- Academic Editor
-
-
-
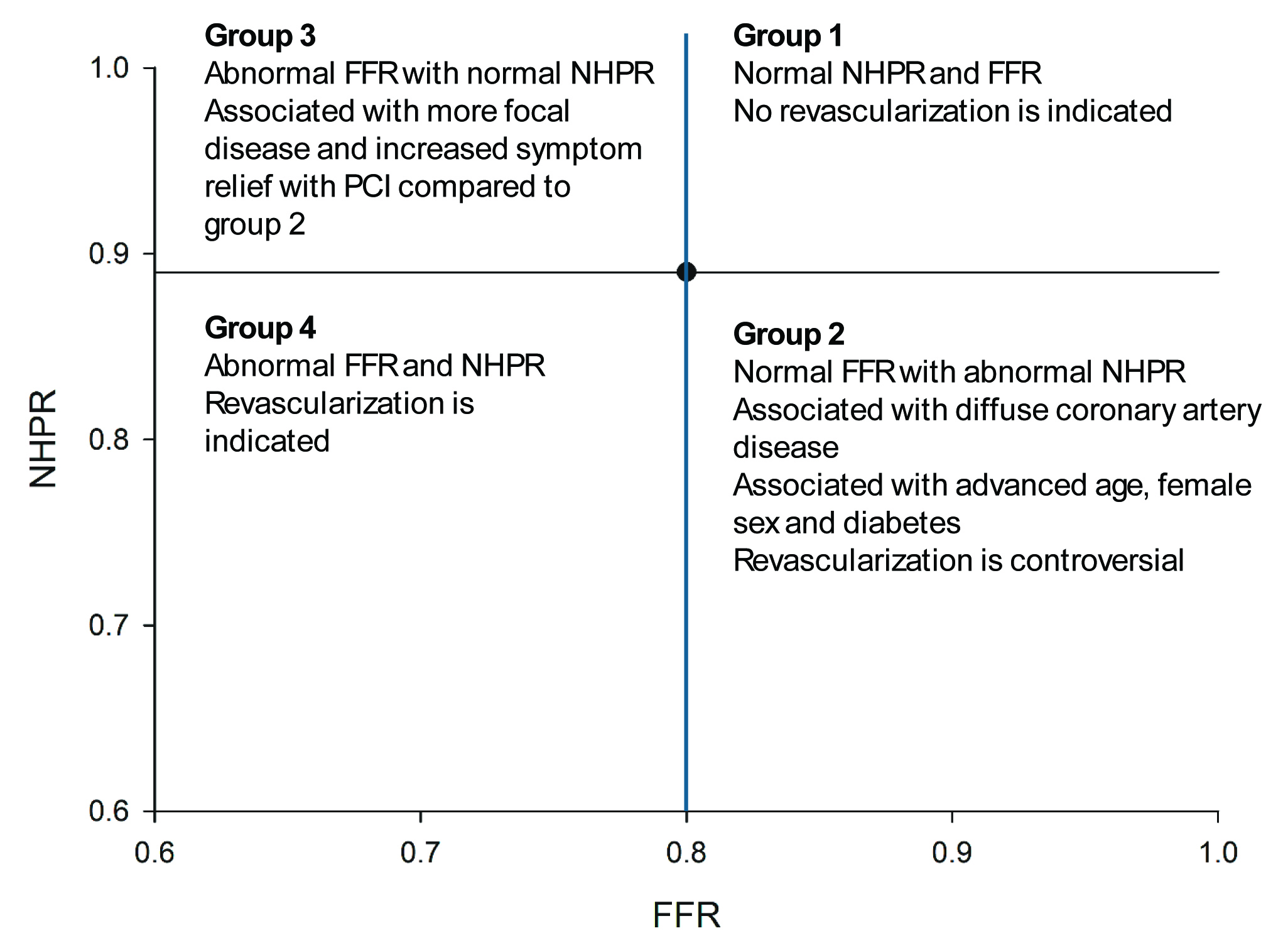
Invasive coronary angiography remains the gold standard for assessing and treating coronary artery disease (CAD). While the decision to intervene on a severely stenotic lesion in acute coronary syndrome (ACS) can be straightforward, assessing the potential benefits of treating an intermediate lesion, especially in patients with stable symptoms, often requires hemodynamic assessment or intravascular imaging. Fractional flow reserve (FFR) is a well-established invasive hemodynamic assessment that is the gold standard for determining the functional significance of intermediate lesions by analyzing the pressure loss across an area of stenosis during maximal hyperemia. The association between the use of FFR and improved clinical outcomes has been validated by numerous clinical trials, leading to societal guidelines for the use of FFR. Recently, invasive hemodynamic indices have been developed that do not require the induction of hyperemia. These non-hyperemic pressure ratios (NHPRs) include the resting full-cycle ratio (RFR), instantaneous wave-free ratio (iFR), diastolic hyperemia-free ratio (DFR), and diastolic pressure ratio (dPR). Clinical studies have suggested “discordance” in FFR and NHPRs in approximately 20% of patients with NHPR-/FFR+ being slightly more prevalent than NHPR+/FFR-. Discordance has been associated with clinical factors, including advanced age, female sex, presence of diabetes, and microvascular dysfunction. Data are inconsistent about whether deferral of revascularization is safe in patients with discordance; however, patients who are NHPR-/FFR+ are more likely to have focal than diffuse disease okand more likely to observe a symptomatic benefit from percutaneous coronary intervention (PCI). Nonetheless, large-scale studies are needed to improve understanding of this discordance, particularly in relation to clinical outcomes.