Background: Preeclampsia is a disorder of pregnancy associated with new-onset hypertension after the 20th week of gestation. The aim of this study is to examine frequency of cesarean delivery in pregnant women with risk for developing preeclampsia compared with pregnant women with normal pregnancy. Methods: The prospective study included 240 pregnant women. The experimental group had 120 pregnant women with preeclampsia risk factors. The control group had 120 pregnant women with no pregnancy risk factors. The method of delivery completion was analyzed. Results: In the experimental group, 88 (73.3%) pregnant women completed delivery vaginally, by cesarean section in 32 (26.7%). In the control group of vaginally deliveries were 105 (87.5%), by cesarean section 15 (12.5%). The difference in the frequency of method of delivery between the experimental and control groups is not random (p = 0.009). The chance of completing a delivery by cesarean section 2.54 times is higher in the experimental than in the control group. In the control group, it was found that the RI of uterine arteries in women who delivered by cesarean section was statistically significantly higher than in vaginal delivery (p = 0.038). Conclusion: Cesarean section is the most commonly used surgical procedure to complete delivery in pregnant womens with risk factors for preeclampsia, which confirmed our study.
Preeclampsia is a disorder of pregnancy associated with new-onset hypertension after the 20th week of gestation (WG). As reported The American College of Obstetricians and Gynecologists hypertension and other signs or symptoms of preeclampsia may present in some women in the absence of proteinuria, although often accompanied by new-onset proteinuria [1].The preeclampsia rate in the United States is 6–8% of all pregnancies [2].
Preeclampsia is associated with an unfavorable perinatal outcome, including intrauterine fetal growth restriction (10–25%), placental abruption (1–4%), perinatal death (1–2%), oligohydramnios, and prematurity [3]. The only effective treatment is the delivery of the fetus and placenta. The decision on further expectant treatment sometimes carries the risk of life-threatening for mother and fetus. On the other hand, prematurity leads to a significant increase in neonatal morbidity and mortality [4].
General recommendations are that pregnant women with severe preeclampsia give birth at 32–35 weeks of gestation (WG), as is the recommendation to give birth to pregnant women with early onset of severe preeclampsia, before 25 WG, and before fetal viability is achieved. When giving birth to a pregnant woman with a severe form of preeclampsia from 25 to 34 WG, it requires the decision of an experienced perinatologist [3].
Several studies have shown a higher probability of cesarean section (CS) in pregnant women with hypertension, preeclampsia, gestational diabetes, and infant birth weight over 4000 g [2, 5, 6]. Yücesoy et al.[7] also describe a higher frequency of CS in pregnant women with preeclampsia. First CS is associated with an increased risk of preeclampsia in the second pregnancy [8].
Preeclampsia was associated with an increased risk for severe maternal morbidity and the risk was consistently greater for women with CS relative to those delivering vaginally [2].
There are studies that have tried to determine the value of the method of Doppler analysis of uterine arteries as a screening test for preeclampsia, but also some other pathological conditions [5, 9]. Findings from study of Stampalija et al. [5] generate the hypothesis of the possible efficacy of a first trimester uterine artery Doppler abnormality to predict different clinical phenotipes of hypertensive disorders of pregnancy. Recorded “notching” and increased vascular resistance in the uterine artery is a better predictor of gestational hypertension and preeclampsia than the values of RI and PI [5, 10]. However, we did not find research that determined the values of Doppler analysis as a screening method for the method of childbirth in pregnant women with preeclampsia, so we hope that our research will try to fill this gap.
The aim of this study is to examine frequency of CS in pregnant women with risk for developing preeclampsia compared with pregnant women with normal pregnancy.
This research has been conducted as prospective study at Clinic for Gynaecology and Obstetrics, University Clinical Center Tuzla, Bosnia and Herzegovina. The research included 240 pregnant women, aged 18 to 40, who were regularly controlled and recived antenatal care by their gynaecologists. The participants were divided into two groups, a experimental group and a control group. The experimental group had 120 pregnant women with preeclampsia risk factors (young primiparous women, older multiparous women, previous pregnancy with complications which were caused by preeclampsia, pregestational and gestational diabetes, prepregnancy body mass index greater than 30, thromboembolic events, thrombopilia, antiphospholipid syndrome, systemic lupus erythematosus, kidney disease, hyperemesis gravidarum, proteinuria, pregnancy from assisted reproductive technologies, hypertension in family history). The control group had 120 pregnant women, aged 18 to 40, primaparous and multiparous women, with no pregnancy risk factors, who were regularly controlled and recived antenatal care by their gyneacologists. Exclusion criteria were twins pregnancies, pregnancy with foetal anomalies and stillbirths, pregnant women in whom the increase in blood pressure occurred before the 20th weeks of gestation (WG) as well as pregnant women with chronic hypertension.
All patients were determined the WG before the ultrasound examination. All
patients who were eligible for inclusion in the study were interviewed and the
necessary information was collected, some of the risk factors in either personal
or family history. All pregnant women from the experimental and control groups in
the examined period from 20–22 WG had a sonogram of the uterine arteries with
recording of the value, resistance index (RI), on the left and right uterine
arteries. The technique of finding the uterine artery by Color Doppler was as
follows: first the iliac artery is found laterally from the edge of the isthmic
part of the uterus, then by moving the sound medially the uterine artery signal
is found at an angle of 60 to 90 degrees to the iliac artery. Then we analysed
the waveform, the presence or absence of an endiastolic notch and the RI is
measured. We measured RI on at least three similar consecutive waveforms.
Elevated RI values of the uterine arteries are considered to be RI values
Then, in the same pregnant women, after childbirth, the following parameters were analyzed: the WG at the time of delivery, the mode of onset of labor, the presence of symptoms of preeclampsia, the mode of completion of labor. The mode of onset of labor was analyzed based on whether the labor started spontaneously or it was an induced labor. The method of delivery completion (vaginal, vaginal instrumental or cesarean section) was also analyzed. Preeclampsia symptoms were analysed based on whether the pregnant woman had blood preasure higher than 140/90 mmHg, after the 20th WG and/or present particles of protein in urine (300 mg/L).
All pregnant women before the ultrasound examination signed a written consent. The survey was approved by the Ethics Committee of University Clinical Center Tuzla.
Statistical analysis of data in this research was conducted by using the
standard methods and procedures of descriptive and inferential statistics. The
frequencies of phenomenon were tested with
Analyzing the parity of pregnant women, in the experimental group, primiparous women were 66 (55%), while multiparous were 54 (45%). In the control group, the same number of primiparous and multiparous women were present, 60 (50%).
Considering that the study was performed at the 20–22 WG, the mean value of the
gestational age, when measuring the flow of uterine arteries in the experimental
group was 20.56 (SD
Ultrasound-determined gestational age, when measuring uterine arteries flow, did
not differ significantly between the experimental 0.01 (SD
The mean value of gestational age in the experimental group was 38.74 (SD
Observing the number of risk factors for preeclampsia, it was concluded that in the experimental group the largest number of pregnant women was with one risk factor, most often, hyperemesis in the first trimester of pregnancy 47 (39.2%), without risk factor 37 (30.8%). In the control group, the most represented were pregnant women without risk factor 108 (90.0%), one risk factor had 10 (8.3%) (Fig. 1).
 Fig. 1.
Fig. 1.Shows the prevalence of risk factors for preeclampsia in both groups of participants.
Delivery in both groups was more often completed vaginally. In the experimental group, 88 (73.3%) pregnant women completed the birth vaginally, by caesarean section (CS) in 32 (26.7%). In the control group of vaginally births were 105 (87.5%), by CS15 (12.5%) (Fig. 2).
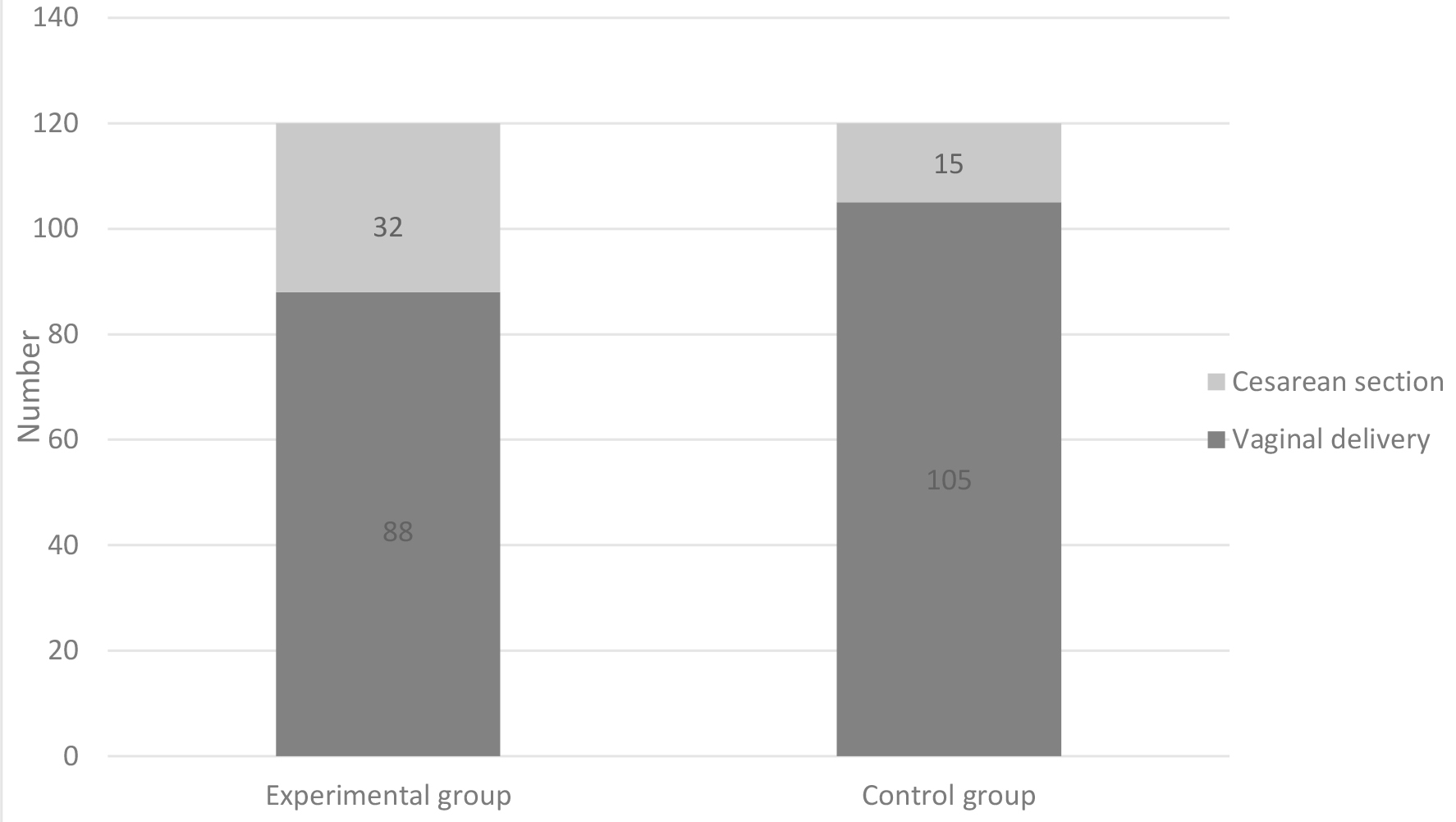 Fig. 2.
Fig. 2.Method of delivery in both groups.
The
By determining the RI of the uterine arteries, in the period from 20 to 22 weeks of gestation, the mean value of the RI of the uterine arteries in the experimental group of pregnant women was 0.55, in the control group the mean RI of the uterine arteries is 0.52. The student’s t-test revealed a statistically significant difference in the mean values of the RI of uterine blood vessels between the experimental and control groups of pregnant women (t = 2.005, p = 0.0045).
The dependence of labor completion on the RI of uterine arteries was analyzed for all subjects (combined experimental and control group). The student’s t-test did not determine a statistically significant difference in the RI of uterine blood vessels between CS and vaginally method of delivery (t = 1.19, p = 0.235).
In the experimental group delivery was completed by CS in 32 (26.7%), delivery stimulated in 53 (44.2%), induced in 26 (21.7%) and 8 (6.6%) woman underwent a manual revision of the uterine cavity after delivery. In the control group delivery was completed by CS in 15 (12.5%), delivery stimulated in 48 (40%), induced in 52 (43.3%) pregnant women, revision performed in five (4.2%) women (Fig. 3).
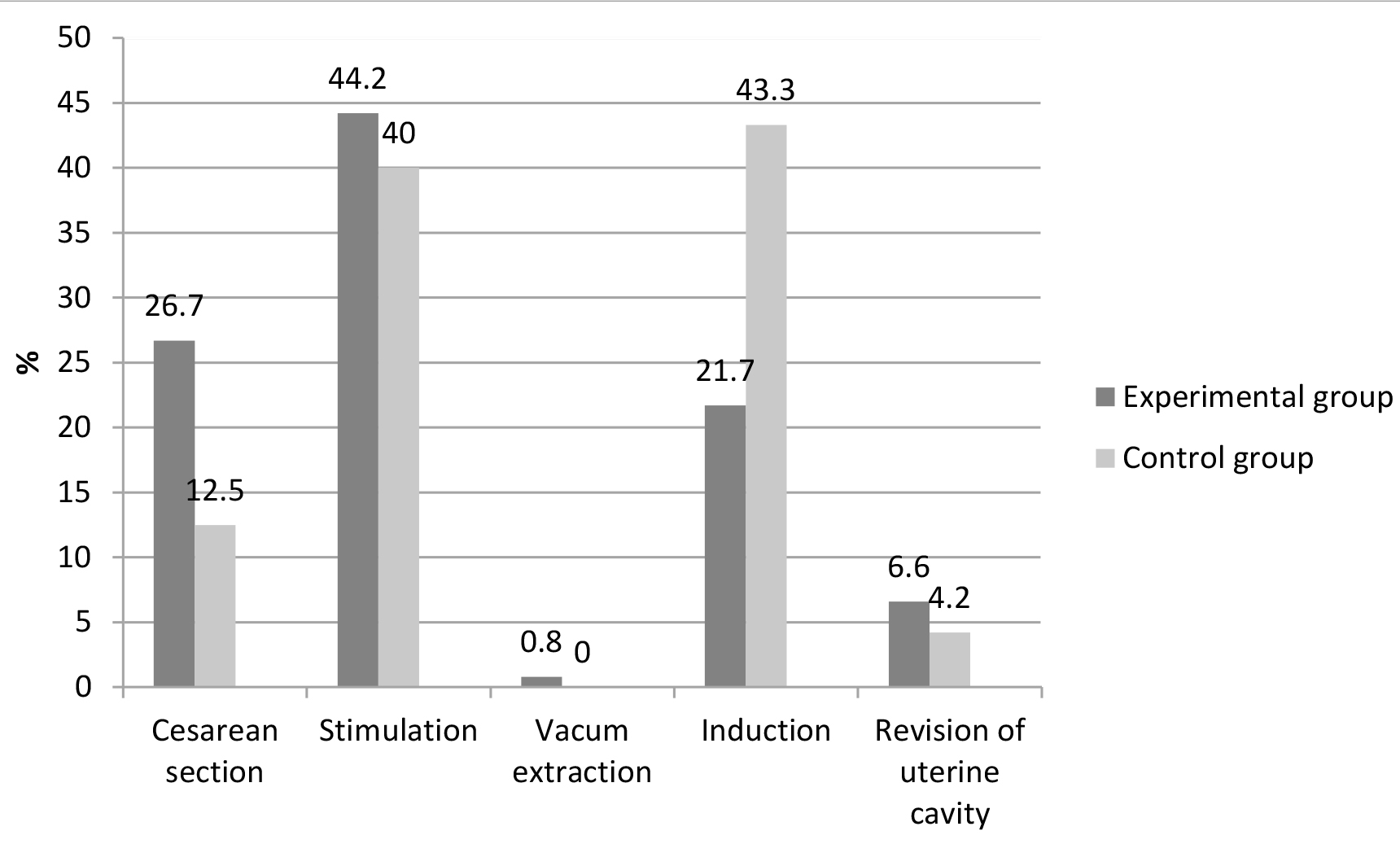 Fig. 3.
Fig. 3.Shows obstetric interventions during delivery (stimulation of already started delivery by oxitocin, induction of onset of delivery by prostaglandins, vacuum extraction, revision) as well as operatively completed deliveries (CS).
In the experimental group, only one (0.8%) pregnant woman completed the delivery with the help of a vacuum extractor, in the control group there were no deliveries completed with the help of a vacuum extractor.
The statistical significance of the difference in the RI of the uterine arteries in groups was analyzed separately. The student’s t-test did not determine a statistically significant difference in the RI of the uterine arteries in vaginal and CS deliveries in the experimental group (t = 0.324, p = 0.746). In the control group, it was found that the RI of uterine arteries in women who delivered by CS was statistically significantly higher than in vaginal delivery (t = 2.10, p = 0.038).
Primiparas are more prevalent in the group of pregnant women with preeclampsia in many analysed research, from 50% to 77.7%, in which range our results fit also [13, 14, 15, 16].
In our study, it was found that there is a statistically significant association between increased resistance of uterine arteries and parity of pregnant women. The chance of developing an incerased RI of the uterine arteries is 2.42 times higher in primiparous women than in multiparous. The difference in the frequency of incerased uterine artery RI values is not random. The occurrence of hypertension in pregnancy is associated with significantly higher values of the RI of the uterine and umbilical arteries especially in primiparous women [17], which correlates with the results of our research.
Nathakomon et al.[18] in a prospective study found a mean gestational age of 20.64 WG in the study group of pregnant women, similar to the results of our study. Napolitana et al.[15] had a slightly higher mean age of pregnancy during their study, the mean gestational age in the second trimester was 22.0, and the mean age of termination of pregnancy was 37.1 WG. Singh et al.[19] during their study had a mean gestational age similar to that in our study of 21 WG.
In the study by Singh et al.[19] the mean gestational age at the end of pregnancy was 40 WG, slightly higher than in our study. Gyselaers et al.[20] in the group of pregnant women with late preeclampsia had a mean age of termination of pregnancy also lower than the gestational age in our study.
In pregnant women with high-risk pregnancies, such as those with preeclampsia, delivery is usually induced prematurely and ends instrumentally or surgically in the interest of the mother and/or fetus [2]. The higher frequency of CS in the experimental group in our study is not accidental. Pregnant women with risk factors for preeclampsia are 2.54 times more likely to have CS. There was no statistically significant difference in the values of the RI of uterine arteries between pregnant women delivered by CS and those vaginally in the experimental group.
In study Boulet et al. [2] there was evidence of positive additive interaction between preeclampsia and CS, with the highest risks for severe maternal morbidity observed among women with both factors. It is crucial to educate clinicians on this association and to encourage providers to offer and encourage vaginal deliveries in this high-risk population of women [2].
In a study by Nagar et al.[21] of 500 pregnant women with some of the symptoms of preeclampsia, 30% had an emergency CS and 12% had an elective CS.
In the research by Ilić [22] in normotensive pregnant women in 33.3% of deliveries was completed by CS, while in pregnant women with hypertension in 61.7% was completed by CS, which is a higher percentage in both groups of pregnant women in compared to the results of our research.
Similar results were obtained by Mashiloane et al.[23] who had 63% of pregnant women delivered by CS in severe preeclampsia, which is more than in our study. According to the same authors, delivery was induced in 37% of pregnant women, which is similar to the results of our research.
Geum et al.[8] concluded that CS in the first pregnancy is associated with an increased risk of developing preeclampsia in the second pregnancy (OR, 1.35; 95% CI, 1.09–1.67). Pregnancy complicated with preeclampsia is more likely to end in CS, stillbirth, and neonatal death [24], which agrees with the results of our study. In 2010, hypertension or preeclampsia were the reasons for 3.1–12.8% induction of delivery in New South Wels, Queensland, South Australia and Tasmania which is lower than the results of our study and 2.3–4.8% CS in Queensland and South Australia [25].
In the study by Abdelaziz et al.[26] there was a significantly higher number of CS in the group of pregnant women with early preeclampsia (75.0%) as well as late preeclampsia (51.7%) compared to the control group of pregnant women (7.9%), which correlate with the results of our study. Turkish authors also describe a higher incidence of CS (63.8%) in pregnant women with preeclampsia [7].
Babović et al.[13] also had a higher percentage of CS in pregnant women whose pregnancy was complicated by preeclampsia and IUGR, 58.5% of emergency and 41.5% of elective CS, which is a higher percentage than in our research.
The increase in CS number has also been the result of defensive obstetrics outside the framework of good clinical practice over the past two decades.
By measuring the RI of uterine arteries, during a routine antenatal examination around 20 WG, pregnant women with an increased risk of developing preeclampsia can be detected, thus the complications that preeclampsia brings with it and also high prevalence of deliveries by CS. In our study there is no statistically significant difference in RI of experimental group when it comes to the method of delivery. The significant difference is only observed in control group.
However, in order to relate higher RI of uterine arteries in preeclampsia and the delivery by CS, numerous and much larger multicentric studies are needed to confirm or deny this thesis.
The strenght of this study is prospective nature of the study. Limitations are the relatively small number of study participants and unicentricity which affected the precision of our estimates. Our statistical analysis not included determination of Risk Ratio and multiple logistic regression to determine the adjusted risk of CS after controlling potential confounders. However our study has led to a several of interesting findings.
Cesarean section is the most commonly used surgical procedure to complete delivery in pregnant womens with risk factors for preeclampsia, which confirmed our study.
LK and AC designed the research study. LK and AC performed the research. MR, AK and MJ provided help and advice on the experiments. DH analyzed the data. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the University Clinical Center Tuzla (approval number: 01/1-37-4-123/11).
Thanks to all the peer reviewers for their opinions and suggestions which improved the quality of our manuscript.
This research received no external funding.
The authors declare no conflict of interest.
