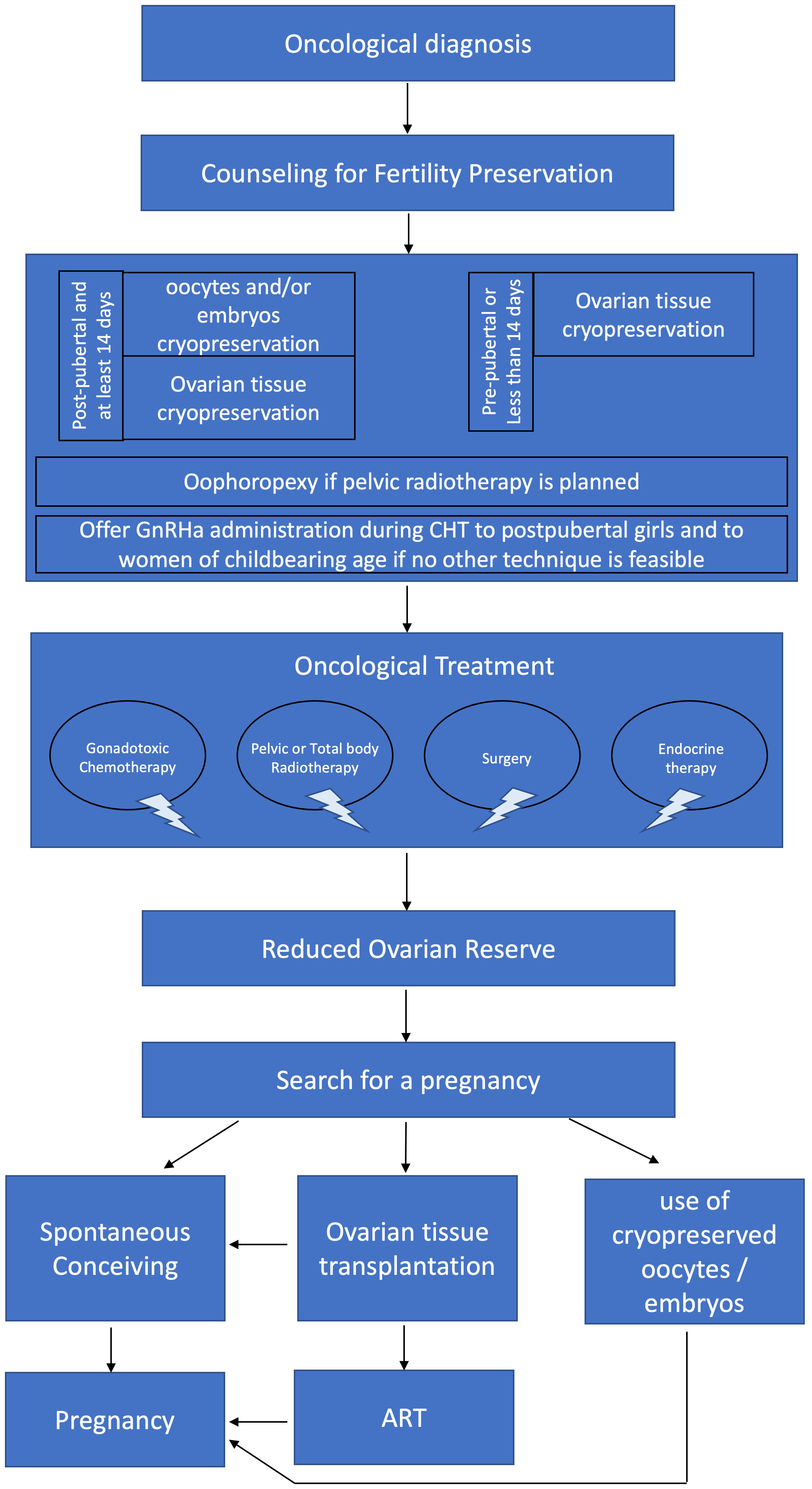
Oncological treatments can damage reproductive organs and affect the ability to conceive. Because of this, it is of primary importance for cancer patients to receive appropriate information about the effects of the oncological treatments that they are going to receive over their future fertility [10, 11, 12] (Fig. 1). Unfortunately, literature confirms that fertility preservation counselling is often inadequate [14]. In a recent study, only 74% of the patients recalled having discussed fertility preservation before starting cancer treatments [15]. Among the patients who did not remember the counselling over fertility preservation, 83% affirmed that they would have liked to receive information about fertility preservation [15, 16]. In a recent review, high prevalence of poor mental health was reported in cancer survivors and reproductive concerns in cancer survivors of fertile age were linked to the development of mental health disorders and to psychological distress [17]. These patients need psychological support from the diagnosis through to survivorship and an adequate oncofertility counselling might help to overcome their reproductive concerns.
 Fig. 1.
Fig. 1.Flowchart for fertility preservation in cancer patient. GnRHa, gonadotropin-releasing hormone agonist; CHT, chemotherapy; ART, assisted reproductive technologies.
In an observational retrospective study, the application of a standard oncofertility care plan was evaluated in a national paediatric care centre in Netherlands [18]. The aim of this study was to identify all the new patients diagnosed with cancer, to assess gonadal damage risks, to inform the patients on their risks and to preserve their fertility if possible. As a result, 88% of patients were triaged for fertility preservation and implementing oncofertility care did not cause any delays in starting cancer treatments [18]. It is therefore important to provide information to cancer patients about the effects of cancer therapies over their reproductive health and their fertility, as stated in international guidelines [10, 11, 12]. It is also mandatory to explain to these patients the impact of the oncological treatments that they are going to receive on their fertility according to their age, their history, their ovarian reserve and to explain to them the available fertility preservation options.
Oncological women should be referred for counselling for fertility preservation in order to evaluate the impact of gonadotoxic treatments on fertility and to establish the best fertility preservation technique.
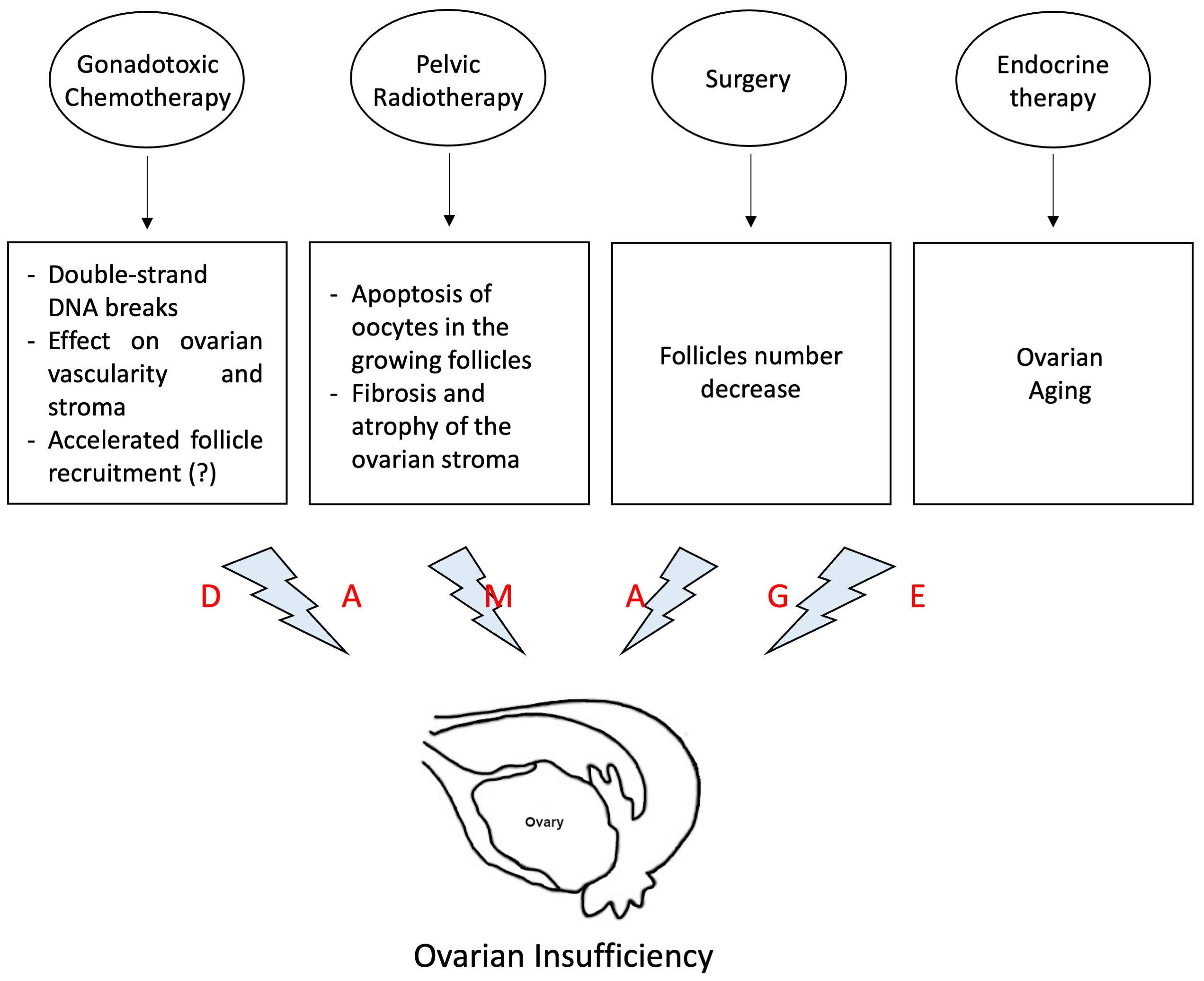
Different kinds of treatments can be used as cancer therapy, such as surgery [4, 5], chemotherapy [7, 8], radiotherapy [6] and endocrine treatment [9]. These treatments, that can be used alone or in different combinations, can lead to infertility mainly through the reduction of the ovarian reserve due to the gonadal damages caused by different mechanisms (Fig. 2).
 Fig. 2.
Fig. 2.Mechanisms of ovarian damage of different oncological treatments. This figure illustrates the different mechanisms of action of oncological treatments that can cause direct or indirect damage to ovarian function.
Surgery can cause infertility when the hypothalamus or the pituitary gland are involved, leading to hypogonadotropic hypogonadism [19]. Surgery can also cause infertility when it involves directly the uterus and the ovaries [4, 5]. Ovarian surgery in cancer patients can lead to a reduction of the ovarian reserve. In fact, ovarian resection, multiple ovarian biopsies [20] or the bilateral ovariectomy can bring to iatrogenic menopause. Uterine surgery can also lead to infertility or to pregnancy issues [4]. Women that underwent hysterectomy need for a gestation carrier to carry on the pregnancy and women who have undergone trachelectomy may have an increased risk of miscarriage and preterm birth and they need a prophylactic cerclage to reduce these risks [21] (Fig. 2).
With regard to chemotherapy treatment, the gonadal damage varies according to
the type of chemotherapy used, the dose of the drug and the age of the woman [10, 22]. Alkylating agents (particularly cyclophosphamide) cause permanent amenorrhea
in
Women undergoing haematopoietic stem cell transplantation have an
age-independent high risk of premature ovarian insufficiency (POI) due to
conditioning chemotherapy with cyclophosphamide and (due to) high-dose total body
irradiation [24, 25]. The risk of permanent amenorrhea is low (
The effects of radiotherapy on the ovarian reserve depend on radiation dose, on patient’s age (prepubertal, postpubertal, adulthood) and whether radiotherapy involves ovaries in its action field [30]. Oocytes in the growing follicles appear to be more radiosensitive than those at a more immature stage, however the most radiosensitive cells in the ovary are those of the granulosa, necessary in folliculogenesis [31]. Ovarian stroma and vascularization are also affected by radiotherapy which causes fibrosis and atrophy of the ovary [32] (Fig. 2). Finally, pelvic radiotherapy can affect fertility also due to uterine radiation damage, especially in prepubertal girls, with defective uterine and endometrial development and consequent greater risk of negative pregnancy outcomes such as higher incidence of abortion, placentation defects, intrauterine fetal growth restriction and preterm birth [6, 32]. It has been theorised that exposure to abdominal irradiation increases myometrial fibrosis and negatively affects uterine vascularization restricting the ability to carry the gestation until term [33, 34].
Endocrine therapy is an oncological treatment in hormone sensitive cancers and it has an indirect negative effect on ovarian reserve acting through ovarian ageing [35]. In fact, this kind of therapy is usually used as adjuvant therapy for 5 or 10 years and during this period the pregnancy must be avoided. It is well known that both quantity and quality of oocytes are affected by age and that fertility decreases quickly after 35 years old [35] (Fig. 2). The “POSITIVE study” (Pregnancy Outcome and Safety of Interrupting Therapy for women with endocrine respons IVE breast cancer) is an ongoing trial (NCT02308085) that is investigating the impact of temporary adjuvant endocrine therapy interruption in order to allow pregnancy and in order to overcome the issue of ovarian ageing due to endocrine therapy. Women enrolled in this study are young hormonal receptor positive breast cancer patients who wish to interrupt therapy and achieve pregnancy. These women have up to 2 years therapy-free in order to become pregnant, deliver and breastfeed and then they should resume endocrine therapy to complete the planned duration. It is recommended to have completed 18–30 months of the adjuvant therapy and 3 months of wash-out between treatment interruption and pregnancy attempt [35]. Final data collection date for primary outcome measure is planned for December 2022 (https://clinicaltrials.gov/ct2/show/NCT02308085).
Different techniques for fertility preservation have been developed according to the oncological disease and the related treatment [12]. In gynecologic cancers, fertility preservation strategies include fertility-sparing surgery and assisted reproductive technologies (ART). The best treatment option is a personalised multidisciplinary strategy. It should be based on the type and on the stage of cancer, on the available time before treatment start, on age, on ovarian reserve and on partner status (Fig. 1).
Patients with early-stage cervical cancer can undergo uterine preserving surgery in selected cases: conization can be considered for FIGO stage IA1; while radical abdominal, vaginal, or laparoscopic trachelectomy with pelvic lymphadenectomy can be considered for stage IA2–IB1 and neoadjuvant chemotherapy combined with conservative surgery for stage IB1 [4]. If pelvic radiotherapy is needed, ovarian transposition to an upper abdominal location far from the irradiation field and/or high-precision MRI-guided brachytherapy can be considered [36, 37].
The uterus-preserving strategies for women with endometrial cancer are limited. The only possibility is for women with well differentiated endometrial adenocarcinoma, who can undergo hormonal therapy with progestins and hysteroscopic resection of the tumour [38]. In countries where gestational carrier is permitted, these women can undergo oocyte or embryo cryoconservation and transfer their embryos into a gestational carrier.
Likewise, in patients with ovarian cancer, only women with early-stage invasive epithelial cancer may undergo utero and ovarian preserving surgery with complete peritoneal staging and systematic pelvic/para-aortic lymphadenectomy [5]. In case of borderline ovarian tumors or germ cell and sex-cord stromal tumors, unilateral salpingo-oophorectomy can be performed or, when both ovaries are involved, ovarian cystectomy should be preferred [39].
Oocyte and/or embryo cryopreservation and ovarian tissue cryopreservation [OTC] are the established methods for fertility preservation when cancer therapy involves gonadotoxic chemotherapy and/or radiotherapy or surgical removal of ovaries [10, 11]. Oocyte and/or embryo cryopreservation requires controlled ovarian stimulation [COS] during 12–14 days [10]. Oocyte cryopreservation is recommended in women without a partner, and it is the only feasible technique according to the law in different countries like Italy or Japan for unmarried women [40].
Different stimulation protocols have been developed for COS in cancer patients, particularly in order to reduce the time to obtain mature oocytes when the women are referred to reproductive medicine specialist during non-menstrual phase of menstrual cycle [41, 42] and in order to avoid circulating estrogens elevation in women with hormone sensitive cancers [43, 44]. With the random-start protocols, it is not necessary to wait for the menstrual period and gonadotropins administration can be started in every moment of the menstrual cycle without reducing ART outcomes [45]. In the past, the biggest concern regarding COS protocols in women with hormone sensitive cancers was the rise of serum estradiol levels. For these women, a COS protocol with the use of aromatase-inhibitor drugs has been established. This protocol is safe and it is comparable to a standard protocol in terms of obtained numbers of mature oocytes and embryos [43, 44].
If the start of oncological treatment cannot be postponed by two weeks, OTC procedure should be offered as a valid and effective technique [11, 46]. This technique allows the collection and cryopreservation of small fragments of ovarian cortical tissue, each one containing hundreds of follicles [47]. A combined procedure with oocyte or embryo cryopreservation may increase fertility preservation potential [48]. OTC is no longer considered an experimental technique since December 2019 by the American Society of Reproductive Medicine [11] and recently Oktay et al. [46] reported 152 live births and ongoing pregnancies. Research on OTC is still going on because this FR technique still has limitations such as the longevity of the transplanted graft (median 33.7 months) [46] and the risk of reintroducing malignant cells [10].
All these techniques require cryopreservation. Vitrification is the gold standard for cryopreservation of embryos and oocytes and it consists in an ultra-rapid cooling process that prevents the formation of ice crystals and consequently the damage of the cells.
The method of choice for cryopreservation for ovarian cortical pieces cryopreservation in slow freezing in fact only few babies worldwide are born from previously vitrificated tissue [47, 49].
Women who cannot delay the start of oncological treatment by two weeks and refuse or are unable to undergo surgery for ovarian tissue retrieval, should be offered the option to receive the administration of GnRHa during chemotherapy [10]. In fact, even if it is still controversial the effectiveness of GnRHa as fertility preservation technique [50], it seems that women who receive GnRHa during gonadotoxic chemotherapy, preserve the ovarian functionality with fewer women experiencing permanent amenorrhea [51].
Women who have a genetic predisposition to develop cancer face additional fertility-related problems, including the transmission of the pre-cancerous mutation to offspring. One example are BRCA-mutated women who face different reproductive challenges.
BRCA genes are involved in DNA double-strand breaks repair mechanisms and their mutations lead to DNA repair deficiency [52, 53]. In animal studies, DNA double-strand breaks repair seems to be essential for maintaining ovarian reserve and its abnormal function is associated with ovarian ageing [54]. Despite the contrasting results that have been reported in humans [55], it seems that BRCA-mutated women tend to have a lower ovarian reserve compared to BRCA-native and to have a worse ovarian response to controlled ovarian stimulation [52, 53]. BRCA1-carriers are encouraged to undergo risk reducing salpingo-oophorectomy (RRSO) at ages 35–40 and BRCA2-carriers at ages 40 and 45; because of this, BRCA patients should complete their reproductive project within this period [56]. When BRCA-mutated women undergo prophylactic RRSO, ovarian biopsies can be performed for ovarian tissue cryoconservation. A careful evaluation must be made before transferring ovarian tissue in BRCA women, due to the risk of ovarian cancer development in the transplanted tissue. Heterotopic ovarian transplantation should also be considered for easier tissue monitoring and easier removal after conceiving [48].
When BRCA women experience breast cancer before prophylactic surgery, they face oncological-treatments that can cause infertility. However, these women also suffer greater ovarian reserve damage due to the DNA repair defect. For this reason, BRCA patients’ oocytes are more vulnerable to chemotherapy [57, 58]. Finally, BRCA women carry an autosomal dominant mutation and they have a 50% chance of transferring it to their offspring [59].
In recent years, long-term survival in pediatric cancer women has steadily increased due to significant therapeutic improvements, especially for hematological cancers. The scientific community has started to focus not only on the prognosis quod vitam but also on the prognosis quod valetudinem. Attention was therefore paid to the issue of POI after gonadotoxic therapies with the possibility of primary amenorrhea and infertility, which is reported to be over 80% [60, 61]. Oncofertility involves some challenges in these patients like the kind of fertility preservation technique to apply and ethical issues, such as the counselling with minors and parents [62]. OTC is the only feasible method for fertility preservation in prepubertal females [11, 47] and the cortical tissue should be retrieved before starting chemotherapy [63]. This technique does not require ovarian stimulation, nor a partner and it can be immediately performed, without delaying cancer therapies. Additionally, it does not even require sexual maturity and it may restore the whole ovarian function, since ovarian tissue also allows steroidogenesis [10]. The amount of tissue that should be removed to ensure good possibility to achieve a pregnancy after autologous cryopreserved ovarian tissue transplantation (ACOTT) has not yet established. While in very young babies one entire ovary should be removed, in older prepubertal girls some authors retrieve one ovary, others make an ovarian resection and others perform cortical biopsies [64, 65]. Further studies are needed to establish the amount of the tissue to be removed in children and in prepubertal and postpubertal girls based on the ovarian size and the estimated number of primordial follicles [20, 47].
A potential limitation of ACOTT is the risk of malignant cell transfer while re-implanting the ovarian tissue, which is strictly dependent on the type of cancer and its stage [63] (see “future possibilities” paragraph for details). Leukemia is the cancer with higher incidence among cancers in pediatric population and, patients with this kind of cancer have an elevated risk of reintroducing malignant cells with ACOTT because of the systemic involvement of the disease [1, 63]. In vitro studies demonstrated the detection of leukemia cells on cryopreserved cortical ovarian pieces through PCR and immunohistochemistry [66]. Malignant cells were not detected when the patients underwent first line chemotherapy and they were in remission [67] therefore for these patients it is suggested to undergo OTC after remission and before bone morrow transplantation [63]. In fact, first line therapy usually has a low risk for gonadotoxicity instead conditioning chemotherapy has a high risk for permanent amenorrhea (see “Oncological treatments with a negative impact on female fertility” paragraph for details). Up to date, few leukaemia survivors received ACOTT and had live births [46]. OTC is recommended also in these women because in the next future new fertility preservation technologies could be applied on cryopreserved tissue without encountering a high risk of disease relapse (see “future possibilities” paragraph for details). While adult women have a cumulative live birth and ongoing pregnancy rate of almost 38% and the natural conception rate is over 60% after ACOTT [49], limited data are available regarding ACOTT outcomes in women survivors of pediatric malignancies. The first live birth after ACOTT in a woman with POI at age 14 years was published in 2015 [60]. ACOTT can also represent a potential tool for puberty induction in patients with prepuberal POI [68]. Patients who do not achieve a physiological puberty induction appear to be exposed to a significant risk of psychosexual disturbances that can severely impact their psychological and physical maturation processes [69, 70]. Case reports in the literature support the efficacy of OTC in inducing ovulation in these patients restoring adequate sex steroid hormone levels [71, 72].
Women who undergo ACOTT need for at least two surgical operations, the first one for the ovarian tissue removal and at least another one for the transplantation [48]. Women with tumors that are at high risk of ovarian contamination, such as ovarian carcinomas and leukemia, have a high risk of reintroducing malignant cells while re-implanting the ovarian tissue [63]. Researchers are working both in developing of a culture system to support oocyte in-vitro development [73] and in the development of an artificial ovary [74, 75, 76, 77] in order to overcome these issues. The ability to support oocyte development entirely in vitro would offer an alternative strategy avoiding both the risk of cancer cells reintroduction and the need for the second surgery for transplantation. Moreover, primordial follicles culture would nullify the need for hormonal stimulation after ACOTT [78, 79]. The ovarian tissue that is recovered for cryopreservation mainly contains follicles in the early stage of development [80]. Researches on how to obtain in vitro mature oocytes from primordial follicles have been ongoing for many years but the follicle growth is a complex mechanism and the accurate knowledge of folliculogenesis is still partially obscure [81, 82]. Various attempts at in vitro follicular growth have been reported in the literature but to date the results are not yet satisfactory and further studies are needed to compare the epigenetic status of oocytes recovered from follicles matured in vitro [78, 83].
Another mechanism to avoid the risk of reintroducing malignant cells is the creation of an artificial ovary to be transplanted to the patient that involves the primordial follicles isolation from the frozen/thawed ovarian cortex and the development of an ovary by reconstitution with somatic cells within a matrix [84]. One of the major limits is the creation of an appropriate scaffold that encapsulates, protects and maintains the follicles and that is capable of degrading to allow the follicle growth and the neoangiogenesis [85]. First polymers to be tested are the natural ones such as alginate, plasma cots and fibrin. They have the advantages to be biocompatible and biodegradable and to contain bioactive factors that promote cell-cell interactions; however, they often have a complex structure and their degradation rate can be difficulty controlled [85]. Collagen seems to be a versatile substance as its stiffness and degradation rate can be modulated by varying fibrinogen and thrombin concentrations [74]. Degradation rate control is improved within the use of artificial polymers such as polyethylene glycol or with three-dimensional bioprinted ovaries using for example gelatine-methacryloyl bioink [75] but these artificial scaffolds can degrade into products that can be toxic at high concentrations and they lack bifunctional molecules. Future researches are still needed regarding the three-dimensional growth of follicles, the growth velocity and the necessary bioactive factors for the creation of a transplantable artificial ovary.
In 2004, a pivotal paper [86] caused the revision of the dogma that established that all female mammals are born with all the oocytes they will ever have in life [87]. Johnson et al. [86] found germline stem cells in the ovary and demonstrated follicular renewal in the mammalian postnatal ovary and others authors reported similar results in different studies [88, 89, 90, 91]. Some authors still contest that the antibody used for the detention of germline stem cells (DDX4) was not specific but can also bind to perivascular cells [92, 93]. Oogonial stem cells and/or follicles obtained from induced pluripotent stem cells could be added to the artificial ovary to increase ovarian reserve [88, 90, 94]. Furthermore, mesenchymal stem cells added to the articular ovary could give greater support to follicular development [95, 96, 97]. If one of these methodologies could be proven effective and safe in human, it would maximize the potential of OTC and it would have many clinical applications relevant to fertility preservation and assisted reproduction.
Among the most common cancer types (breast, lymphoma, leukaemia, thyroid,
melanoma, cervix) that occur during reproductive age [98], women who had
leukaemia, cervical cancer or breast tumor showed the lowest rates for subsequent
pregnancies [99]. Women who had melanoma or thyroid cancer have instead a similar
pregnancy rate as compared to controls, probably because treatments for these
diseases at early stages have no major negative impact on patients’ fertility
[99]. Evidence-based consensus guidelines recommend that conception in cancer
survivors does not appear to increase cancer recurrence risk [100]. The
appropriate time to conceive after chemotherapy has not been determined yet,
however oncologists should establish when the risk of recurrence of the disease
is low and the seeking for the pregnancy can be safe [100]. It is important to
consider that even the oncological follow-up will have to be modified during
pregnancy because it will not be possible use ionising radiation in diagnostic
imaging and to perform nuclear imaging tests. Some women with a good prognosis
following cancer treatment are often advised to delay pregnancy for at least 2
years because any recurrence is more likely to happen in the first 2 years
[100, 101] but, a personalized counselling should be performed considering the
time of completion of therapy, the risk of relapse, patient’s age and ovarian
reserve [102]. Obstetric complications may also be related to the time interval
between chemotherapy and conception. Women who conceived
Cancer survivors can face other long-term risks in addition to an increased risk of infertility such as the recurrence of the cancer and the development of cardiovascular diseases. All these issues might become evident during the pregnancy and complicate it [104, 105]. Negative pregnancy outcomes can be related to specific types of cancer, for example hypertension complicating pregnancy in Wilms tumor survivors [106] or specific cancer treatment such as premature labour in patients that underwent surgery for cervical cancer or premature delivery and low birth weight child in patients treated with pelvic radiotherapy [98, 99, 107]. For these reasons, pregnancy in cancer survivors should be planned and monitored by a multidisciplinary team consisting of gynecologist, oncologist, psychologist and specialists depending on the patient’s anamnestic history such as cardiologist, nephrologist, etc. Despite obstetric guidelines for obstetric women with previous cancer do not exist yet, clinical conditions that could worsen during the gestation should be evaluated before seeking the pregnancy and monitored during the gestation. For example, women who received anthracyclines should undergo an echocardiogram before and during pregnancy to rule out possible heart issues related to previous chemotherapy [108] and women who received trachelectomy should be screened for cervical length as early as the first trimester and during pregnancy to evaluate a possible shortening [109].
One of the major concerns might be the risk of cancer recurrence in women with previous hormone sensitive cancer due to the elevation of circulating estrogen and progesterone levels during pregnancy [110]. Studies showed that cancer recurrence is not increased in hormone sensitive cancer survivors who became pregnant, even if the pregnancy occurs in the first few years after diagnosis [100]. For this reason, these women should not be discouraged from becoming pregnant. A recent study by Poorvu PD et al. [16] demonstrated that many women remain interested in future fertility in the 4 years after a breast cancer diagnosis but only a minority of them attempt to become pregnant and another study reported that 51% of cancer survivors who underwent fertility preservation had a strong wish to conceive about 3 years after treatment but only 29% had tried to conceive [111] and two different studies reported a utilization rate of cryopreserved embryos or oocytes of 8–29% [112] and of 24% [113]. Young cancer survivors may face several barriers to safely and successfully conceiving a pregnancy [22] but a multidisciplinary team should counsel women in the best way to give them adequate information to make conscious choices, knowing the real risks and removing the shadows of fears about what is safe. We hope that the “POSITIVE study” (NCT02308085) can bring clarity and safety also to the clinicians who will then carry out the counselling. Finally, it has been found that cancer survivors are more likely to deliver by an elective cesarean than the general population [106, 114], probably because the history of cancer may lead to increased surveillance and a lower threshold for interventions [115].
Many women with cancer face the risk of infertility after oncological treatments resulting in a poor quality of life. These women should receive information regarding the impact of the oncological treatments on their fertility and the different options for fertility preservation. ACOTT is the only feasible preserving fertility technique in prepubertal girls and it is now no longer experimental, but some limitations are still present like the longevity of the graft and the risk of reintroducing malignant cells. Research is going on in this field to overcome these limitations.
Pregnancies in cancer patients should be planned as they can require closed monitoring but they seem not to have a negative effect on the risk of relapse of the cancer. For this reason, cancer survivors should not be discouraged to become pregnant.
LM and AA supervised the entire study; FE, CV, LN reviewed the literature and wrote the first draft of the manuscript; LM, GC and ASL edited the manuscript; GA and MR revised the manuscript draft. All authors read and approved the final manuscript.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest. ASL and AA are serving as one of the Editorial Board members and Guest editors of this journal. GC is serving as one of the Editorial Board members of this journal. And LM is serving as one of the Guest editor members of this journal. We declare that ASL, AA, GC and LM have no involvement in the peer review of this article and have no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to MHD.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.