- Academic Editor
-
-
-
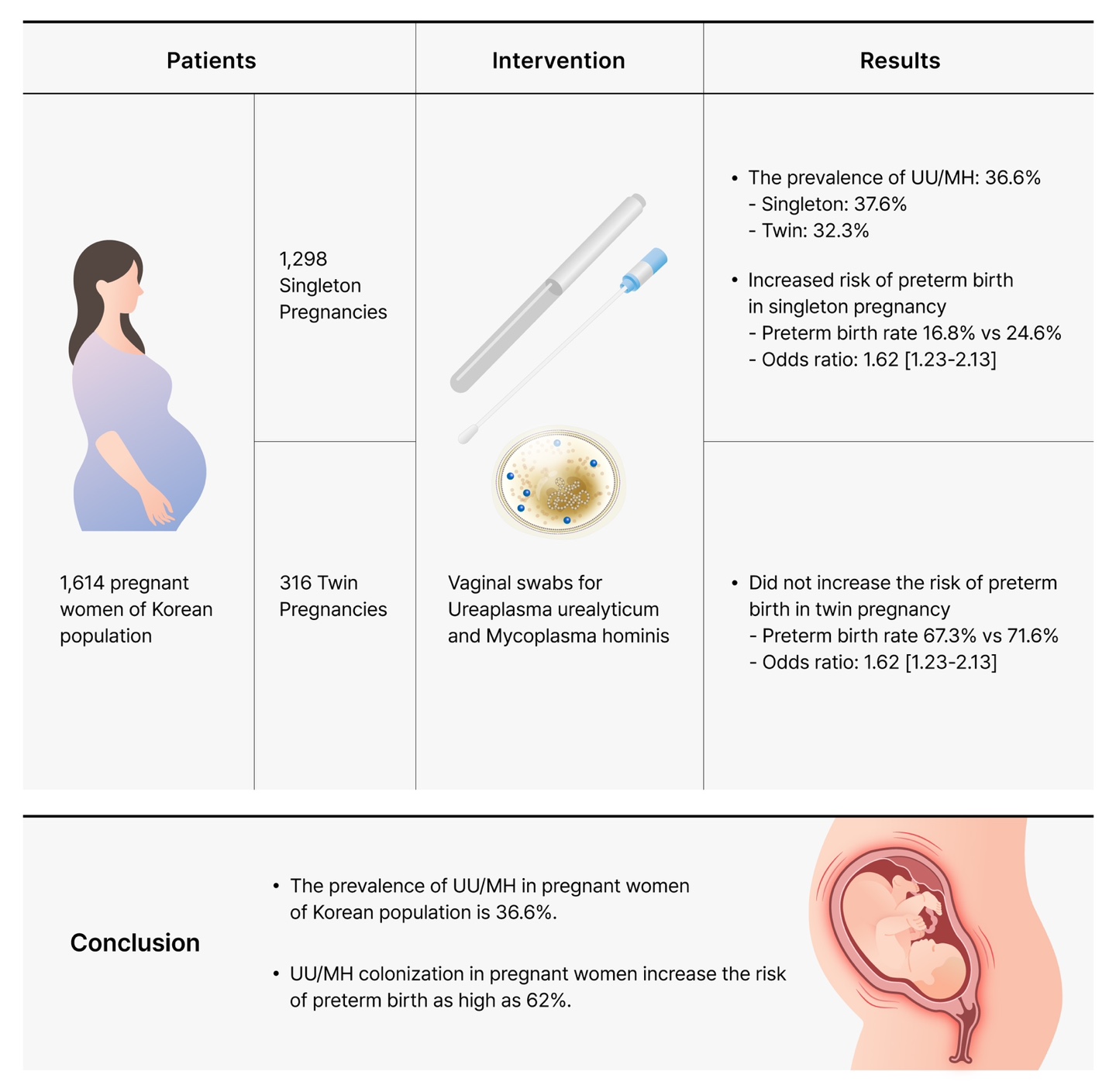
Colonization of the lower genital tract by Ureaplasma urealyticum (UU) and Mycoplasma hominis (MH) has been associated with adverse pregnancy outcomes, including preterm birth, but evidence remains inconsistent. This study aimed to assess the association between UU/MH colonization and preterm birth in singleton and twin pregnancies among Korean women.
This single-center observational study reviewed electronic medical records of pregnant women who attended the obstetrics clinic at Gyeongsang National University Changwon Hospital from January 2017 to December 2020. A total of 1614 pregnant women with available UU and MH test results were included. Both singleton (n = 1298) and twin pregnancies (n = 316) were analyzed. Vaginal swab samples were tested using culture methods, and obstetric outcome data were collected. Statistical analyses included Student's t-test and chi-square (χ2) test, with p-values calculated for statistical significance.
The prevalence of UU and/or MH colonization in the lower genital tract was 36.6% (n = 590/1614). In singleton pregnancies, UU/MH positive women had a higher incidence of preterm birth compared to the negative group (24.6% vs. 16.8%, p < 0.001), with an odds ratio (OR) of 1.62. Late preterm birth (34+0 to 36+6 weeks) constituted the majority of preterm births in singleton pregnancies. There was no significant difference in the proportion of small for gestational age (SGA) neonates between the two groups. In twin pregnancies, UU/MH colonization did not significantly affect preterm birth rates (p = 0.443). Bacterial vaginosis was significantly associated with UU/MH colonization (p < 0.001), but was not associated with increased risk of preterm birth (p = 0.189).
UU and MH colonization is prevalent in pregnant women in South Korea and is associated with an increased risk of preterm birth in singleton pregnancies. However, this association is not observed in twin pregnancies. Further multi-center studies utilizing both culture-based and polymerase chain reaction (PCR) methods are necessary to evaluate neonatal outcomes and to refine clinical management strategies.