-
- Academic Editor
-
-
-
To investigate the factors that influence blood transfusions after neonatal cardiac surgery and their association with prolonged mechanical ventilation (PMV) to provide a basis for optimizing blood transfusion strategies.
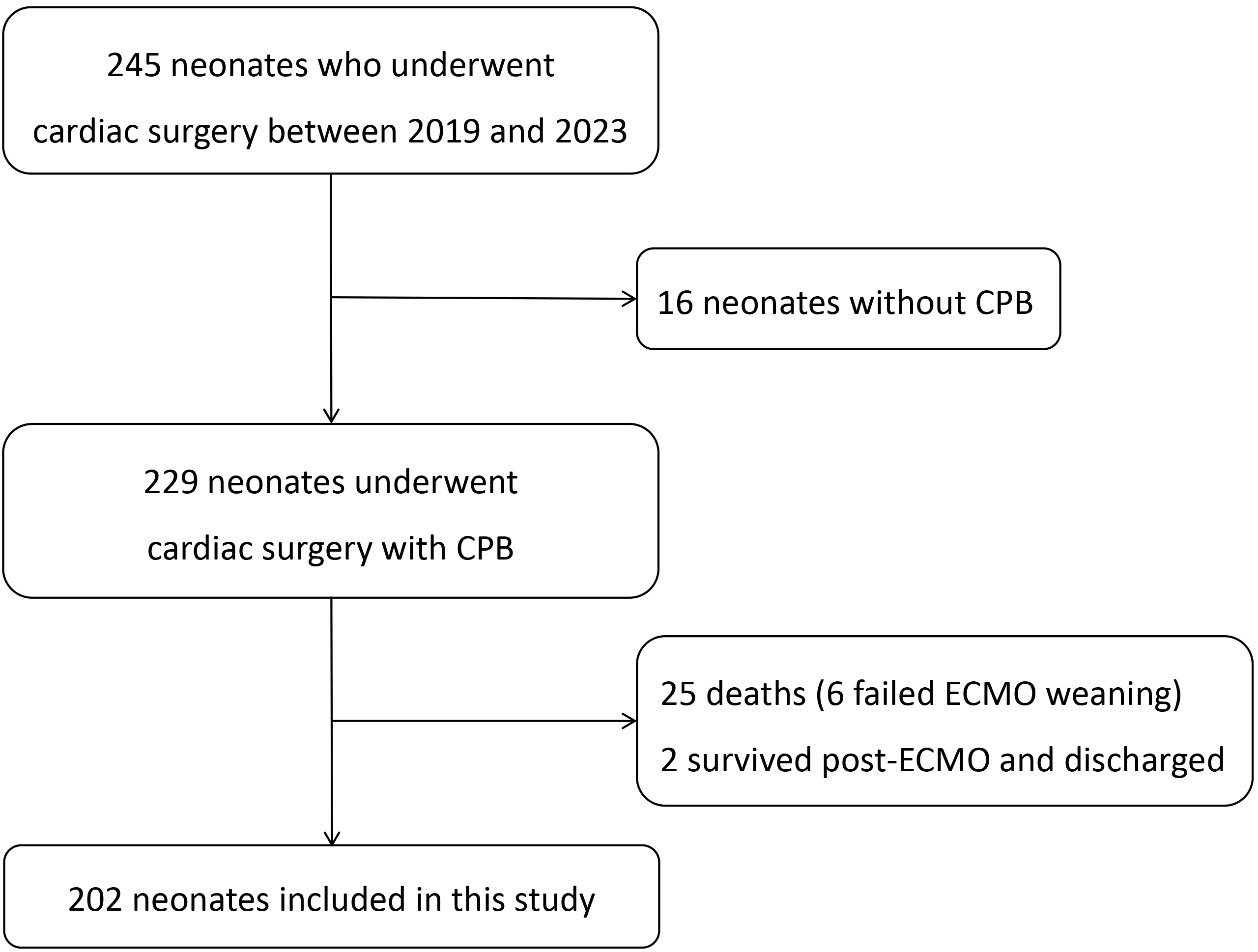
This study retrospectively analyzed the clinical data of 202 neonates who had undergone cardiac surgery with cardiopulmonary bypass (CPB) in Beijing Anzhen Hospital from 2019 to 2023. Demographic data, preoperative parameters (body weight, hemoglobin, Risk-Adjusted Classification of Congenital Heart Surgery 1 (RACHS-1) score), intraoperative data (CPB time, aortic cross-clamp time, deep hypothermic circulatory arrest (DHCA)), and transfusions of red blood cells (RBCs), fresh frozen plasma (FFP), and platelet concentrate (PC) within 48 hours after surgery were collected. PMV was defined as mechanical ventilation ≥96 hours after surgery. Multivariate logistic regression was used to analyze independent risk factors for PMV, and the dose–response relationship between transfusion volume and PMV was evaluated by restricted cubic splines (RCSs).
Within 48 hours postoperation, 50.00% of patients were transfused with RBCs, 37.62% were transfused with FFP, and 27.72% were transfused with PC. The PMV incidence was 36.63% in patients with lower body weight (odds ratio (OR) = 0.38, 95% confidence interval (CI): 0.20–0.74; p = 0.005), lower preoperative hemoglobin (OR = 0.99; 95% CI: 0.97–0.99; p = 0.041), and a RACHS-1 score of 4 (OR = 2.56; 95% CI: 1.04–6.27; p = 0.040), and RBCs (OR = 2.02; 95% CI: 1.02–4.00; p = 0.043), and FFP infusion (OR = 1.98; 95% CI: 1.02–3.85; p = 0.043) were independent risk factors. The RCS demonstrated a linear dose–response relationship between the volume of RBCs infused and PMV (p nonlinear = 0.668), whereas there was no association for FFP. The duration of intensive care unit (ICU) stay in patients with PMV (14 days vs. 8 days) and the hospitalization (18 days vs. 13 days) were significantly longer (both p < 0.001).
Blood transfusion after neonatal cardiac surgery is an important controllable risk factor for the development of PMV, and its risk increases linearly with the volume of RBC transfusion. Future multicenter prospective studies are needed to validate the causal association further.