-
- Academic Editor
-
-
-
The Perceval device is a sutureless, rapid-deployment valve designed to shorten aortic cross-clamp (ACC) and cardiopulmonary bypass (CPB) times, with the aim of improving postoperative outcomes in older, high-risk patients.
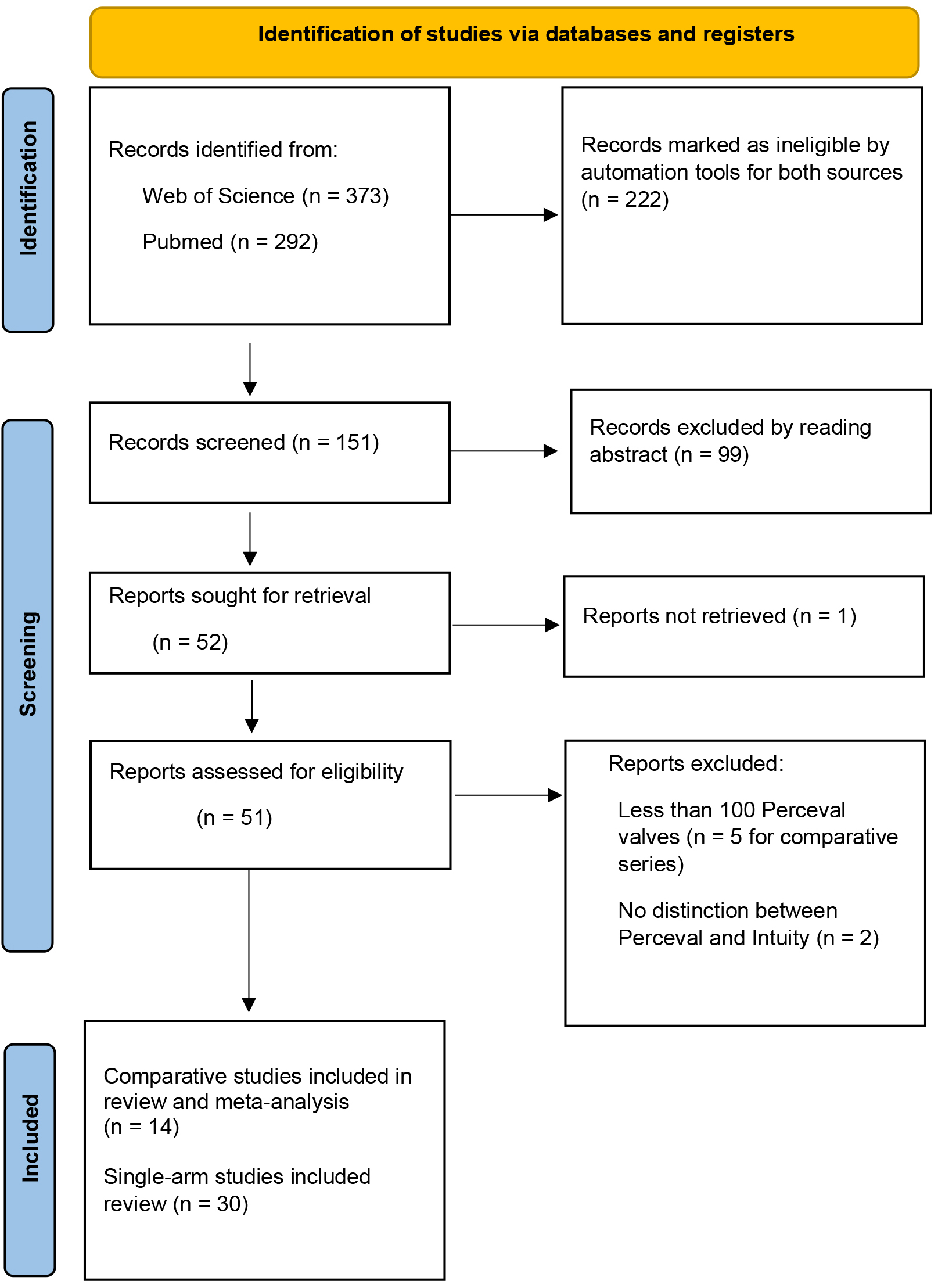
A systematic review was conducted for full articles published between 2020 and 2024, comparing the Perceval valve with conventionally sutured valves, with a focus on preoperative and operative data, as well as postoperative outcomes. Single-arm series were retained for the same purpose. Articles with at least 100 valves were included.
A total of six propensity score-matched series and four randomized controlled trials were identified after removing articles with data from the same patient population. Consequently, age and risk scores were comparable. The use of a minimally invasive approach and the association of other procedures, such as coronary artery bypass grafting (CABG), varied depending on the research design. Adverse postoperative events were comparable for both valve types, except for the development of conduction defects, which required the implantation of a permanent pacemaker (PPM). The initial PPM implantation rate was higher for the Perceval valve, as shown in 5 of the 14 comparative series; however, this rate decreased after the adaptation of surgical techniques. A meta-analysis showed that the CPB and ACC times were significantly shorter using the Perceval valve, at 14.9 (8.2–21.5) minutes and 16.6 (12.1–21.2) minutes, respectively. Platelet counts after implantation were lower with no clinical consequences, and the hemodynamic performance of the Perceval device was acceptable and stable over time. The survival and durability of the Perceval valve were also acceptable, with a reoperation rate of 1% at the 5-year follow-up.
The Perceval valve appears to be a suitable alternative for older, high-risk patients undergoing aortic valve replacement. Notably, the Perceval valve is associated with shorter surgical times and could facilitate the advantage of minimally invasive surgery. The need for postoperative PPM implantation remains an issue.