-
- Academic Editor
-
-
-
†These authors contributed equally.
Ultrafiltration (UF) is an alternative approach to diuretic therapy for the treatment of acute heart failure (AHF), but its optimal endpoint is unclear. This study explores using non-invasive ultrasonic cardiac output monitor (USCOM) to determine UF endpoints based on hemodynamic changes.
In this single-anonymized, randomized controlled trial, acute decompensated heart failure patients were randomly assigned to UF (U, n = 20) and USCOM+UF (UU, n = 20) groups at a ratio of 1:1. A mixed linear model was utilized to analyze repeated measurement data of hemodynamic indicators (primary endpoint) in the U and UU groups. A 30% or 50% decrease in B-type natriuretic peptide (BNP) concentrations relative to the baseline was established as the criteria for the UF endpoint success. Multivariate logistic regression was used to identify potential indicators within the USCOM that could have influenced the UF endpoint success. Receiver operating characteristic (ROC) curves were used to evaluate the value of the predictive model. Economic benefits, including treatment costs and hospitalization duration, were also assessed.
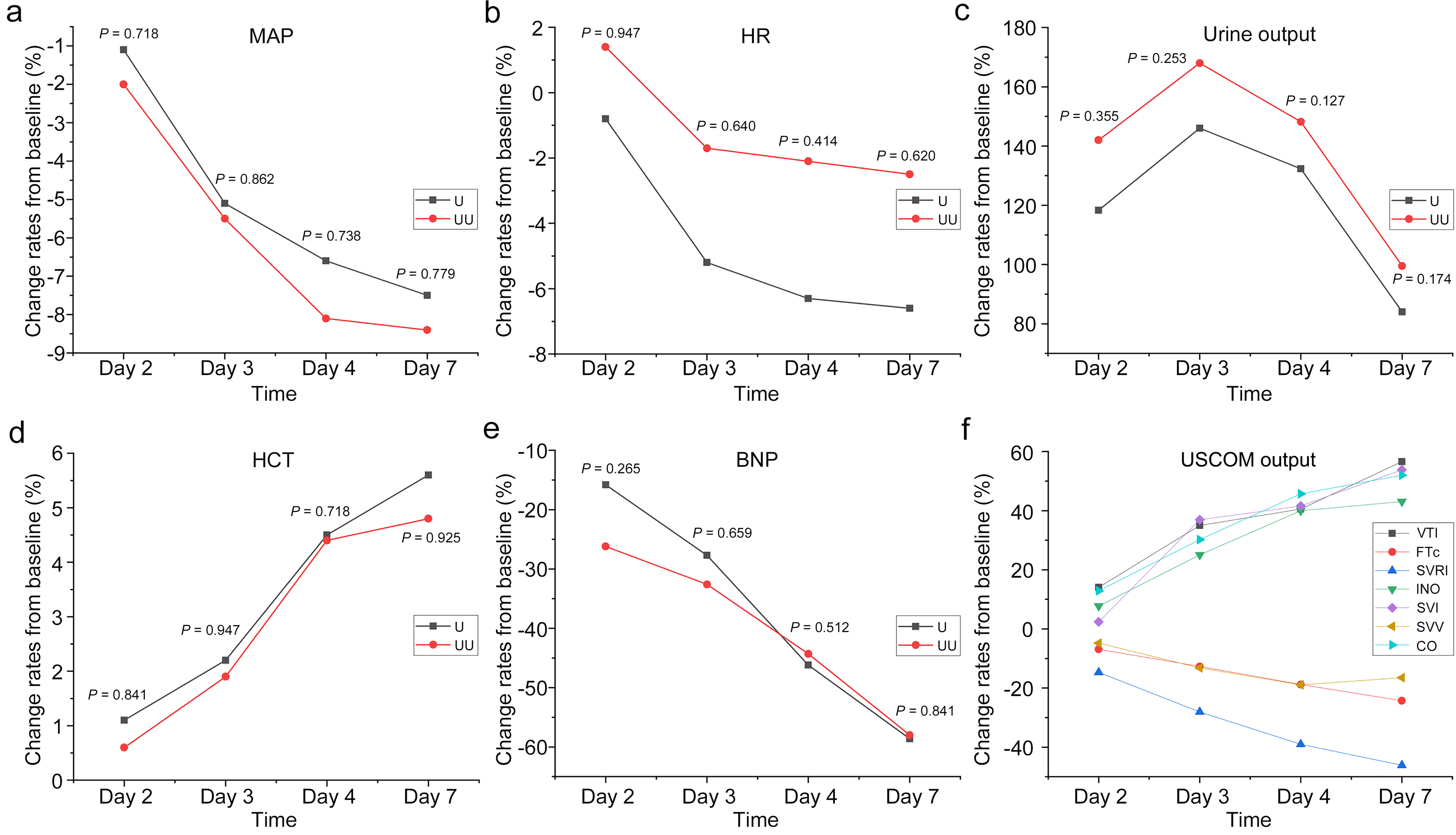
Change rates in mean arterial pressure, heart rate (HR), urine output, hematocrit, and BNP concentrations were similar between the U and UU groups over 7 days (all p > 0.05). On day 4, significant correlations were found between various USCOM parameters, including inotropy (INO), systemic vascular resistance index (SVRI), systemic vascular resistance, corrected flow time (FTc), velocity time integral, and the BNP of the UF parameters. Multivariate logistic regression revealed that INO and SVRI were correlated with a 30% reduction in BNP on day 4 compared to baseline, while FTc and HR were found to be independently associated with a 50% reduction in BNP on day 4 compared to baseline. The UF endpoint prediction formula for a 30% reduction in BNP was –2.462 + 0.028 × INO – 0.069 × SVRI, with sensitivities, specificities, and accuracies of 70%, 83%, and 75%, respectively. The UF endpoint prediction formula for a 50% reduction of BNP was –2.640 – 0.088 × FTc – 0.036 × HR, with sensitivities, specificities, and accuracies of 83%, 63.0%, and 72.5%, respectively. The addition of the USCOM significantly reduced treatment costs and hospitalization stay lengths.
Observing the USCOM using probability formulas served to determine appropriate UF endpoints during AHF treatments. UF combined with the USCOM can reduce the costs of UF and hospitalization.
NCT06533124, https://clinicaltrials.gov/study/NCT06533124?term=NCT06533124&rank=1.