1 2nd Department of Gynaecology and Obstetrics, Ružinov Hospital, 82101 Bratislava, Slovakia
Academic Editor: Michael H. Dahan
Abstract
Background: During pregnancy, many hormonal, anatomical, and
musculoskeletal changes occur. These changes alter the postural balance and
increase the risk of falls. Falls during pregnancy can cause maternal and foetal
injuries. In our analysis, we focused on women who fell as a result of gait and
balance alterations. The primary objective of this study was to evaluate the
incidence of falls in our study population. The secondary objective was to
identify the risk factors for falls during pregnancy. Methods: 165
healthy singleton pregnant women were included in the study. The participants
were asked to complete a questionnaire regarding their sociodemographic
information, baseline health status and medical history, a detailed interview
about potential falls during pregnancy, and a Modified Falls Efficacy Scale
(MFES) questionnaire. A blood sample was taken to determine the baseline total
circulating 25-hydroxyvitamin D (25(OH)D) level. Based on the evaluation of the
questionnaires, we then divided the participants into two groups—the first
group consisted of women who experienced a fall during pregnancy, and the rest of
the participating pregnant women were included in the control group. Comparing
the two groups, we analysed selected demographic data and a number of other
variables including weight gain, the amount of exercise performed during
pregnancy, and the participants’ vitamin D levels. Results: The
incidence of falls in our study was 12.73%. We found that age was the only
statistically significant independent risk factor for falls during pregnancy
(p-value: 0.0267). We found no statistical difference between the two
groups regarding their levels of serum vitamin D. We also compared relevant
variables in patients who feared the possibility of a fall and those who did not.
We concluded that this fear was mainly associated with participants with BMI
Keywords
- pregnancy
- fall
- vitamin D
- fear
- risk factor
Pregnancy causes many hormonal, anatomical and physiological changes in a woman’s body. These include significant weight gain, mainly in the third trimester, increased ligamentous laxity caused by the hormone relaxin [1], and decreased neuromuscular control and abdominal muscle strength. The altered biomechanics in pregnancy cause an anterior shift in the location of the centre of the body’s mass [2], which induces hyperlordosis of the lumbar spine [3]. Gestational weight gain and adaptive postural changes needed to adjust the anterior-posterior centre of gravity, as well as increased joint laxity, lead to alterations in the static and dynamic postural stability of a pregnant woman [4]. These changes may increase the risk of falls during pregnancy. Moreover, the incidence of falls during pregnancy is higher compared to non-pregnant women of the same age [5]. The risk of falls increases with the gestational age, and the majority of falls are experienced in the third trimester [6]. During pregnancy, falls represent the most common cause of minor injuries (e.g., bruises, scratches, abrasions) and the second most frequent cause of trauma that requires hospitalisation, right after motor vehicle accidents [7]. Pregnant women are 2, 3 times more likely to be hospitalised due to falls than non-pregnant women in the same age group [5]. Falls during pregnancy can lead to many complications, including contusions, sprains, bone fractures and other traumatic complications, but also obstetric complications like abortion, preterm delivery, premature rupture of membrane, placental abruption, uterine rupture, stillbirth, or maternal death [8].
Postural stability in general is improved by regular exercising. Several studies have shown that regular exercise reduces the risk of falling. The majority of these studies were performed in the elderly population, however, a few studies focusing on pregnancy have shown that exercise improves postural stability and could reduce the risk of falls in pregnant women [9, 10]. Regular physical activity during pregnancy leads to a strengthening of the back muscles and improves the body’s postural balance [11, 12].
Recently, vitamin D and its functions has been of great interest in many studies. Vitamin D is known to be a factor in skeletal homeostasis, but it may also have potential effects on the musculoskeletal system [13, 14], immune system [15], cardiovascular function [16], as well as neural development [17]. Decreased vitamin D levels are often associated with a higher risk of falls in the elderly population. The function of vitamin D in pregnancy is not clearly defined. Many studies have confirmed vitamin D deficiency in the general population, but also in pregnant women [18, 19].
We conducted our analysis to assess the characteristics of women who reported any unexpected event in which they came to rest on the ground, floor, or lower level. None of the participants needed to be hospitalized because of the fall. Two participants suffered only minor injuries including small bruises, and/or scratches. In our study, we examined various factors that may increase the risk of falls during pregnancy. Among others, we evaluated the participants’ vitamin D levels to verify if there is an association between vitamin D deficiency and the increased incidence of falls during pregnancy. The primary objective of this study was to evaluate the incidence of falls in our study population. The secondary objective was to identify risk factors for falls during pregnancy.
A flowchart of the study design is presented in Fig. 1.
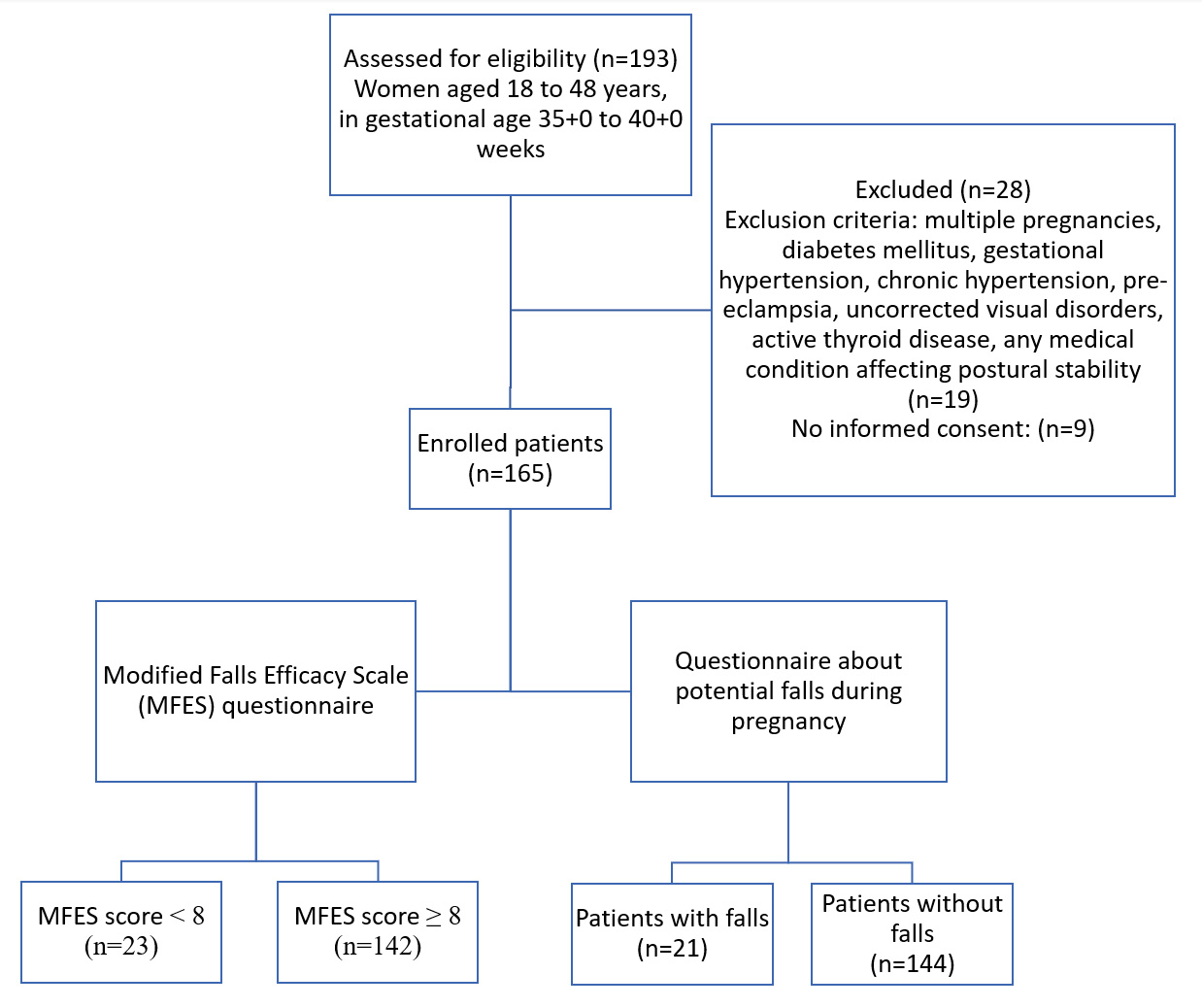 Fig. 1.
Fig. 1.Study flow diagram.
Our study was a retrospective study conducted from the 1st of November 2019 to the 31st of March 2020, in the 2nd Department of Obstetrics and Gynaecology, University Hospital in Bratislava. The study population consisted of 193 pregnant women aged between 18 and 48 years. We selected healthy uncomplicated singleton pregnancies with no associated medical diseases, in the gestational age between 35 + 0 to 40 + 0 weeks. Exclusion criteria were as follows: (1) multiple pregnancies; (2) diabetes mellitus; (3) gestational hypertension; (4) chronic hypertension; (5) pre-eclampsia; (6) uncorrected vision disorders; (7) pregnant women with active thyroid disease (e.g., Graves’ disease, Hashimoto’s disease, or thyroiditis); (8) musculoskeletal or neurologic abnormalities, and any other medical conditions that affect postural stability. Thyroid disorders can affect the levels of vitamin D in the blood. The incidence of vitamin D hypovitaminosis in women with autoimmune thyroid disease is significantly higher than in the healthy population [20].
The participants who provided signed informed consent form were asked to
complete a questionnaire regarding their sociodemographic information, baseline
health status, medical history, and they subsequently underwent a detailed
interview about any potential falls that had occurred during their pregnancy (n =
165). To determine if a fall had occurred, subjects were asked: “Did you fall
during your pregnancy?”. Additional information was collected, including the
gestational age of occurrence, the frequency of falls, the mechanism of injury,
and the medical consequences of the fall. Women were also asked questions about
their physical activities before and during the pregnancy. Additionally, the
participants also completed a Modified Falls Efficacy Scale (MFES) questionnaire.
Based on their responses, the participants were classified as either fearful
(MFES score
A blood sample was taken to determine the baseline total circulating 25-hydroxyvitamin D (25(OH)D) level.
According to our evaluation of the questionnaires, we divided the participants into two groups—the first group consisted of women who did fall during pregnancy, and the rest of the pregnant women were included in the control group. In analysing the data provided by the two groups, we compared selected demographic data and other variables, including weight gain, the amount of exercise during pregnancy according to the completed questionnaires, and the participants’ vitamin D levels.
The laboratory measurement was done in a validated laboratory. We measured the total circulating 25(OH)D concentration in serum samples. The amount of exercise was evaluated according to the given questionnaire. The MFES questionnaire is a questionnaire used to determine the fear of falling during various activities. The aim of its questions was to determine how confident the participants felt when they performed each activity. In our study, we used an adapted MFES from Tinetti et al. [21] and Hill et al. [22]. The original English version of the MFES was translated into Slovak language. The total scores ranged from 0–140; lower scores indicated worse self-efficacy or self-confidence in a participant’s ability to avoid falls. The mean score was calculated by dividing the total score by the number of items; a lower mean score suggested a bigger fear of falling, and a threshold of less than 8 has been used to denote the presence of the fear of falling [23]. Lastly, we compared some variables in patients who feared the fall and in those who did not.
Continuous variables were tested by Student’s t-test, and nominal data
were compared by Fisher’s test. p-values
The characteristics of the total group of patients included in the study are listed in Table 1. The mean age of patients was 30.6. The majority of the participating women were nulliparous. 21.8% of patients listed regular exercise patterns during pregnancy. The mean plasmatic level of vitamin D was 22.5 ng/mL. 48.5% of pregnant women had vitamin D levels lower than 20 ng/mL, which is the threshold of hypovitaminosis according to The Institute of Medicine recommendations [24]. 21 women (21/165–12.73%) reported a fall during pregnancy, while the others did not (144/165–87.27%).
| N = 165 | |
| Age (years), mean |
30.6 ( |
| 35 years and older | 28 (17.0%) |
| Height (cm), mean |
168.2 ( |
| BMI (kg/m |
22.5 ( |
| BMI 25 and more | 33 (20.0%) |
| Nulliparous | 112 (67.9%) |
| 3 times and more weekly exercise before pregnancy | 36 (21.8%) |
| MFES score, mean |
9.0 ( |
| MFES score less than 8 | 23 (13.9%) |
| Vitamin D plasmatic level (ng/mL), mean |
22.5 ( |
| Vitamin D level less than 20 (ng/mL) | 80 (48.5%) |
| Fell during pregnancy | 21 (12.7%) |
| Data are shown as n (%), median (range), or mean | |
Defined characteristics and their comparison in terms of statistical significance between the above-mentioned subgroups of patients (fall during pregnancy vs. no fall during pregnancy) are listed in Table 2. Based on our evaluation, we found that age was the only statistically significant independent risk factor for falls during pregnancy (p-value: 0.0267). We found no statistical difference between the two groups regarding their level of serum vitamin D.
| yes (n = 21) | no (n = 144) | p values | |
| Age (years), mean |
32.6 ( |
30.3 ( |
0.0267 |
| 35 years and older | 5 (23.8%) | 24 (16.7%) | 0.5939 |
| Height (cm), mean |
169.7 ( |
167.8 ( |
0.2372 |
| BMI (kg/m |
21.9 ( |
22.6 ( |
0.4012 |
| BMI 25 and more | 4 (19.0%) | 29 (19.4%) | 0.5862 |
| Nulliparous | 16 (76.2%) | 96 (66.7%) | 0.2718 |
| 3 times and more weekly exercise before pregnancy | 2 (9.5%) | 34 (23.6%) | 0.2306 |
| MFES score, mean |
8.69 ( |
9.05 ( |
0.1586 |
| MFES score less than 8 | 5 (23.8%) | 18 (12.5%) | 0.2892 |
| Vitamin D plasmatic level (ng/mL), mean |
24.4 ( |
22.2 ( |
0.3744 |
| Vitamin D level less than 20 (ng/mL) | 11 (52.4%) | 69 (47.9%) | 0.8808 |
| Data are shown as n (%), median (range), or mean | |||
Table 3 compares some variables in patients who feared the fall and those who
did not. Important findings concluded that fear of fall was mainly associated
with BMI
| Less than 8 (n = 23) | 8 and above (n = 142) | p-values | |
| Age (years), mean |
30.3 ( |
30.6 ( |
0.6991 |
| 35 years and older | 5 (21.7%) | 23 (16.2%) | 0.6902 |
| Height (cm), mean |
166.4 ( |
168.3 ( |
0.1970 |
| BMI (kg/m |
23.1 ( |
22.4 ( |
0.4154 |
| BMI 25 and more | 9 (39.1%) | 24 (16.9%) | 0.0037 (RR: 2.31, 95% CI: 1.24–4.33) |
| Nulliparous | 15 (65.2%) | 97 (68.3%) | 0.9403 |
| 3 times and more weekly exercise before pregnancy | 1 (4.3%) | 35 (24.6%) | 0.0377 (RR: 0.17, 95% CI: 0.03–1.22) |
| Vitamin D plasmatic level (ng/mL), mean |
22.0 ( |
22.6 ( |
0.8009 |
| Vitamin D level less than 20 (ng/mL) | 11 (47.8%) | 69 (48.6%) | 0.5627 |
| Data are shown as n (%), median (range), or mean | |||
According to published studies, the incidence of falls in pregnancy ranges from 13 percent [25] to 29 percent [26, 27]. In our work, the incidence of falls in the study group was 12.7%, which is in on a par with other published data.
Non-severe or severe traumatic injuries during pregnancy have been associated with increased risk of obstetrics complications [28]. Defining risk factors could help with the selection of pregnant women in risk of fall based on simple questionnaires in order to prevent the falls.
There are several studies identifying the possible risk factors that are associated with falls in a population of pregnant women. A systematic review by Hrvatin et al. [6] investigated both extrinsic and intrinsic risk factors as possible causes of falls during pregnancy. Among potential intrinsic risk factors were: age lower than 30, advanced pregnancy, unintended pregnancy, and particular bodily changes (e.g., weight gain, increase in joint laxity, musculoskeletal changes). According to this review, physical activity, education and maternity support belts seem to be beneficial for reducing the risk of falls during pregnancy [6]. In general, exercise intervention has been recommended to improve muscle strength, balance, and gait ability to reduce the risk of falls [28]. Cadore et al. [29] in 2013 examined the effects of multicomponent training on muscle power output, muscle mass, the risk of falls, and functional outcomes in the elderly population. The intervention group performed exercises twice-weekly for a total of 12 weeks. The intervention group showed enhanced muscle power and strength and decreased incidence of falls [29]. A randomized controlled study made by Chittrakul et al. [30] in 2020 found that a Multi-system Physical Exercise program (at least 3 times per week) had a significant effect on improving proprioception, reaction time, knee extension, and balance in the participating pre-frail adults, which reflected improved overall physical performance and reduced the fall risk [30]. A big systematic review, which aimed to retrieve recent evidence examining the potential role of physical exercise interventions in elderly people, provided evidence that physical exercise has positive effects on most of the outcome measurements [31].
There are very little data in current literature regarding potential improvement of postural and dynamic stability in pregnancy. One study on pregnant women made by McCrory et al. [32] in 2010 observed that sedentary pregnant women had a higher rate of falls than women who exercised regularly. They concluded that exercises performed during pregnancy might protect against falls [32]. A review of randomized controlled trials of interventions to reduce back pain in pregnancy found that any land-based exercise was associated with a significant reduction in back pain and improvement in functional disability [33, 34]. Based on these studies, we expected that regular exercise would reduce the risk of falls during the pregnancy, however, we could not confirm this hypothesis. In our study, the women who exercised regularly felt more secure in terms of their postural stability, but, surprisingly, we found no statistical significance in the incidence of falls in women who did and did not exercise. In a study made by Inoue-Hirakawa et al. [23] in 2021 it was concluded that the weight gain in pregnancy may lead to a decrease in balance and increase in fear of falling according to the MFES questionnaire. The difference between our study and the one made by Inoue was that we included pregnant women, whereas, in the mentioned study, they used healthy non pregnant women with simulated gestational weight, using a maternity simulation jacket. This may be the reason why we did not confirm the weight gain as a risk factor for fall. In non-simulated pregnancy, the weight gain is gradual, and therefore the women have time to adapt to this change [23].
A postpartum interview analysis conducted by Harland et al. [35] examined risk factors for injuries during pregnancy. Unplanned pregnancy and young age have been shown to be a risk factor for falls. The authors hypothesize that younger women are more likely to have unintended pregnancies [35]. Age also turned out to be an important risk factor in the publication by Dunning et al. [26], especially in an age group between 20 to 24 years. They attributed this to an increased physical activity in younger patients compared to pregnant women over the age of 35 [26].
In our study, age was the only risk factor for fall with statistical significance. Older women were more likely to fall during pregnancy. In general, the older population is more prone to falls. This is usually due to changes in muscular tonus, muscular mass, lower bone density, and weight gain associated with reduced physical activity. Only some of these factors apply in pregnancy. We did not confirm lower physical activity in women who did fall in pregnancy, nor identified the weight gain as a significant risk factor for falls. This may be related to the relatively small number of patients included in our study. It remains unclear why age is the only risk factor, and thus, these findings require a larger prospective study.
The serum concentration of 25(OH)D can be used as an indicator of nutritional vitamin D status. Although there is no consensus on an optimal plasmatic level to maintain overall health, most agree that a serum level of at least 20 ng/mL (50 nmol/L) is needed for normal bone metabolism [36, 37]. An optimal serum level during pregnancy has not been determined and remains an area of active research. In our study we confirmed that approximately half of pregnant women have vitamin D deficiency, which is in accordance with other studies [38, 39, 40]. The significance of vitamin D deficiency in pregnancy is not yet clear. Many observational studies, supported by compelling in vitro and in vivo data, have generated evidence suggesting that low vitamin D status in pregnancy may also contribute to the risk of adverse perinatal outcomes including hypertensive disorders (e.g., preeclampsia), foetal growth restriction, and preterm birth. However, the few large randomized controlled trials (RCTs) conducted to date have generated conflicting evidence for the role of vitamin D supplementation in improving perinatal outcomes [40, 41]. Vitamin D is associated with bone metabolism. Vitamin D hypovitaminosis is associated with higher risk of falls in elderly population. Vitamin D deficiency in elderly population is associated with an increased postural sway, and greater risk of falling [42]. One study showed that vitamin D supplementation improved postural balance by 9% in vitamin D deficient older adults [43]. In this study, we did not confirm the link between vitamin D deficiency and the risk of falls in pregnant women. The role of vitamin D supplementation in pregnancy is yet to be defined, but it does not affect the postural and dynamic stability to the extent that it would reduce the risk of falls.
There are several limitations to this study including a small sample size, participants bias, and a used research method. Possible limitations of our detailed questionnaire about potential falls during pregnancy could be its reliability and validity, which are in general low. In addition, subjects can misinterpret a question or answer dishonestly. These limitations could be reduced by using posturography as an objective technique to quantify postural control.
In summary, we did not manage to establish any isolated risk factors of falls during pregnancy, except that of higher age. In contrast to other studies, we did not confirm that regular exercise reduced the risk of falls during pregnancy, only that it improved self-confidence in the postural stability of pregnant women. Further study with objective quantification of postural and dynamic stability in pregnant women by using computerised static posturography may help more accurately identify the risk group of pregnant patients and this will be the aim of our further work.
PD, JZ and PO designed the research study. PD performed the research. PD, ZC and MJ analysed the data. PD, JH and ND wrote the manuscript. JZ supervised the project. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
All patients involved in this study signed an informed consent. The study was approved by the Ethics Committee of Comenius University Bratislava on April 24, 2019 under the reference number EK/099/2019 and is registered at www.clinicaltrials.gov under the identification number NCT04482504.
We would like to express our gratitude to all those who helped during the writing of this manuscript, to the peer reviewers for their opinions and suggestions, the editors for their comments and guidance.
This research was funded by Scientific Grant Agency of the Ministry of Education, Science, Research and Sport of the Slovak Republic and Slovak Academy of Sciences (Grant No. VEGA 1/0560/22), Cultural and Educational Grant Agency Ministry of Education, Science, Research and Sport of the Slovak Republic (Grant No. KEGA 032UK-4/2021).
The authors declare no conflict of interest.

