1 Department of Physiotherapy, University North, 42000 Varaždin, Croatia
2 Department of Obstetrics and Gynaecology, Merkur University Hospital, 10000 Zagreb, Croatia
3 Departmet of Obstetrics and Gynaecology, School of Medicine, University of Zagreb, 10000 Zagreb, Croatia
†These authors contributed equally.
Academic Editor: Ugo Indraccolo
Abstract
Objective: This narrative review is presenting the impact of exercise on pregnant women and fetus and provides current recommendations for exercise in pregnancy. Mechanism: Exercise during pregnancy has a numerous effects on both pregnant woman and her fetus. When recommending exercise during pregnancy, it is necessary to keep in mind the physiological responses of the body’s systems during exercise, changes occuring in pregnancy and the influence of this changes on pregnant woman’s body as well as on the fetus and fetal responses to exercise during pregnancy. The type, intensity, duration, and frequency of exercise should be adjusted to the level of physical activity of pregnant women and period of pregnancy in order to achieve clinically significant health benefits. Findings in Brief: Exercise in pregnancy is beneficial for both the mother and her fetus and contributes to the prevention of pregnancy-related disorders. It is recommend to exercise 30 minutes daily five days a week with a tendency to increase the exercise each day in order to accumulate 150 to 300 minutes of exercise per week with moderate intensity. Conclusions: Regular exercise leads to specific adaptation processes of the body systems improving the physical and mental health of pregnant women with positive effect on her fetus.
Keywords
- exercise
- pregnancy
- adjustments
- recommendation
Exercise during pregnancy has an important role in improving and maintaining physical and mental health. Pregnant women are increasingly practicing sedentary activities that lead to many negative outcomes such as weight gain, hypertension and mental health disorders [1]. The incidence of sedentary lifestyle during pregnancy ranges from 57.1% to 78% [1, 2, 3, 4]. Despite scientifically proven advantages and benefits of exercise in pregnancy, pregnancy itself is still represents one of the causes of a significant reduction and avoidance of exercise [5, 6]. Clark and Gross suggest that 39% of pregnant women who exercised before pregnancy did not continue to do so during pregnancy [7]. Similarly, Fell et al. [8] suggest that most pregnant women reduce exercise during the first 20 weeks of pregnancy compared to their pre-pregnancy exercise level. Domingues and Barros report that only 4.3% of pregnant women exercise throughout pregnancy [9] and Gjestland et al. [10] report that 14.6% of pregnant women exercise more than 3 times a week and more than 20 minutes at moderate intensity in the second trimester and 50% of them reduces exercise level to less than once a week during the third trimester. Ribeiro and Milanez reports better results with 29% of pregnant women exercising during pregnancy with 25% of them exercising 3 times a day for 20 minutes [11]. Despite avaiable guidelines that recommend exercise during pregnancy (i.e., 30 minutes a day, most days a week at a moderate intensity or a minimum of 150 minutes per week at moderate intensity throughout pregnancy), less than 15% of pregnant women follow that recommendation [12, 13, 14, 15].
There are numerous published papers about this matter. As well as that, there are numerous guidelines and protocols made in order to describe how to approach the problem of excercise in pregnancy. In this narrative review we did our best to collect all present knowledge and ciritically review all published data to make recommendations more clear and usefull for the clinical practice. As well as that, we wanted to open a further discussion about this matter and stimulate further research all having a goal to get better answers to all problems related to the exercise in pregnancy.
Regular exercise during pregnancy has positive physical and mental effects on the pregnant woman and her fetus [16, 17, 18, 19, 20, 21, 22]. Benefits of exercise for pregnant women include: reduced risk of developing gestational diabetes [23, 24, 25, 26, 27], effective intervention in diabetes management [28, 29, 30], reduced incidence of gestational hypertension [31, 32, 33], preeclampsia [33, 34, 35], peripheral edema [36, 37], varicose veins and deep venous thrombosis [38, 39], reduced incidence of urinary incontinence [40, 41, 42] as well as painful conditions of the spine and pelvis (including sacroiliac dysfunction) [43, 44, 45], weight problems [46, 47] and premature birth [36, 48]. Also, exercise during pregnency is associated with a reduction in the duration of labor [15, 48], cesarean section [32, 49] and instrumental delivery rates [25, 48] and some labour complications [50, 51]. The benefits of exercise in pregnancy for the fetus include increased placental weight and placental growth [52, 53]. Exercise affects amniotic fluid volume and placental volume (vascular volume, capillary surface area and parenchymal density) [15, 54], placental blood perfusion and functional capacity [55], vascular function and improves fetal neurological development [53]. Maternal psychological benefits of exercise include reducing fatigue [56], improved sleep [57, 58], anxiety [59, 60], depression [61, 62], stress and mood improvement [36, 63]. In conclusion, exercise in pregnancy is safe for both mother and her fetus [2, 3] contributing to the prevention of some pregnancy-related disorders [11] and is a preventive and therapeutic measure used to reduce complications of pregnancy and improve the overall health of pregnant women and fetus (Fig. 1) [12, 64].
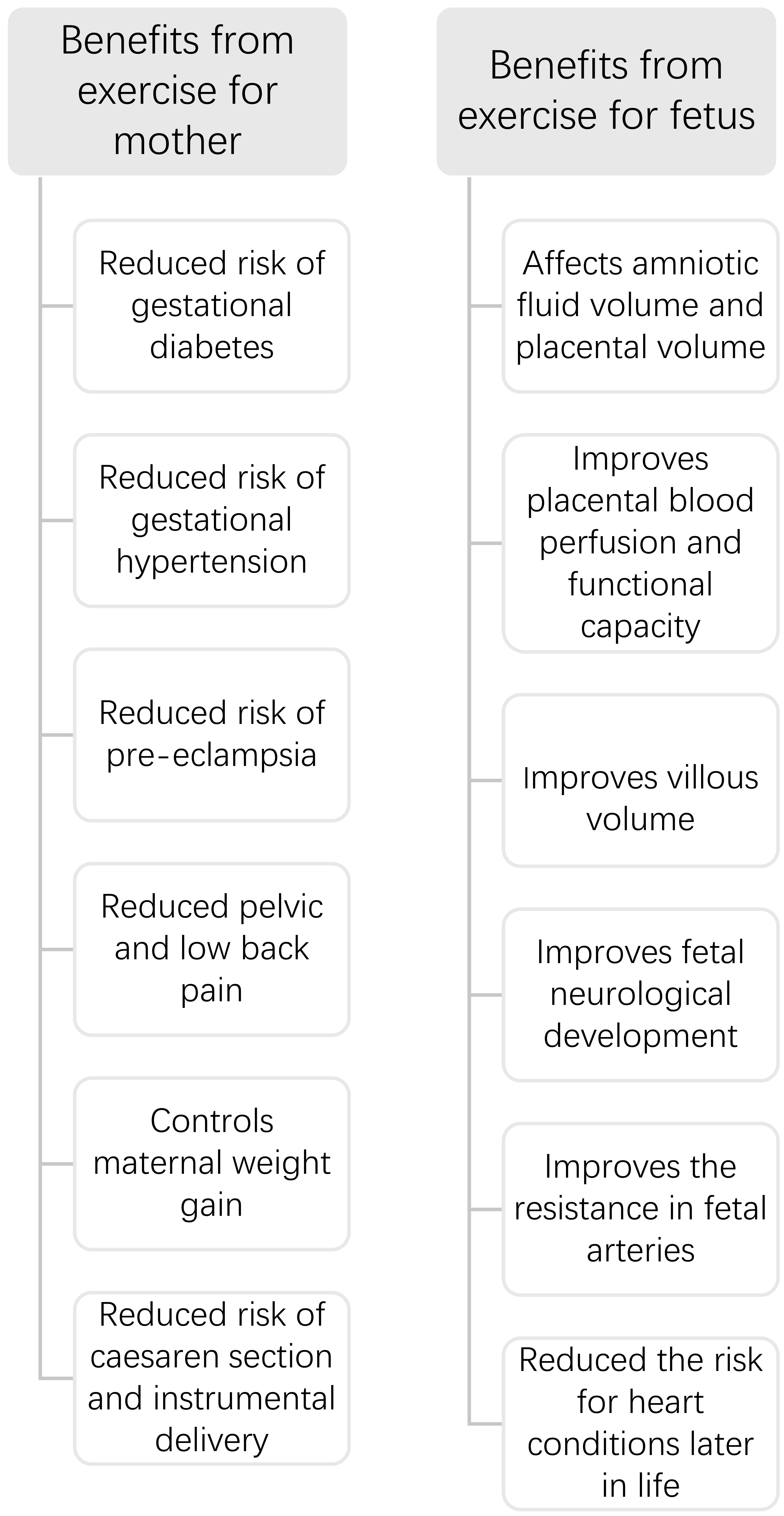 Fig. 1.
Fig. 1.Benefits from exercise for mother and fetus.
Pregnancy is a period of numerous physiological adjustments of the body systems being necessary to achieve a successful outcome. Adjustments and adaptations affect almost every organ and body system and it is necessary to understand all the changes in order to make a difference between physiologic from pathologic. A complete understanding of physiological adjustments will facilitate the development of an exercise program designed for personal needs and capabilities.
The adaptation of the musculoskeletal system to pregnancy leads to changes in the posture of the pregnant women. The constant growth of the uterus is responsible for these changes influencing statics and dynamics posture. Changes in the center of gravity [23, 65], weight gain [23, 65], skeletal changes, increased ligament and soft tissue laxity [23, 65] are the factors that contribute to postural adjustments during pregnancy [66, 67]. The expansion of the uterus anteriorly into the abdominal cavity shifts the center of gravity as manifested by lumbar lordosis and anterior pelvic rotation [65, 67, 68]. Compensation of lumbar lordosis results in increased flexion of the cervical spine, adduction and internal rotation of the shoulder girdle, hyperextension of the knee and reliance on the posterior part of the foot [68]. Adjusted posture during pregnancy leads to the body imbalance, shortening or stretching of muscles, which can result in painful conditions such as sacroiliac dysfunction, low back pain or hip pain [68, 69, 70].
Muscle changes also occur during pregnancy. The most common changes are manifested in the area of the pelvic floor muscles and abdominal muscles. Changes in the pelvic floor muscles often leads to their dysfunction having for a consequence pelvic organ prolapse and incontinence [71] while changes in the abdominal muscles may result in diastasis of rectus abdominis muscles (DRA) [36].
Physiological changes occuring during pregnancy have an important impact on the structure and function of the pelvic floor muscles. As early as in the first trimester, urinary frequency is present, urinary incontinence occurs in 60%; urge incontinence in 10% to 19%, and stress incontinence in 30% to 60% of pregnant women [68]. During pregnancy bladder neck is descending [72], genital hiatus is increasing [72], resulting in increased bladder neck mobility, decreased urethral resistance and decreased compliance [72], elasticity change [72] and pelvic floor contractility [71]. Increased load caused by the uterine growth and weight gain during pregnancy leads to increased pressure on the pelvic floor muscle and bladder, resulting in greater urethral mobility [73]. Also, weight gain causes impaired blood flow and innervation of the bladder and urethra [73]. Due to increased and prolonged mechanical load and collagen changes, there is a decrease in the strength of the pelvic floor muscles [73]. Hormonal and mechanical changes during pregnancy lead to excessive stretching of ligament structures and pelvic floor muscles [74], connective tissue weakness and impairment of normal pelvic floor muscle function [74, 75].
During pregnancy, there is a change in the geometry of the abdominal muscles that still retain their function. Uterine growth affects the shape of the abdomen and the position of the lumbar spine (increase in lumbar lordosis), which results in elongation of the abdominal muscles and changes in the angle of their attachments. This affects their function by reduction of the strength, mainly of the rectus abdominis muscles [76]. In addition to that, streching and flaccidity of the linea alba can occur resulting in an increase in the distance between the medial border of the muscle and a subsequent loss of their straightforward course [76]. The most common change in the abdominal muscles during pregnancy is diastasis or separation of the rectus abdominis mucles in the medial line of the linea alba [76]. The occurrence of DRA contributes to the constant mechanical load on the abdominal wall (due to fetal growth resulting in stretching and weakness of the abdominal muscles) hormonal and consequent changes in the functional capacity of the abdominal muscles during pregnancy [76]. DRA reduces abdominal wall function during pregnancy, affects trunk and pelvic stability and leads to consequent pain in the pelvis, hip and lumbar spine [76]. It also results in difficulties in daily activities that require an increase in intra-abdominal pressure (e.g., defecation, urination, vomiting, etc.) and contributes to the appearance of a hernia [76].
In pregnancy, there is an increase in ligament laxity [67, 23, 68], softening of cartilage and increase in synovial fluid due to elevated concentrations of progesterone [36] and relaxin [67]. This results is increased joint mobility with consequent postural instability. However, in the third trimester there is a decrease in mobility in the ankle and wrist area despite an general increase in ligament laxity. These changes are caused by fluid retention in the connective tissue which can lead to edema [68] and is responsible for development of compression syndromes (e.g., carpal tunnel syndrome, Guyon’s canal syndrome or tarsal tunnel syndrome). Ligament laxity in the pelvic region may lead to the development of sacroiliac dysfunction [70, 77] while ligament laxity in the lower extremities may be associated with pain in the knees, hips and lower spine [78].
Physiological changes of the cardiovascular system in pregnancy maximizes oxygen delivery to the mother and her fetus [68]. Diaphragm displacement and chest shape changes moving the heart upward and towards the left. Also, the heart rotates along its long axis, resulting in an enlarged heart silhouette on some imaging studies [68].
Cardiovascular adjustments during pregnancy include increased blood volume, heart rate, stroke volume, cardiac output, and decreased systemic vascular resistance [67]. Cardiac output is 30–50% higher compared to non pregnant state [67, 68], stroke volume increases by 10% in the first trimester while heart rate increases by 20% in the second and third trimesters [67]. Arterial pressure decreases by 5–10 mmHg from the beginning towards the middle of the pregnancy and then gradually increases [65, 67, 68]. The decrease in arterial pressure is the result of an increase in uterine vascularity, i.e., establishment of uteroplacental circulation and a decrease in systemic vascular resistance. [65, 67]. These hemodynamic changes provides circulatory reserves necessary for better supply of nutrients and oxygen to the pregnant woman and her fetus during rest and also during exercise [67]. There is an increase in total blood volume by about 40–50% [65, 68] as a result of an increase in plasma volume by 50% [65] and red blood cells by 30% [65]. Also, the stroke volume increases by 30% [68] and the heart rate by 17% [65, 68]. It is important to take into account all these cardiovascular changes together with body position adjustments during exercise. In supine position the enlarged uterus compresses the inferior vena cava [68] resulting in reduced venous return [23, 68] and decreased cardiac output. During exercise, blood is redistributed from the visceral organs to the active skeletal muscles [79, 80]. Decreased blood flow to the uterus may temporarily reduce the fetus’ oxygen and nutrient supply [79, 80]. The intensity and duration of exercise affects the amount and intensity of this changes [80].
During pregnancy, the nasopharyngeal mucosa becomes hyperemic and edematous with
mucus hypersecretion due to increased estrogen [68]. These changes often lead to
nasal stuffiness and breathing difficulties [68]. 27% of pregnant women in the
first trimester have nasal congestion and rhinitis, and this incidence increases
to 42% in the 36 week of pregnancy [68]. The shape of the chest changes in early
pregnancy, much earlier that can be accounted for by mechanical pressure from
growing uterus [68]. The reason for these change are in the laxity of the
ligamentous attachments between the ribs and the sternum [68]. The subcostal
angle increases from 68° to 103°, the transverse diameter of the chest
expands by 2 cm, and the circumference of the chest expands by 5 to 7 cm [68]. As
pregnancy progresses, the diaphragm shifts cranially by approximately 4 cm [68].
Diaphragm displacement is caused by progesterone, which acts at the level of
central chemoreceptors in order to increase diaphragm strain resulting in higher
negative inspiratory pressure [68]. Increase in progesterone levels leads to
chronic hyperventilation, resulting in increased tidal volume, from 30% to 50%
in the 8 week of pregnancy [68]. An increase in tidal volume results in an
overall parallel increase in minute ventilation despite a stable respiratory rate
[68]. An increase in minute ventilation, combined with a decrease in functional
residual capacity, leads to a larger-than-expected increase in alveolar
ventilation from 50% to 70% [68]. Chronic mild hyperventilation results in
increased alveolar oxygen (PaO
Exercise during pregnancy can promote morphological changes in placental tissue; it significantly increase villous tissue volume consequently improving placental efficiency [81, 82]. Also, regular exercise during pregnancy stimulates placental surface area by affecting its growth and size [83]. Clapp considers fetal growth and size dependent on the type, intensity, frequency and duration of exercise during pregnancy [82]. By increasing parenchymal component of the placenta, total vascular volume, surface area and capillary volume; exercise improves placental perfusion [36] and villous volume [84]. As fetal para-sympathetic and sympathetic nervous systems become mature and functional during the second and third trimesters, exercise is considered to be effective in increasing fetal heart rate variability and decreasing fetal heart rate [36]. Studies indicate a minimal or moderate increase in fetal heart rate by 10–30 beats/min over baseline during or after exercise [67, 85]. On the other hand, chronic exposure to norepinephrine and other catecholamines essential for fetal growth resulting from exercise will improve fetal cardiac autonomic control [28, 36]. Fetal response to aerobic training during pregnancy include modulation of fetal heart rate and improves autonomic control [83]. Maternal exercise intensity and duration of time spent participating in exercise results in greater adjustments in fetal cardiovascular responses [83]. Aerobic and strength exercises during pregnancy are positively correlated with fetal heart rate adaptability and variability and heart rate variability [83].
Increased muscle mass of pregnant women can contribute to improved ability of placental transport of amino acids necessary for good health and development of the fetus. According to Australian physical activity guidelines for pregnant women, low- to moderate-intensity resistance training may be beneficial for placental-fetal amino acid transport during pregnancy [81]. Regular exercise reduces the pregnant women body fat, which enhances oxygen transfer and reduces the diffusion of carbon dioxide through the placenta, which has a positive effect on fetal development [22, 86]. Exercise during pregnancy improves the resistance in the fetal arteries and reduces the risk for heart conditions later in life [22, 87]. In addition, the sounds and vibrational stimuli that accompany exercise can accelerate fetal brain development [88]. There is the evidence that offspring of mothers who exercised during pregnancy had higher scores on IQ tests and showed higher verbal abilities between the ages of one and five [22, 88].
Absolute and relative contraindications for exercise in pregnancy should be considered before starting exercise. Warning signs to reduce intensity or stop exercising should be kept in mind during exercise in pregnancy.
According to the Society of Obstetricians and Gynecologists of Canada, American College of Obstetricians and Gynecologists and National Institute for Health and Care Excellenc guidelines, absolute contraindications for exercise during pregnancy are ruptured membranes, premature labor, unexplained persistent vaginal bleeding, placenta praevia after 28 weeks’ gestation, preeclampsia, cervical insuficiency, intrauterine growth restriction, multiple pregnancy (e.g., triplets and more), uncontrolled type I diabetes, uncontrolled hypertension, uncontrolled thyroid disease and other serious maternal cardiovascular, respiratory or systemic disorders [14, 24, 89]. Additionally, relative contraindications for exercise in pregnancy are recurrent pregnancy loss, history of spontaneous preterm birth, twin pregnancy after the 28th week, gestational hypertension or mild/moderate cardiovascular or respiratory disease, symptomatic anemia, malnutrition, eating disorders, and some other significant medical conditions [14, 24, 89].
According to the Society of Obstetricians and Gynecologists of Canada, American College of Obstetricians and Gynecologists and Obstetrics and National Institute for Health and Care Excellence guidelines warning signs to stop exercising in pregnancy are persistent excessive shortness of breath (that does not resolve on rest), severe chest pain, regular and painful uterine contractions, vaginal bleeding, persistent leakage of fluid from the vagina (indicating rupture of the membranes), persistent dizziness or faintness (that also does not resolve on rest) [14, 89].
The effectiveness of the exercise program is determined by the appropriate interaction of its main components: intensity, duration, frequency and type of exercise that suits individual pregnant woman individually [90, 91, 92]. The combination of aerobic and resistance exercises [41, 90, 93] is considered to be the most effective for the pregnant woman’s health providing greater benefit compared to aerobic exercises alone [14, 24, 94]. The intensity and type of exercise depends on the functional abilities of the pregnant woman and should be individually adjusted [95]. In general, more physical activity (frequency, duration and/or intensity) is associated with more benefits. Hovewer, there is no scientific evidence that exercising more then recomended provides additional benefits [14]. Exercise in pregnancy contributes to the improvement of cardiorespiratory (aerobic exercise) and musculoskeletal (resistance exercise) status [67].
According to the type, all, aerobic, resistance and flexibility exercise are recommended during pregnancy [67]. Aerobic exercises using large muscle groups in a continuous rhythm are recommended (i.e., walking, hiking, aerobic dancing, swimming, cycling, skating, dancing and skipping rope) [23, 67, 96]. Activities that increase the risk of injuries, such as gymnastics, horseback riding, downhill skiing [14] or those that can result in excessive joint stress, such as jogging and tennis, are not recommended or they should be performed with caution [67] as well as contact activities such as ice hockey, soccer, and basketball [14]. Scuba diving [14] should also be avoided during pregnancy due to the increased risk for the fetus of decompression sickness as a result of the inability of the fetal lungs to filter the bubble formation [67]. Resistance exercise is recommended twice a week, in series of 1–2 with repetitions of 12–15 times. Body weight, weights or elastic bands are recommended for the load [23].
According to the frequency it is recommended to exercise five days a week with a tendency to increase every day. For sedentary pregnant women or overweight or obese it is recommended to exercise three to four days a week [23].
According to the intensity it is recommended to exercise at a moderate intensity which is defined as an activity that is equivalent to 3–4 METS (metabolic equivalent) or brisk walking activity [67, 97] or intensity of 60–90% of maximal heart rate or 50–85% or of maximal oxygen uptake or heart rate reserve [67, 97]. Lower intensity (60–70% of maximal heart rate or 50–85% of maximal oxygen uptake) is recommended for pregnant women who did not exercise regularly before pregnancy [67]. An intensity of 60 to 80% of maximal aerobic capacity is recommended in pregnant women with normal body weight [23].
According to the duration it is recommended accumulation of 30 minutes of exercise during the day five days a week or every day [67, 97] or accumulation of 150 to 300 minutes per week of moderate intensity [23, 43, 84, 95, 98]. Also, a shorter duration of exercise is recommended for sedentary pregnant women, overweight and obese, i.e., 15 to 20 minutes with a gradual increase to 30 minutes [23].
Aerobic exercise during pregnancy stimulates and strengthens the body’s utilization of oxygen [38, 99] and improves overall cardiovascular function [28]. Cardiovascular response during aerobic exercise are an increase in heart rate, stroke volume and cardiac output with minimal or no changes in blood pressure [28, 100]. Also, there is a decrease in resting heart rate and an increase in heart rate variability [28, 100]. These changes are thought to be due to an increase in autonomic control, caused by heart rate variability [28, 101]. Regular aerobic exercise during pregnancy improves blood lipid regulation [87, 100]. In aerobic exercise in water, the main effect of immersion is the redistribution of extravascular fluid into the vascular space resulting in an increase in blood volume [67]. This effect is very quick and is proportional to the depth of immersion leading to a decrease in blood pressure [67]. These changes are associated with a decrease in antidiuretic hormone, aldosterone and plasma renin activity [67]. The change in blood volume leads to a respiratory change with a decrease in vital capacity, ventilation capacity and expiratory reserve volume [67]. Regular aerobic exercise during pregnancy is thought to affect the maturation of fetal cardiac autonomic control, affecting fetal heart rate [28, 101, 102, 103].
Resistance exercise increases muscle strength and endurance [38, 99], contributing to less weight gain during pregnancy, nausea, fatigue and headaches and better overall wellbeing [68]. Resistance exercise is also thought to have some cardiovascular effects [68, 104] being are similar to those in non-pregnant population [68]. Blood pressure is highest when performing strength exercises using larger muscle groups and the heart rate is elevated in all strength exercises of pregnant women [68, 99]. Increase in fetal heart rate is also thought to be present, being similar to aerobic exercise [68, 99]. Also, the frequency, intensity and duration of resistance exercise are inversely related to fetal complications (i.e., intrauterine growth restriction, fetal asphyxia), and resistance exercise is associated with a reduced likehood of fetal complications during pregnancy [105]. During pregnancy, resistance exercise is considered safe and beneficial [38, 68].
The intensity of exercise should be in accordance with the degree of physical activity level of the pregnant woman and the week of pregnancy. Heart rate [14, 38], Borg’s Rating of Perceived Exertion scale and Talk test [23, 89, 90, 99] are suggested in order to determine exercise intensity. All these methods are useful and complementary.
The recommended heart rate for pregnant women under the age of 29 is 102 to 124 beats/min for low intensity, 125 to 146 beats/min for moderate intensity and 147 to 169 beats/min for vigorous intensity exercise [90]. The recommended heart rate for pregnant women over the age of 30 is 101 to 120 beats/min for low intensity, 121 to 141 beats/min for moderate intensity and 142 to 162 beats/min for vigorous intensity exercise [90].
According to Borg’s Rating of Perceived Exertion scale a rating of 12 to 14 on 6 to 20 scale is considered for moderate intensity [40, 99]. Pregnant women with a higher physical activity level are recommended a rating from 15 to 16 or high intensity [23].
According to the Talk test, if a pregnant woman can talk normally, she is considered to be in a zone of moderate intensity, and if she catches air and cannot hold a conversation, she is considered to be in a zone of high intensity exercise [14, 23].
Pregnant women who exercised before pregnancy are recommended to exercise at a moderate intensity and pregnant women with a sedentary lifestyle to exercise with a low intensity with a gradual increase [14, 24, 84, 79]. Pregnant women who have exercised intensively before pregnancy may continue this level of activity during pregnancy according to the guidelines [106].
Before starting exercise, it is necessary to assess the physical activity level of the pregnant woman in order to determine the best exercise program in order to achieve clinically significant health benefits [14]. Physical Activity Readiness Medical Examination for pregnancy (PARMed-X), Get Active Questionnaire for Pregnancy, Kaiser Physical Activity Survey, Pregnancy Physical Activity Questionnaire, (PPAQ) and Godin Leisure - Time Exercise Questionnaire are useful tools for assessment of the degree of physical activity level of a pregnant woman.
Physical Activity Readiness Medical Examination for Pregnancy and Get Active Questionnaire for Pregnancy are questionnaires developed by the Canadian Society for Exercise Physiology. PARMed-X for pregnant women assesses the health status of the pregnant woman, activity habits and physical activity intentions [107]. Get Active Questionnaire for Pregnancy is a simple two-part self-assessment too; the first part contains questions about the health status of the pregnancy and the second part about the physical activity level [108].
The Kaiser Physical Activity Survey is a self-assessment tool that assesses household and family care activities, occupational activities, active living habits and participation in sports and exercise [109].
Pregnancy Physical Activity Questionnaire is adjusted for pregnant women according to the International Physical Activity Questionnaire developed by the World Health Organization. The PPAQ is a self-assessment questionnaire that assesses the type of physical activity (household/caregiving), occupational, sport/exercise and pysical activity level (as sedentary, low, moderate, and vigorous activity) [110].
Godin Leisure - Time Exercise Questionnaire is self-assessment questionnaire for physical activity score in one week longer than 15 minutes [111].
These assessment tools are valuable in the detection of the type, intensity, duration and frequency of physical activity in pregnant woman and designing the exercise program during pregnancy.
Recommendations for exercise in pregnancy have been published through several
international guidelines [14, 23, 24, 89]. It is advisable to accumulate 150–300
minute of exercise per week, with sessions on most days of the week (
| Guidelines | Frequency | Intensity | Time | Type |
| Society of Obstetricians and Gynecologists of Canada | moderate | aerobic and strength exercises | ||
| Royal Australian and New Zealand College of Obstetricians and Gynecologist | every day of the week | moderate, high or a combination of both intensities | 150 to 300 minutes of moderate intensity per week, 75 to 150 minutes of high intensity | aerobic and strength exercises |
| American College of Obstetricians and Gynecologists | moderate | 150 minutes per week | aerobic and strength exercises |
Guidelines from the Society of Obstetricians and Gynecologists of Canada suggest
that all pregnant women without contraindications should exercise in pregnancy,
especially pregnant women who exercised before pregnancy, as well as pregnant
women with gestational diabetes as well as overweight and obese pregnant women
(with pre-pregnancy body mass index
Guidelines from the Royal Australian and New Zealand College of Obstetricians and Gynecologist for exercise in pregnancy in normal pregnancies are the same as the guidelines for the general population (aged 18 to 64 years). It is recommended to exercise 150 to 300 minutes of moderate intensity per week, 75 to 150 minutes of high intensity or a combination of both intensities. In addition to the above recommendations, it is believed that strengthening exercises should be performed at least two days a week. Regular exercise every day of the week for 30 to 60 minutes is encouraged for pregnant recreational and professional athletes, while pregnant beginners should exercise for 20 to 30 minutes. It also emphasizes the reduction of a sedentary lifestyle to a minimum, ie reducing the amount of time spent in prolonged sitting and interrupting long periods of sitting as often as possible by changing body position and/or getting up and walking [23, 114].
Guidelines from the Danish Health and Medicines Authority recommends 30 minutes exercise 3 times a week with moderate intensity during a normal pregnancy [35].
Guidelines from the American College of Obstetricians and Gynecologists recommend that pregnant women should exercise for at least 30 minutes at a moderate intensity, preferably five times a week [86, 89, 96] or every day or 150 minutes per week, avoiding more than two consecutive days without exercise [67]. A combination of aerobic exercise and strengthening exercises at least twice a week is recommended, with at least five exercises involving large muscle groups. Pregnant women who start exercising during pregnancy are advised to exercise with a maximum of 15 minutes of exercise daily three times a week with a gradual increase to 30 minutes of exercise.
Recommendations from the American College of Sports Medicine and the American Heart Association advice increasing exercise in pregnancy by at least 16 MET hours per week [38, 97]. To achieve a minimum of 16 MET hours per week, it is recommended to walk 3.2 km per hour or 6.4 hours per week (2.5 MET, moderate intensity) or exercise on a stationary bicycle 2.7 hours per week (6.0–7, 0 METs, high intensity) [115].
Exercise in pregnancy reduces the incidence of cardiovascular and metabolic diseases as well as painful conditions. Exercise is effective in the management of both conditions improving the symptoms and short and long term outcome. If recommendations for exercise in pregnancy are followed, exercise has no adverse acute effect on the fetus.
Therefore, exercise in pregnancy can and should be recommended form all healthcare professionals due to the well known beneficial effect on the pregnant woman and her fetus.
DRA, diastasis of rectus abdominis muscles; PARMed-X, Physical Activity Readiness Medical Examination for Pregnancy; PPAQ, Pregnancy Physical Activity Questionnaire; MET, metabolic equivalent.
MF and RM contributed equally to the design, analysis the data and writing. All authors read and approved the final manuscript.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest. MF and RM are serving as the Guest editors of this journal. We declare that MF and RM had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to UI.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

