-
- Academic Editor
-
-
-
†These authors contributed equally.
The birth outcomes of neonates born to mothers with polycystic ovary syndrome (PCOS) following intrauterine insemination (IUI) remain unclear, as do the correlations with pregravid maternal characteristics, thus warranting further investigation.
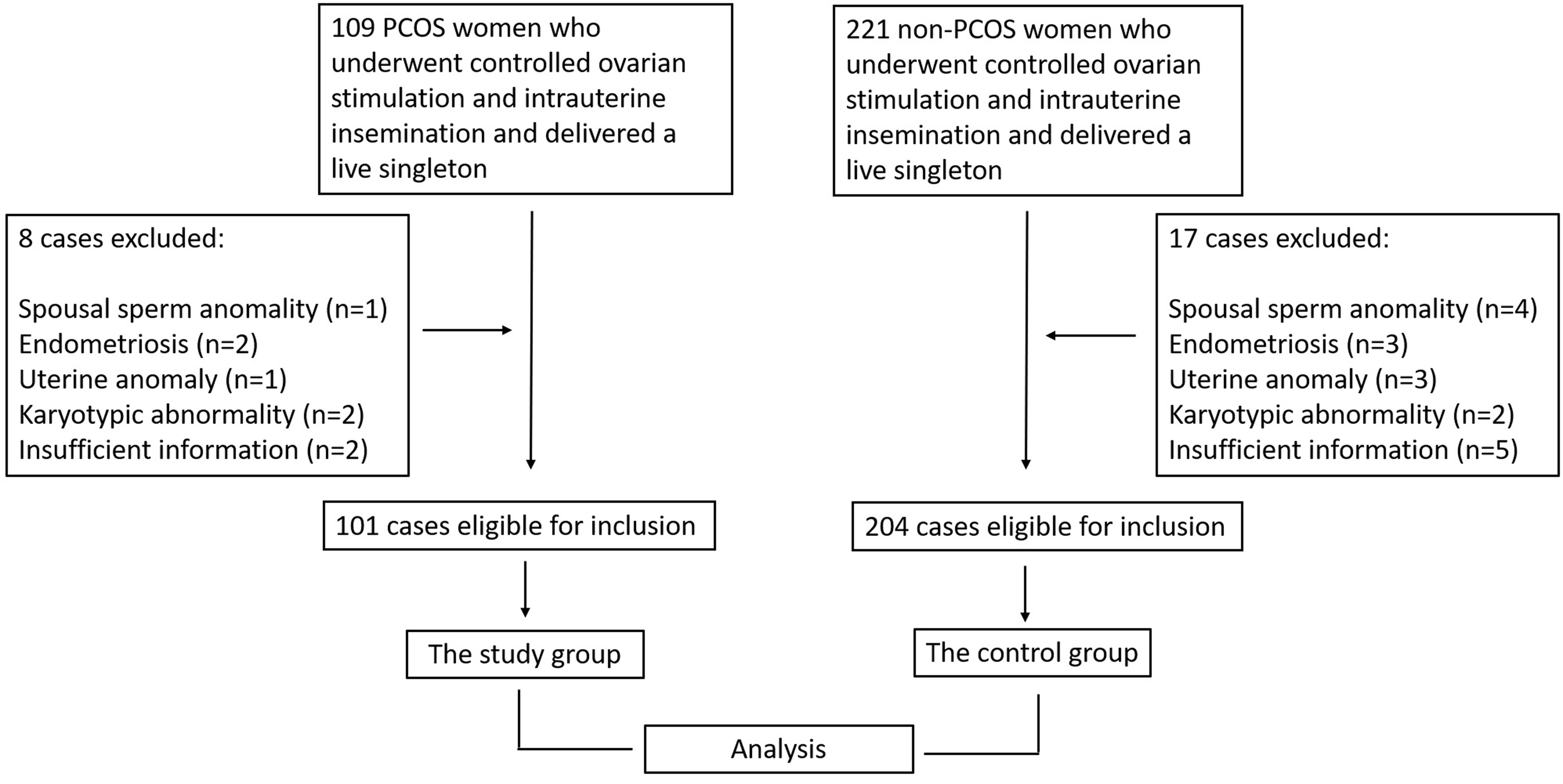
Data were collected on mothers with PCOS (PCOS group, n = 101), including the birth outcomes of their offspring. Mothers without PCOS (non-PCOS group, n = 204) and their offspring served as the control group. The two groups were analyzed for correlations between neonatal birth outcomes and pregravid maternal characteristics using univariate analysis, Spearman rank correlation, and logistic regression models.
In the PCOS group, maternal body mass index (BMI) was a positive predictor of neonatal complications, independent of confounding factors (unadjusted odds ratio [OR] = 1.28, p = 0.03; adjusted OR = 1.30, p = 0.04). However, no significant association was found between maternal BMI and neonatal complications in the non-PCOS group (unadjusted OR = 1.06, p = 0.34; adjusted OR = 1.02, p = 0.71). Compared to non-PCOS mothers, each one-unit increase in the BMI among PCOS mothers was associated with a 1.30-fold increased risk of adverse neonatal complications. Secondly, maternal BMI was a positive predictor of caesarean section delivery in the PCOS group, independent of confounding factors (unadjusted OR = 1.25, p = 0.006; adjusted OR = 1.28, p = 0.005). Maternal BMI was also a positive predictor for caesarean section delivery in the non-PCOS group, independent of confounding factors (unadjusted OR = 1.15, p = 0.004; adjusted OR = 1.14, p = 0.014). However, the adjusted OR in the PCOS group was higher than that observed in the non-PCOS group (OR = 1.28 vs. OR = 1.14).
The co-occurrence of elevated maternal BMI and PCOS may be associated with an elevated risk of neonatal complications and delivery by caesarean section following IUI. Mothers with PCOS are advised to maintain a healthy pregravid BMI in order to minimize the risk of adverse neonatal complications.