1 Department of Medical and Surgical Sciences, Obstetrics Unit, Mother Infant and Adult, University Hospital Policlinico of Modena, 41125 Modena, Italy
2 Department of Biomedical, Metabolic and Neural Sciences, International Doctorate School in Clinical and Experimental Medicine, University of Modena, and Reggio Emilia, 41121 Modena, Italy
Academic Editor: Laura Avagliano
Abstract
Background: The induction of labor (IOL) is a common obstetric
intervention, steadily increasing (one out four pregnancies) in the last years.
This procedure should be considered only when there is a medical indication, and
when the benefits outweigh the maternal and/or fetal risks of waiting for
spontaneous onset of labor. Therefore, this study aims to compare the efficacy of
the IOL in terms of induction to delivery time, mode of delivery, and neonatal
well-being among different evidence-based and non-evidence-based indications.
Methods: This prospective study was conducted at the University Hospital
of Modena, between January and December 2020. We included singleton pregnant
women undergoing IOL, at the term. Intrauterine deaths, small for gestational age
fetuses
Keywords
- induction of labor
- non-evidence-based indication
- PROM
- post-term pregnancy
- ARRIVE trial
- parity
- cesarean section
- the time between induction and delivery
- NICU admission
The induction of labor (IOL) is a common obstetric intervention, steadily increasing (counting approximately one out four pregnancies) in the last years. The Italian rate is overall 24.8% of the 347.772 deliveries (82.077 women) [1] in 2018 and, even in the Emilia-Romagna region, induction represents 29.6% of deliveries in 2020 [2].
According to WHO [3], this procedure should be considered only when there is a medical indication, and when the benefits outweigh the potential maternal and/or fetal risks of waiting for spontaneous onset of labor. Although indications to the IOL progressively increased, most of them lack supporting evidence. Indeed, Italian scientific societies [4] recommend IOL with a good quality of evidence in case of postdate pregnancy, premature rupture of membranes (PROM) at term, hypertensive disorders, and pre-pregnancy diabetes mellitus. Other indications such as gestational diabetes, small for gestational age, cholestasis in pregnancy, oligo/polyhydramnios, suspected macrosomia, assisted reproductive technology (ART), and twins pregnancy reach only low or moderate quality of evidence, thus are not considered as strong indication [5].
Moreover, after the recent publication in the Journal of New England of Medicine of the ARRIVE trial [6], also women with no medical indication for delivery were considered for induction at 39 weeks, because the results of this large American randomized controlled trial, demonstrated better outcomes in IOL group (lower CS rate of 16%, lower hypertensive disorders of 46% and similar neonatal complications) respect than the expectant management (EM) group. However, this trial presents some controversial aspects that may undermine the external validity of this policy at the wide population level [7], because of the different demographic parameters, sociocultural environment, perinatal mortality, and obstetric risk factors of the study population respect the general population, namely the European one.
Indeed, in the ARRIVE trial, the socioeconomic status and maternal age were significantly lower, while body mass index was significantly higher, and the hypertensive disorders were more frequent concerning the Italian cohort. as demonstrated by Tassis et al. [8] and Facchinetti et al. [9].
Finally, against the universal induction policy, a general perception of
“limited satisfaction” of the antenatal care has been reported among women with
induced labor [10, 11], first, because most women planned physiological labor and
birth while acknowledging that birth can be “unpredictable and frightening”
[12, 13] (and these beliefs give a reason as to why 73% of the
Therefore, this study aims to compare the efficacy of the IOL in terms of induction to delivery time, mode of delivery (vaginal or cesarean section), and neonatal well-being among different evidence-based and non-evidence-based indications.
This prospective study was conducted at the University Hospital of Modena,
between January and December 2020. We included singleton pregnant women
undergoing IOL, at the term of gestation (
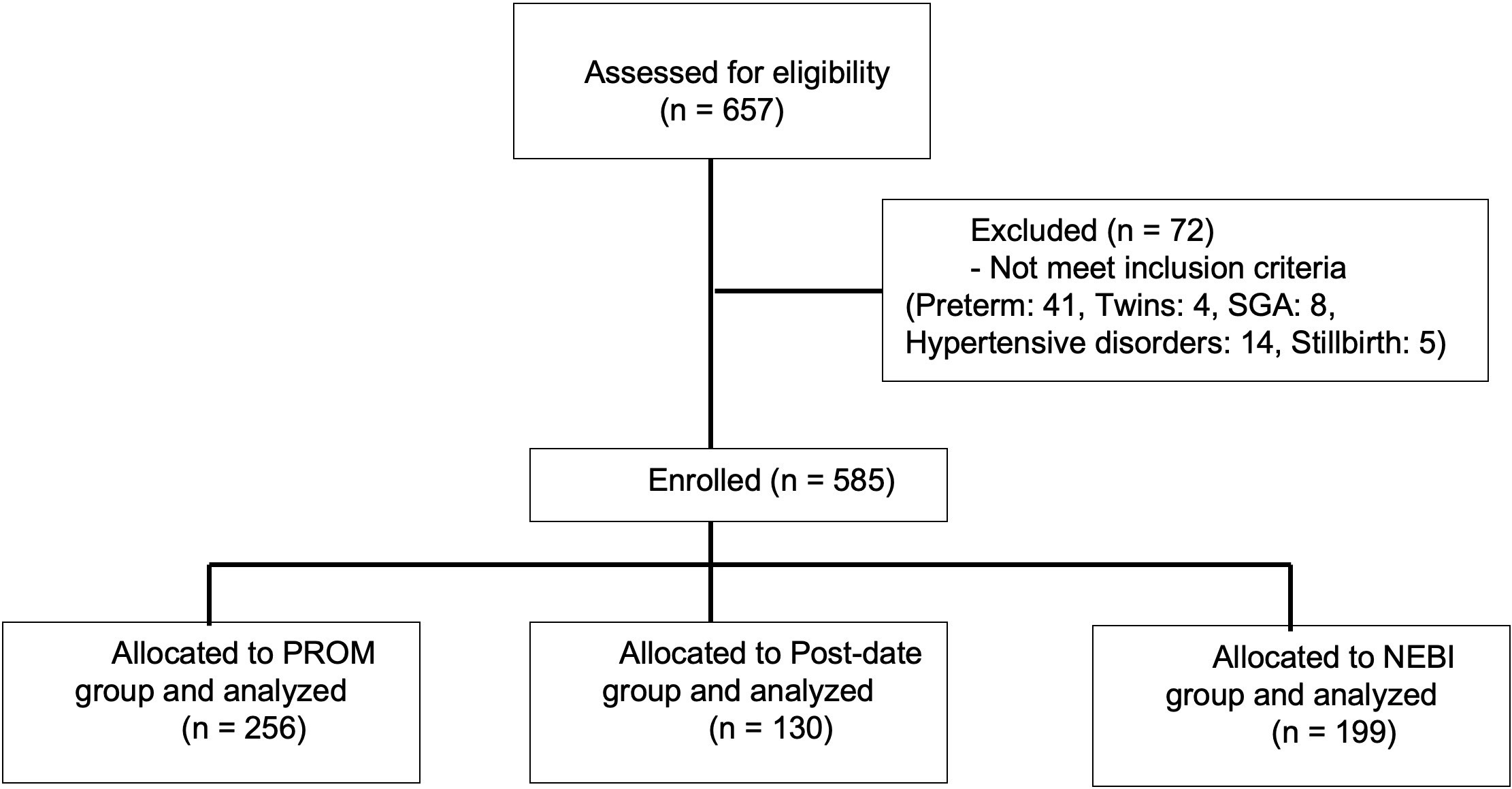 Fig. 1.
Fig. 1.Flow chart.
Women have been subdivided into 3 groups based on the indication to IOL:
premature rupture of membranes (PROM) that exceeds 24 hours (or
The diagnosis of PROM was confirmed by visualization of amniotic fluid passing from the cervical canal and pooling in the vagina, a basic pH test of vaginal fluid, or arborization (ferning) of dried vaginal fluid, which is identified under microscopic evaluation. Rupture of membranes was considered as a delivery indication when spontaneous labor occurred more than 24 hours after PROM. The postdate pregnancy was defined as 41 weeks + 3 weeks of gestation. Gestational age was based either on the first-trimester ultrasound scan or, in women with a regular cycle, on the first day of the last menstrual period if the expected date of delivery differed less than 7 days from that estimated by ultrasound.
Protocol for induction of labor was summarized in supplementary material.
The primary outcome is the time occurring between IOL and delivery (TIME), analyzing separately nulliparous and multiparous women. Moreover, mode of delivery and neonatal well-being through the Apgar at the 5th minute less than 7 and admission to neonatal intermediate or intensive care unit (NICU) were evaluated. As indicated by previous studies, these outcomes are associated with significant risks of neonatal mortality or long-standing adverse health complications, including hypoxic-ischemic encephalopathy [17].
The authors have complied with the World Medical Association Declaration of Helsinki regarding the ethical conduct of research involving human subjects. Approval from the local Institution Review Board was obtained (n: 25094 of 16/9/2020).
As we stratified neonatal outcomes according to delivery indications, we also
compared how maternal, fetal, and neonatal characteristics varied in the case of
PROM, postdate, or NEBI. Categorical variables were presented as n (%) and
tested with the Chi-square test or Fisher’s exact test as appropriate. Normally
distributed continuous variables were presented as mean
A total of 585 women underwent IOL in the study period. Table 1 summarizes
maternal characteristics subdivided by parity. Among the 351 cases of nulliparous
women the three study groups significantly differ in mean maternal age (p = 0.02), mean gestational age at delivery (p
| PROM (n = 256) | Post-date pregnancy (n = 130) | Non-evidence based indication (n = 199) | p value | ||
| Nulliparous (N = 351) | |||||
| Mean maternal age | 32.3 |
33.5 |
34.4 |
0.02 | |
| Country of origin | 0.39 | ||||
| Italy | 104 (62.6) | 50 (60.2) | 64 (61.5) | ||
| Other | 62 (37.4) | 33 (39.8) | 40 (38.5) | ||
| Pre-pregnancy BMI | 24.4 |
23.9 |
25.5 |
0.09 | |
| Obesity (BMI |
16 (9.6) | 8 (9.6) | 17 (17.3) | 0.31 | |
| BMI at delivery | 28.6 |
28.0 |
29.7 |
0.08 | |
| Mean gestational age | 39.1 |
41.0 |
39.4 |
||
| Mean bishop score | 3.9 |
2.6 |
3.1 |
0.0002 | |
| Mild cholestasis | 2 (1.2) | 2 (1.5) | 3 (1.5) | 0.73 | |
| GDM | 14 (8.5) | 6 (7.2) | 11 (10.6) | 0.27 | |
| ART | 2 (1.2) | 1 (1.2) | 2 (1.9) | 0.56 | |
| Suspected Macrosomia | 12 (7.2) | 6 (7.2) | 11 (10.5) | 0.19 | |
| Isolated poly/oligohydramnios | 1 (0.6) | 0 | 2 (1.9) | 0.15 | |
| Multiparous (N = 235) | |||||
| Mean maternal age | 32.2 |
33.4 |
33.9 |
0.07 | |
| Country of origin | 0.31 | ||||
| Italy | 39 (43.5) | 18 (39.5) | 41 (41.8) | ||
| Other | 51 (56.5) | 28 (60.5) | 57 (58.1) | ||
| Pre-pregnancy BMI | 25.3 |
24.2 |
28.6 |
||
| Obesity (BMI |
17 (18.9) | 6 (13.0) | 41 (41.8) | ||
| BMI at delivery | 28.9 |
27.9 |
31.4 |
0.001 | |
| Mean gestational age | 39.0 |
40.9 |
38.9 |
||
| Mean bishop score | 4.0 |
3.8 |
3.4 |
0.23 | |
| Mild cholestasis | 2 (1.2) | 1 (0.8) | 3 (1.5) | 0.58 | |
| GDM | 8 (8.8) | 4 (8.7) | 10 (10.2) | 0.38 | |
| ART | 0 | 0 | 1 (1.0) | 0.45 | |
| Suspected Macrosomia | 7 (7.7) | 4 (8.6) | 8 (10.2) | 0.21 | |
| Isolated poly/oligohydramnios | 0 | 1 (2.2) | 1 (1.0) | 0.29 | |
| Continuous variables are reported as mean Categorical variables are reported as numbers (%). Bold numbers reach statistical significance (p | |||||
No significant differences were found in the frequency of obstetrics NEBI conditions (mild cholestasis, gestational diabetes mellitus (GDM), assisted reproductive technologies (ART), suspected macrosomia and isolated poly/oligohydramnios) in the three groups, except for obesity.
Overall, the median TIME between IOL and delivery was 19 hours, and the mean CS rate was 15.5% (91/585).
In the univariate analysis, shown in Table 2 (Ref. [6]), the main perinatal
outcomes were presented according to delivery indication and parity. Overall,
pregnancies induced for postdate and non-evidence-based indications
registered respectively a significantly higher median time: 19 (10–36) hours and
17 (10–35); p
| PROM (n = 256) | Post-date pregnancy (n = 130) | Non-evidence based indication (n = 199) | p value | |
| Induction to delivery time* (h) | 10 (6–18) | 19 (10–36) | 17 (10–35) | |
| CS rate** | 30/256 (11.7%) | 25/130 (19.2%) | 36/199 (18.1%) | 0.19 |
| Apgar |
4/256 (1.6%) | 3/130 (2.3%) | 8/199 (4%) | 0.26 |
| Adimission to neonatal intensive care unit** | 0/256 (0%) | 3/130 (2.3%) | 6/199 (3%) | 0.02 |
| Intermediate neonatal unit** | 4/256 (1.6%) | 0/130 (0%) | 2/199 (1%) | 0.35 |
| Nulliparous (N = 351) | ||||
| Induction to delivery time* (h) | 12 (8–21) | 27 (15–41) | 26.5 (15–41) | |
| CS rate** | 23/166 (13.9%) | 21/83 (25.9%) | 25/104 (24%) | 0.05 |
| Apgar |
4/166 (2.4%) | 2/83 (2.4%) | 4/104 (3.8%) | 0.76 |
| Adimission to neonatal intensive care** | 0/166 (0%) | 2/83 (2.4%) | 4/104 (3.8%) | 0.05 |
| Intermediate neonatal unit** | 4/166 (2.4%) | 0/83 (0%) | 0/104 (0%) | 0.24 |
| Multiparous (N = 235) | ||||
| Induction to delivery time* (h) | 7 (4–11) | 11 (6–15) | 14.5 (8–27) | 0.001 |
| CS rate** | 7/90 (7.7%) | 4/47 (8.5%) | 11/95 (11.5%) | 0.78 |
| Apgar |
0/90 (0%) | 1/47 (2.1%) | 4/95 (4.2%) | 0.15 |
| Adimission to neonatal intensive care** | 0/90 (0%) | 1/47 (2.1%) | 2/95 (2.1%) | 0.38 |
| Intermediate neonatal unit** | 0/90 (0%) | 0/47 (0%) | 2/95 (2.1%) | 0.58 |
| * Values are given as median and IQR. ** Values are given as numbers (%).
Induction to delivery time (h) has been calculated only for women with vaginal delivery, excluding CS and Operative deliveries. Intermediate neonatal unit: area organized and equipped to provide constant care and treatment for mild to moderately ill infants not requiring neonatal intensive care such as jaundice, late preterm, hypoglycemia requiring endovenous infusion, transient tachypnea, abstinence neonatal syndrome, congenital minor cardiopathies, need to improve feeding competences, newborns of HIV positive mothers [6]. | ||||
Furthermore, in nulliparous, the CS rate in the PROM group was significantly
lower than in the postdate group and the NEBI group (p = 0.05).
Similarly, admission to NICU resulted significantly lower in PROM group respect
than in the postdate and the NEBI group (0 cases), respect then in postdate group
(2 cases of Agar score 5’
Table 3 reported the multivariate logistic regression models that investigated
the role of maternal age, gestational age at delivery, pre-pregnancy BMI, BMI at
delivery, Bishop score, and IOL indication, on the IOL TIME, CS, and NICU
admission in nulliparous and multiparous women. The IOL TIME
| Induction to delivery time |
Cesarean section | NICU admission | ||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Nulliparous | ||||||
| Maternal age (+1 year) | 1.05 (0.9–1.1) | 0.33 | 1.0 (0.9–1.2) | 0.30 | 0.9 (0.7–1.2) | 0.53 |
| Gestational age (+1 week) | 0.99 (0.8–1.1) | 0.86 | 0.9 (0.8–1.1) | 0.41 | 0.9 (0.7–1.2) | 0.97 |
| Bishop score (+1 point) | 0.37 (0.2–0.6) | 0.000 | 0.5 (0.4–0.8) | 0.003 | 0.7 (0.3–1.8) | 0.49 |
| NEBI | 2.4 (1.1–5.1) | 0.02 | 1.5 (0.7–3.2) | 0.32 | 1.6 (0.2–8.9) | 0.65 |
| POST-TERM | 1.4 (0.8–1.6) | 0.47 | 1.1 (0.7–1.8) | 0.50 | 0.6 (0.2–2.3) | 0.46 |
| PROM | § | § | § | |||
| Multiparous | ||||||
| Pre-pregnancy BMI (+1) | 1.1 (0.9–1.2) | 0.22 | 1.1 (0.9–1.2) | 0.32 | 0.96 (0.7–1.3) | 0.86 |
| BMI at delivery (+1) | 1.0 (0.9–1.1) | 0.52 | 0.9 (0.9–1.0) | 0.64 | 1.0 (0.9–1.1) | 0.33 |
| Obesity (BMI |
1.4 (0.8–2.3) | 0.17 | 1.1 (0.9–1.1) | 0.59 | 1.3 (0.8–2.1) | 0.21 |
| Gestational age (+1 week) | 0.8 (0.8–0.9) | 0.000 | 0.9 (0.8–0.9) | 0.01 | 0.8 (0.7–0.9) | 0.002 |
| NEBI | 1.8 (1.2–2.8) | 0.008 | 1.6 (0.9–2.8) | 0.23 | 1.5 (0.3–6.7) | 0.62 |
| POST-TERM | 1.2 (0.7–1.5) | 0.52 | 1.3 (0.9–1.5) | 0.33 | 0.8 (0.5–1.3) | 0.45 |
| PROM | § | § | § | |||
| Multivariate logistic regression models investigating the role of maternal age,
gestational age at delivery, pre-pregnancy BMI, BMI at delivery, Bishop score,
and non-evidence-based indication, on the Induction to delivery time, cesarean
section, and NICU admission in nulliparous and multiparous women.
§: reference group. | ||||||
Our study highlights that the IOL performed for non-evidence-based indications (NEBI) represent about 30% of the inductions in this study population and this datum is comparable to that reported in the literature [18].
The rate of NEBI IOL is progressively increasing, with a crescent need of resources in the Hospital such as additional rooms [19]. Thus, to counteract this phenomenon, it was proposed for the induction of nulliparous, the outpatient cervical ripening, however, only two small sample size trials on its safety have been performed [20, 21].
Moreover, our data confirm the literature highlighting that NEBI IOL compared with IOL for PROM, have longer induction to delivery time (TIME) both in nulliparous and multiparous women. Moreover, this TIME is influenced by the Bishop score and gestational age, in line with other study results such as Rossi RM et al. [22] who provided a risk calculator for CS, available online (https://ob.tools/iol-calc) for health care providers in counseling women who are undergoing induction of labor. Indeed, this score includes the Bishop score and gestational age in addition to other 5 factors.
Moreover, it is worth pointing out that PROM patients of our study seem to have a more favorable prognosis, probably related to the membrane rupture itself, which is usually a strategy used to accelerate labor in women with intact membranes.
Our data are in line with ARRIVE trial [6] where the induced women without indications present a reduced cesarean section rate of 16% and similar neonatal complications respect the expectant management group. Indeed, in our population, CS rate and NICU admission were not increased in the NEBI IOL group and in Post date group comparing with PROM group.
It must be underlined that our population presents different maternal characteristics respect with to those of the IOL group of the ARRIVE trial. Women included in our NEBI group, were certainly older (mean age 33 vs. mean age at randomization 24 years), while less obese (mean BMI 25.1 vs. mean BMI at randomization of 30.5) than the IOL group population of the ARRIVE [9]. Therefore, this compensation could explain the similar results in terms of CS and neonatal outcomes in induced patients with respect than other controls group, despite the different population characteristics (in ARRIVE trial, patients are younger but much more obese).
Those women, induced for NEBI, who delivered vaginally in our study, experimented with a significantly longer TIME respect than women induced for PROM, as already showed by Delorme P et al. and Papalia N et al. [23, 24].
Moreover, in our population nulliparous women presented the same age as the multiparous one. A possible explanation is that in the Italian population, the mean age at first pregnancy is higher respect than in other countries (31.5 years) [12]. On the other hand, multiparous were more frequently foreign women and usually they had the first pregnancy before the Italians. Thus, foreign multiparous result having the same age as Italian nulliparous.
Aside from the impact of an aging population on the economics and burdens of society [25], age is positively associated with both increased CS rate [26] and occurrence of perinatal mortality such as stillbirths (SB) [26], however, in our study maternal age did not influence the perinatal outcome. Moreover, the obesity rate in our population is in line with European data (7.8%–25.5%) [27], and lower respect whit American data such as presented in the ARRIVE trial. This maternal characteristic, which was significantly represented in the multiparous population, at multivariate analysis did not influence the perinatal outcome. Thus, we hypothesize that, as speculated in the studies of Tassis et al. [8] and of Ghi et al. [7], the CS rate of the NEBI group was not worsened by BMI because these patients could benefit from the anticipate of delivery. Indeed, it is well-known that obesity represents one of the major risk factors for obstetric and perinatal complications [28] including intrapartum stillbirth [29] and perinatal asphyxia [30].
The limitation of our study is the lack of detailed perinatal outcomes because more midwives participated in the study, and some data was neglected or poorly collected (pH, BE, etc.). The strengths are represented by the prospective design and the accuracy of collected data namely for the indications of the induction.
Our study confirms that IOL in non-evidence-based indications, leads to an increase in induction to delivery time comparing with women induced for PROM, both in nulliparous and multiparous women, thus it should be justified and carefully evaluated for counselling patients. Further randomized controlled trials (RCT) conducted in European/Italian settings are needed to determine the perinatal outcomes of IOL in non-evidence-based indications.
All authors have accepted responsibility for the entire content of this manuscript and approved its submission. Each author contributed significantly: FM, RP in data collection or management and manuscript writing; DM and GG in data analysis and manuscript writing and editing; FM, ES, GT in the project development and FF in project development and manuscript editing.
The authors have complied with the World Medical Association Declaration of Helsinki regarding the ethical conduct of research involving human subjects. Approval from the local Institution Review Board was obtained (n: 25094 of 16/9/2020). Approval from the local Institution Review Board was obtained (n: 25094 of 16/9/2020) and written informed consent was obtained from each patient enrolled.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

