Academic Editors: Ichiro Wakabayashi and Klaus Groschner
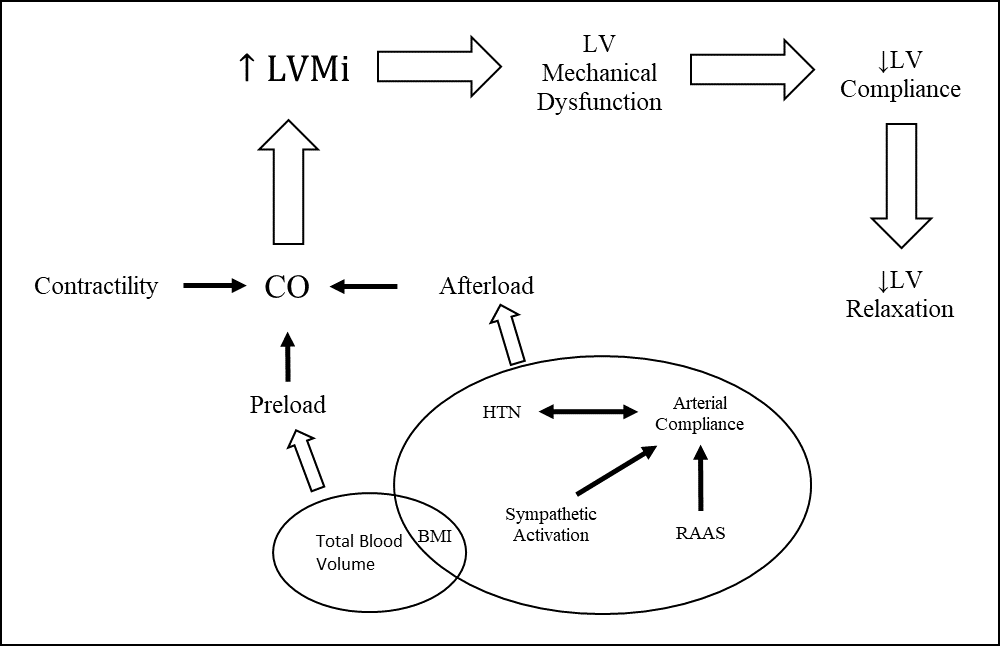
Background: Hypertension is one of the most prevalent diseases in the
United States, affecting an estimated 3.5% of children and adolescents. It can be
adversely affect most organ systems but is particularly detrimental
to the heart and vascular systems. The repercussions can be gauged through well-established
measures of cardiovascular function including left ventricular mass index (LVMI), left
ventricular hypertrophy (LVH), carotid intima media thickness (cIMT), and aortic stiffness.
Cardiovascular function is also affected by underlying etiologies of hypertension
including chronic kidney disease, polycystic kidney disease, coarctation of the aorta, adrenal disorders, renal artery stenosis, obstructive sleep apnea,
as well as various drugs and medications (decongestants, stimulants, Non-steroidal Anti-inflammatory Drugs (NSAIDs), and
steroids). Methods: An exhaustive literature search was conducted for
clinical data regarding pediatric hypertension. Sixty-seven articles were incorporated
with data on 189,477 subjects total. The data was then extracted and categorized
as relating to hypertension incidence, LVMI, LVH, cIMT, and/or aortic stiffness.
Results: The prevalence of pediatric (