- Academic Editors
-
-
-
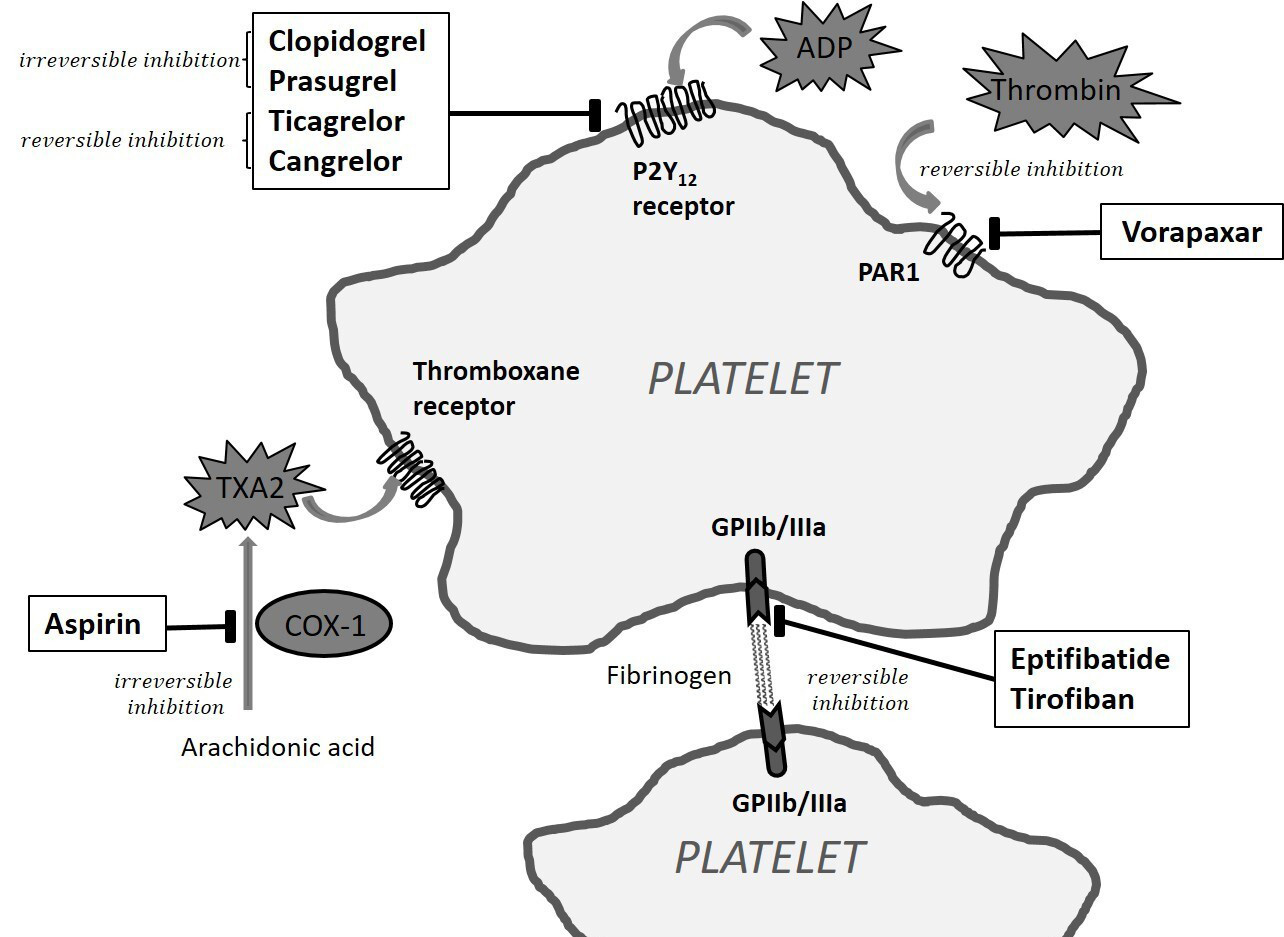
Antiplatelet therapy plays a pivotal role in the management of atherosclerotic cardiovascular diseases, providing critical protection against thrombotic complications. However, the role of antiplatelet therapy in primary prevention is limited, as an elevated risk of bleeding often offsets the potential benefits. Meanwhile, long-term antiplatelet monotherapy in secondary prevention provides clear benefits for stable patients. In the setting of acute coronary syndromes, dual antiplatelet therapy, which combines aspirin with a P2Y12 inhibitor, such as clopidogrel, prasugrel, or ticagrelor, has demonstrated superior efficacy over aspirin alone, with prasugrel and ticagrelor offering more rapid and potent effects. However, the increased bleeding risk associated with more intensive regimens necessitates careful assessment of both ischemic and bleeding risks, particularly in high-risk individuals. Recent advancements in stent technology and a deeper understanding of patient-specific risk profiles have led to significant advances in tailoring antiplatelet strategies. Current guidelines emphasize individualized approaches regarding the duration and intensity of the therapy. This review examines the evolution of antiplatelet treatment strategies in heart diseases, integrating evidence from pivotal studies to highlight current practices, while addressing considerations for special populations and optimal antithrombotic regimens following structural cardiac interventions. The development of novel agents, such as targeted antithrombotic therapy, and personalized therapeutic approaches continues to shape efforts to improve both efficacy and safety. Together, these advances support a more refined, patient-centered approach to antiplatelet therapy aimed at optimizing clinical outcomes in the context of a highly dynamic and evolving therapeutic landscape.