Academic Editor: Shigeki Matsubara
Background: In several countries a gap is still present between evidenced-based stillbirth care guidelines and the actual care that parents receive. Knowledge of international guidelines is the first step to give respectful care when a perinatal death occurs. Parents’ trauma could in fact be worsened by inadequate support from health care professionals (HCPs) during and after hospitalisation. Aim of this study is to analyse the knowledge of Italian midwives about the main aspects of clinical management included in international stillbirth guidelines. Methods: The subject of this paper is a post-hoc analysis of the BLOSSoM study. In particular, descriptive statistics was used to analyse the items of Lucina questionnaire (a section of the BLOSSoM study) linked to clinical management of perinatal loss. Results: Four areas of clinical management included in international guidelines were investigated: (1) bereavement care, (2) pharmacological management and aftercare, (3) post-mortem procedures and rituals, and (4) pattern of fetal movements. In the first area, most midwives showed a lack of knowledge particularly regarding natural inhibition of lactation (22.5%) and milk donation (18%). Pharmacological management was characterised by a relevant use of sedatives and analgesia during both labour (38.4% and 89.3%) and childbirth (26.3% and 65.6%). Regarding post-mortem procedures, more than half midwives were not fully aware of Italian law on funerals and related matters, and 37.1% thought that the baby was disfigured during post-mortem examination. Only 30% of the sample answered correctly to the items about the characteristics of healthy fetal movements pattern. Finally, a multivariate analysis was performed to identify independent factors predictive of high knowledge of international guidelines. The variables taken into account were: age, years of work, number of stillbirths assisted, presence in the hospital of a specific protocol and personal training on stillbirth management. Only the last one was significantly associated with a high knowledge of guidelines. Conclusions: Italian midwives are still not fully aware of international guidelines on stillbirth management. The definition of national guidelines endorsed by scientific societies, as well as specific training courses for midwives in Italian hospitals, could be the first steps to improve clinical and psychological management of perinatal loss.
Perinatal loss is a dramatic event for both parents and health care professionals (HCPs). Psychological distress after stillbirth has been reported in almost all HCPs [1] who feel the weight of the responsibility to meet parents’ needs and fear legal consequences [2]. Stillbirth involves millions of couples all over the world every year and it has a profound long-lasting psychosocial impact on them [1]. In Italy, stillbirth happens to nearly 4 women out of 1000 [3] and even if high-income countries’ rates are low compared to low- and middle-income ones, it still represents a huge health issue, comparable to the deaths of infants and toddlers [4].
Perinatal loss (a figure that includes miscarriages, stillbirth and neonatal death) has an extensive impact on parents’ wellbeing; in fact, the loss of a baby at any stage of life fulfils all criteria for a severe traumatic event, as underlined by Paykel et al. [5] in 1971; such events need therefore adequate support and care in order to reduce the risk of a mental health disorder outbreak. The most recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) includes the new dedicated diagnostic category of prolonged grief disorder (PGD), showing how a physiological response such as grief could become a pathological one [6]. Furthermore, suicide is a cause of maternal death [7], its rates are higher in women who lost a baby in the previous 12 months [8, 9, 10] and HCPs could have a pivotal role to prevent it. Conversely, parents’ distress linked to loss can be aggravated by inadequate support during pregnancy, labour, and birth [11]. Couples who are properly assisted express fewer negative emotions during the mourning process [12, 13], so it is important that HCPs work with couples to improve their psychological post-traumatic response [14].
Although many data show how the issue is widespread and impactful, the lack of interest on a social level is diffuse, due to the very nature of the loss that makes it invisible from outside [15]. Moreover, stillbirth is still surrounded by stigma, which affects both relatives of families affected by the loss, and HCPs as well [16]. The latter are at risk of developing burnout syndrome; this is especially true for midwives, whose burnout symptoms have been shown to happen quite early during their career [16]. It should be also noted that adequate professional training, which is the first and maybe the most important step to guarantee respectful care, plays a protective role in the development of burnout symptoms [17].
In Italy, a massive gap has been identified between evidence-based care and the actual care that parents receive [18]. Despite an improvement in perinatal loss care during the last twenty years [19], there are still some critical issues about HCPs training and the subsequent management of pregnancy and stillbirth [18]. Ravaldi et al. [18], in a paper concerning the training of HCPs in perinatal care, showed that around 75% of Italian HCPs had never received proper training on bereavement care. Moreover, the authors evaluated the assistance provided to mothers of stillborn babies with reference to international guidelines and the results were very poor, especially regarding the themes of “respect for baby and parents” and “creating memories” [18]. The study also explored some issues about the type of birth and the use of analgesia and sedatives. This last aspect showed how HCPs beliefs were very far from most of the international guidelines regarding the best labour and childbirth practices [18, 20]. Moreover, the literature suggests that women’s experience with stillbirth could be used as a parameter to evaluate the quality of care which includes clinical and emotional aspects [19].
This paper is a secondary analysis of the BLOSSoM study which, to the best of our knowledge, was the first study, and still the only one, exploring the impact of perinatal care on Italian midwives and its correlation with the knowledge of international guidelines about bereavement care. The aim of this paper is to deepen the knowledge of midwives about aspects of international stillbirth guidelines mainly linked to clinical management. Most of all, the focus is on four areas:
Particular attention will be paid to the knowledge of midwives regarding fetal movements pattern, since it is a very important issue in terms of stillbirth prevention [19].
The aim of this paper is a further analysis of some aspects of the BLOSSoM questionnaire, developed by CR and AV, concerning the clinical management of stillbirth. This survey was the core of the BLOSSoM study [17] and was distributed by CiaoLapo, an Italian charity for perinatal loss support, in collaboration with several hospitals. All participating hospital authorities approved the protocol and authorized the study. All data were collected and analysed anonymously. The BLOSSoM questionnaire was uploaded as an on-line survey using the Surveymonkey platform (https://www.surveymonkey.com).
In brief, the BLOSSoM study was a cross sectional study with four sections:
Methodological details and full text of the survey were published elsewhere [17].
The current paper focuses on the items of the Lucina questionnaire directly linked to clinical management of perinatal death. All participants of the BLOSSoM Study were included in this paper: the sample is composed of midwives working either in the hospital or in different settings. Although no sex or gender criteria were applied, all respondents were female.
Survey responses were downloaded and extracted from the online survey tool Surveymonkey and imported into Excel for data management. Data was cleaned and checked. Quantitative data was imported into Stata/BE 17 (StataCorp) for statistical analysis. Descriptive statistics were used to analyse quantitative data. Categorical data (i.e., answers to binary questionnaire items Y/N) were reported as frequencies (raw numbers and and percentages), whereas continuous data (age and working years) were reported as mean values with standard deviations (SD). Some continuous or discrete variables (i.e., age, years since graduation, working years and numbers of stillbirths assisted) were also recoded into categorical ones and reported as frequencies.
A multivariate analysis (logistic regression) was performed to identify
independent factors predictive of high knowledge of international guidelines
[21, 22]. High knowledge was defined in the BLOSSOM study where each subject was
graded in three classes of knowledge divided into low (correct answer
The maps of respondents’ locations and knowledge of guidelines across Italy were plotted using Tableau Desktop 2020.3 (Tableau Software, LLC, Seattle, WA, USA).
For a better understanding of this paper, some sample features published in the BLOSSoM study [17] are reported next. Four hundred forty-five female midwives with a mean age of 35.1 (SD 9.9) and a mean of working years of 11.2 (SD 10.2) responded to the questionnaire and represented our sample. Participants answered from all over Italy, although most responders worked in hospitals of the following regions: Lombardy, Piedmont, Emilia Romagna, Sardinia and Puglia (Fig. 1). All details about the professional settings where participants worked at the time of the survey and the number of stillbirths they attended to, are published elsewhere and briefly reported in Supplementary Table 1 [17].
 Fig. 1.
Fig. 1.Proportional circle map showing where participants came from.
As mentioned above, the midwives’ answers covered four thematic areas: bereavement care, clinical management and aftercare, post-mortem procedures and rituals, and fetal movements pattern.
As shown in Table 1, there was a general lack of information about some aspects of lactation management after stillbirth, regarding natural inhibition of milk production and donation to a human milk bank. Respectively, only 22.5% and 18% of midwives gave this information to women. Other topics that pertained to bereavement care and had received poor attention were: informing about the so called “empty arms syndrome” and on the possibility of feeling as the baby was still moving in the belly. Regarding the procedures linked to the meeting with the baby, midwives were more informed about mementos, especially about giving ID bracelets and pictures, although still 30.8% of them reported to evaluate the appearance of the baby before deciding to advise parents whether to see them or not.
| Bereavement care | Yes | No |
| Evaluating baby appearance and advising parents whether to see them or not | 30.8% | 69.2%* |
| Giving parents pictures | 69%* | 31% |
| Giving parents a hand or footprint | 66.3%* | 33.7% |
| Giving parents an id bracelet | 74.8%* | 25.2% |
| Giving parents a lock of hair | 32.6%* | 67.4% |
| Informing on empty arms syndrome (pain and discomfort in the arms) | 44.7%* | 55.3% |
| Informing on feeling that the baby is still moving in the belly | 59.6%* | 40.4% |
| Informing on sleep disorders (insomnia or hypersomnia) | 71.2%* | 28.8% |
| Informing on appetite problems (absence of hunger, excessive hunger) | 60.7%* | 39.3% |
| Informing on milk production | 94.6%* | 5.4% |
| Informing on drug inhibition of milk production | 90.6%* | 9.4% |
| Informing on natural inhibition of milk production | 22.5%* | 77.5% |
| Informing on donation to a human milk bank | 18%* | 82% |
| * indicates procedures endorsed by guidelines. | ||
Although the use of analgesia and sedatives is a topic of medical relevance, midwives should know what the current best practices are. This is the reason why the authors included items about these two topics in the BLOSSoM questionnaire (Table 2). Data showed a high use of analgesia during labor and birth, while pointing out a moderate prescription of sedatives during those phases.
| Pharmacological management and aftercare | Yes | No |
| Use of analgesia during labor | 89.3%* | 10.7% |
| Use of sedatives during labor | 38.4% | 61.6%* |
| Use of analgesia during birth | 65.8%* | 34.2% |
| Use of sedatives during birth | 26.3% | 73.7%* |
| After stillbirth more follow up visits are needed | 41%* | 59% |
| Routinely activate the home care | 50.5%* | 49.5% |
| * indicates procedures endorsed by guidelines. | ||
Regarding “aftercare”, additional follow-up visits beyond postpartum physical evaluation were scheduled only in 41% cases after stillbirth and only 50.5% of midwives usually activated home care (Table 2).
Post-mortem procedures and rituals are two crucial issues for both midwives and parents (Table 3). Italian midwives showed a lack of knowledge about these topics. In particular, 66.1% and 61.5% of them respectively thought that a burial request can be submitted after 24 hours from the event and that the law does not allow to bury the baby at any gestational age. Moreover, 62.9% thought that during post-mortem examination the baby could be disfigured.
| Post-mortem procedures and rituals | Yes | No |
| Parents can request burial even under 20 weeks | 75%* | 25% |
| The burial request must be submitted within 24 hours of the event | 33.9%* | 66.1% |
| The law does not set any gestational age limit under which burial cannot be request | 38.5%* | 61.5% |
| Post-mortem examination is indispensable | 60.4%* | 39.6% |
| Post-mortem examination only adds to the couple’s pain | 7.2% | 92.8%* |
| It is best when both stillborn baby’s body and placenta are examined | 75.9%* | 24.1% |
| During post-mortem examination the body will not be disfigured | 37.1%* | 62.9% |
| A partial report of post-mortem examination can also be provided one month after childbirth | 58.4%* | 41.6% |
| Time of post-mortem examination report should not exceed 4 months after childbirth | 66.7%* | 33.3% |
| Parents can see their child even after post-mortem examination | 44.5%* | 55.5% |
| * indicates procedures endorsed by guidelines and/or Italian regulations. | ||
The last area investigated was the “fetal movements pattern” (Table 4). Around one third of the sample thought that fetal movements decreased during the last month or week of pregnancy. Furthermore, 47.6% midwives considered that counting at least 10 movements a day is a right practice to estimate the well-being of the baby.
| Fetal movements pattern | Yes | No |
| Fetal movements decrease during the last month of pregnancy | 29.2% | 70.8%* |
| Fetal movements decrease during the last week when the baby prepares to the birth | 28.1% | 71.9%* |
| Fetal movements are peculiar and specific to each child and remain unchanged until birth | 59.6%* | 40.4% |
| It is enough to count at least 10 movements a day to estimate the well-being of the child | 47.6% | 52.4%* |
| * indicates procedures endorsed by guidelines. | ||
Moreover, there was an inconsistency between the answers of midwives about change of fetal movements pattern during pregnancy. As shown in Tables 5,6, 9.2% and 7.2% of midwives answered both that fetal movements “remain unchanged until birth” and that they “decrease during the last month or week”.
| Fetal movements decrease during the last month | Fetal movements are peculiar and specific to each child and remain unchanged until birth | |
| YES n (%) | NO n (%) | |
| YES | 41 (9.2%)* | 89 (20%) |
| NO | 224 (50.3%) | 91 (20.5%) |
| * indicates contradictory claims. | ||
| Fetal movements decrease during the last week when the baby prepares to be born | Fetal movements are peculiar and specific to each child and remain unchanged until birth | |
| YES | NO | |
| YES | 32 (7.2%)* | 93 (20.9%) |
| NO | 233 (52.4%) | 87 (19.5%) |
| * indicates contradictory claims. | ||
In the end, only about 30% of the sample reported the correct answer to all items about fetal movements: 129 midwives out of 445 (28.9%) correctly reported that fetal movements are peculiar and specific to each child and remain unchanged until birth (not decreasing either during the last month, or during the last week) and it is not enough to count 10 movements a day.
Maps reported in Fig. 2 show the knowledge of midwives of international guidelines’ items on stillbirth care. Data from the BLOSSoM study [17] showed different levels of knowledge for several domains of care in different Italian settings. Here we confirm important differences between various Italian regions regarding the total number of guidelines items known by midwives: in blue, regions where midwives answered correctly to more than the 75% of the items regarding the international guidelines (75% is national median) and in red, regions under 75% (Fig. 2A). Generally speaking, a significant difference was present between the North and the Centre of Italy, and the South (Fig. 2B).
 Fig. 2.
Fig. 2.Map of Italy showing midwives’ level of knowledge concerning international guidelines about bereavement care, divided by regions (A) and between Northern, Central and Southern Italy (B).
A multivariate analysis conducted by logistic regression that included in the model age, years of work, number of stillbirths assisted, presence in the hospital of a specific protocol and personal training on stillbirth management, showed that only attendance to specific courses on stillbirth was significantly associated with a high knowledge of guidelines (Fig. 3).
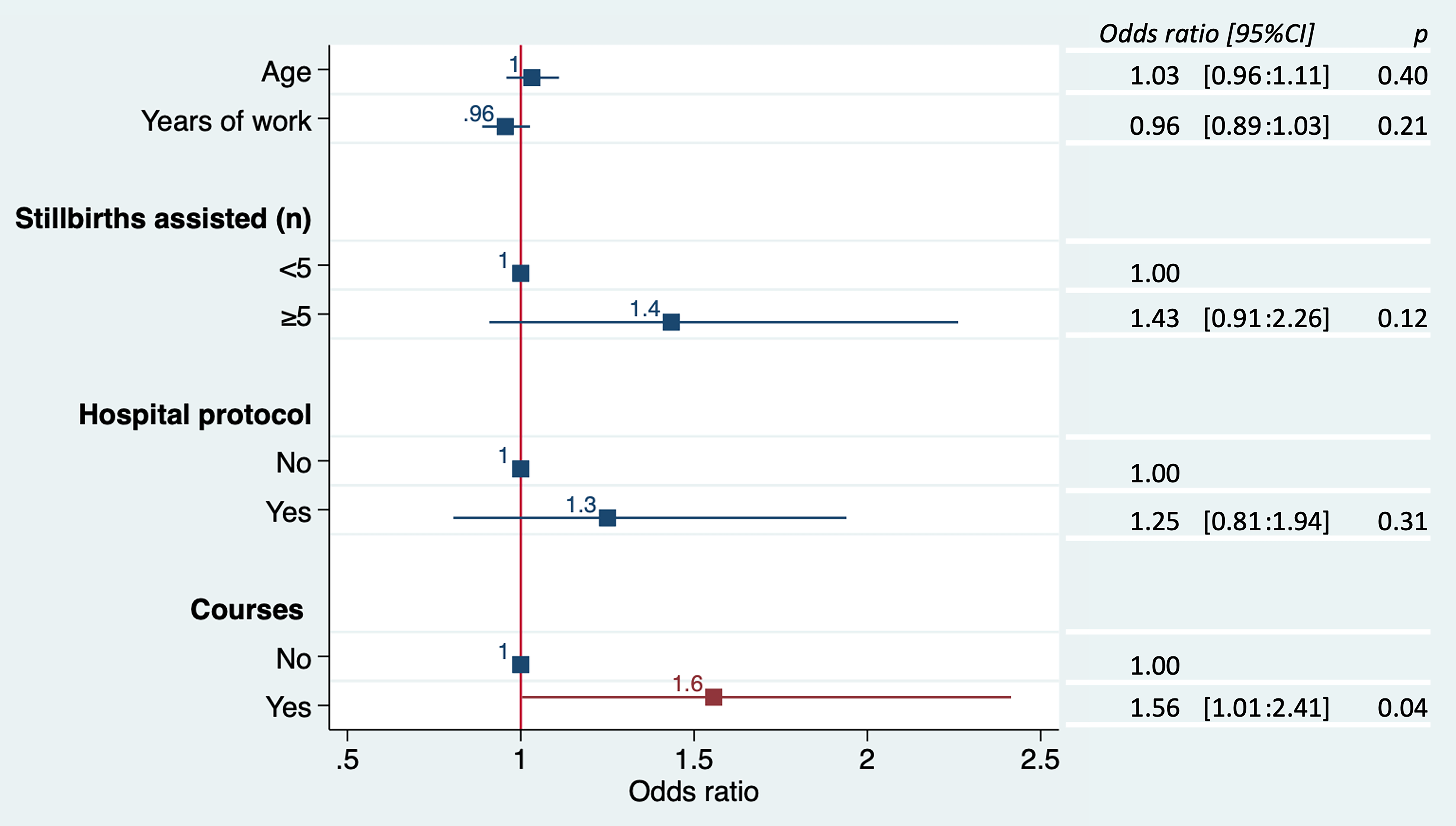 Fig. 3.
Fig. 3.Results of logistic regression showing factors that influence a high knowledge of international guidelines about bereavement care.
Although guidelines on perinatal loss care have been around for many years internationally, a shared intervention protocol is not yet available in Italian hospitals. Therefore, stillbirth care is highly variable and too often it relies on women’s luck to be cared for by those HCPs properly trained and sensitive to this theme.
(1) In the area of bereavement care, the present study underlines that Italian midwives generally inform women about milk production, although most of them have an inadequate knowledge about natural inhibition of lactation and the possibility of milk donation. The consequence is that women do not have an actual opportunity to choose the best pathway for them, since most often the only choice that is available to them is pharmacological inhibition of lactation. In this field literature suggests that donating milk after a loss might even have several benefits: for instance, some women feel more empowered in a time where all certainties about their future have fallen apart. Moreover, it can provide them with an opportunity to redefine their loss and to give it a new meaning. Not less important, donating milk is a repetitive act with the power of becoming a grieving ritual which could have the potential to facilitate the grieving process [23, 24]. Milk inhibition or donation should therefore be a shared decision between the couple and midwives, that is the core of patient-centred care [25].
Midwives showed a lack of information about the possibility that women could suffer from so called “empty arms syndrome” (a condition still to be properly defined, in which bereaved mothers’ arms are aching for not holding a baby) and feel phantom baby kicks, a phenomenon that sometimes happens also in women who had a physiological pregnancy and birth, even after several years. This experience could elicit different feelings such as nostalgia or confusion, leaving women upset [26]. In particular, when a perinatal death happens, these experiences could worsen women’s mental health status and proper information may play a pivotal role to prevent and manage them.
(2) In the area of clinical management, the large use of sedatives and analgesia stands out. Although childbirth analgesia should be always offered to women in cases of stillbirth, it is well known that sedation may instead interfere with the grieving process and make re-living the experience in the days and months later more difficult [20]. Anyway, midwives should not automatically assume that the best choice for women is always the use of analgesia during labour or birth, due to the fact that some mothers may want to experience it without pharmacological aid. When a perinatal death occurs, labour and birth could represent the only moment in common with physiological pregnancies and could be an important piece in the puzzle of parenthood. The choice whether or not using analgesia during labour and childbirth of stillborn babies should always be made together with the mother, in the framework of a shared decision making process.
Regarding aftercare, the majority of Italian midwives did not plan more than one follow-up visit and did not activate any home care service. International guidelines suggest a different pathway of care: more than one follow-up should be scheduled not only with the purpose of physical evaluation, but also in order to provide adequate psychological support [27]; women with a history of psychiatric disorder should also receive particular attention [22]. If possible, follow-up visits should be scheduled outside the maternity unit to avoid parents reliving the trauma [22] Furthermore, midwives should ensure that mothers receive at least one follow-up call or visit at home [21].
(3) Midwives’ knowledge regarding post-mortem procedures is very poor, especially about Italian law on funerals and related matters and the details of anatomo-pathological procedures. One third of the sample wasn’t aware of the possibility to bury a fetus under 20 weeks of gestational age, as it is instead allowed by Italian law [28]. In addition, more than half of the sample thought that the baby’s body is disfigured during the post-mortem examination so that it cannot be shown to parents after the procedure. In particular, this belief could drive their counselling on post-mortem examinations and eventually influence parents’ decision about performing the autopsy, a procedure that is often of paramount importance to understand the causes of death and prevent further perinatal losses [29]. The guidelines of the Perinatal Society of Australia and New Zealand (PSANZ), one of the leading references currently available, recommend that all HCPs involved in bereavement care should be familiar with post-mortem procedures to ensure proper support to couples [21]. The timing of the report of the post-mortem examination is also very important. Results of the autopsy could be a turning point for parents, so it is necessary to schedule a follow-up appointment to discuss about them no later than 12 weeks after the loss [22]. Although according to Italian guidelines on post-mortem examination, preliminary results should be available and provided to parents as soon as possible [27], our results showed that one third of parents waited for them over four months.
(4) The last part of the survey investigated midwives’ knowledge regarding “fetal movements pattern”. One third of the sample thought that a healthy pregnancy is characterised by a decrease in fetal movements in the last month or week and a small percentage of midwives even showed confusion about fetal movements characteristics, answering both that they remain unchanged until birth and that they decrease during the last month or week. Moreover, 47.6% of midwives considered that counting 10 movements a day is the right method to evaluate a baby’s well-being. Actually, about fetal movements frequency changing, the Royal College of Obstetricians and Gynaecologists (RCOG) underlines that the number of movements tends to increase until 32 weeks of pregnancy and then stay about the same [30]. In addition, fetal movements at the end of pregnancy are even more strong and powerful, while a decrease of them is likely associated with intrauterine growth restriction or increased stillbirth risk [31, 32]. It is also important to highlight that fetal movements are unique as the mother’s perception of them [33]. For this reason, teaching women to count at least 10 movements a day is widely considered a wrong practice, due to the large variability of the pattern.
Finally, we have shown an important disparity between regions about midwives’ knowledge of international guidelines, with worse results in the South than in the North or the Centre of Italy. A similar trend is present in the number of perinatal losses which are instead more prevalent in the South [34].
It seems to us that both conditions should be urgently addressed, by means of the definition of shared national guidelines and through specific training courses, focused on specific geographical needs of Southern Italy and aimed both at prevention and management of stillbirth and perinatal loss. As shown in Fig. 3, having participate to specific training courses is the only factor significantly influencing the knowledge of guidelines by interviewed midwives, and, as we have previously shown, the knowledge of guidelines is the most important factor able to provide better management skills in cases of stillbirth and to decrease the risk of professional burnout [17].
The subject of this paper is a post-hoc analysis of the items of Lucina questionnaire pertaining to clinical management of perinatal death. Thus, the main limits are those of the BLOSSoM study published elsewhere [17]. In brief they are: a lack of information about midwives that decided to not participate at the study; the impossibility to define a proper response rate considering that the survey was diffused online and by personal contact in selected hospitals; most responders worked in northern/centre and we cannot be sure that the differences of the knowledge of guideline are due to regional difference or to the minor responders from the South.
The results of this paper suggest that Italian midwives should improve their knowledge about clinical management of perinatal loss. In particular, the most lacking areas are: management of lactation, correct use of analgesia and sedatives, Italian law on funerals and related matters, post-mortem examination and healthy/pathological fetal movements pattern. In particular, the latter issue should receive more attention since monitoring fetal movements patterns could play a crucial role in stillbirth prevention.
Finally, we suggest that the adoption of national guidelines endorsed by scientific societies, shared protocols and the organisation of specific training courses could be important steps to improve perinatal bereavement care in Italian hospitals, particularly in the South of the country, where a general improvement is most needed.
CR & AV led this research including proposal write up and designed the instrument. CR, AV, ECar, AF, ST, ECos, FF collected the data; AV, LM, FM analysed the data; CR, AV, LM, FM, FF discussed data and wrote the manuscript. All authors read and approved the final manuscript.
The survey was voluntary and anonymous, no personal data were recorded, in no way it was possible to identify the single respondents. Informed consent was obtained from all participants. Data were acquired in compliance with GDPR regulation (General Data Protection Regulation, European Union 2016/679). The research proposal was approved and authorized by all participating hospital authorities.
CiaoLapo Foundation for Healthy Pregnancy and Perinatal Loss Support provided infrastructure for the realisation of the study (documents, questionnaires, material, software, web platforms, open access, etc.).
This research received no external funding.
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
