-
- Academic Editor
-
-
-
†These authors contributed equally.
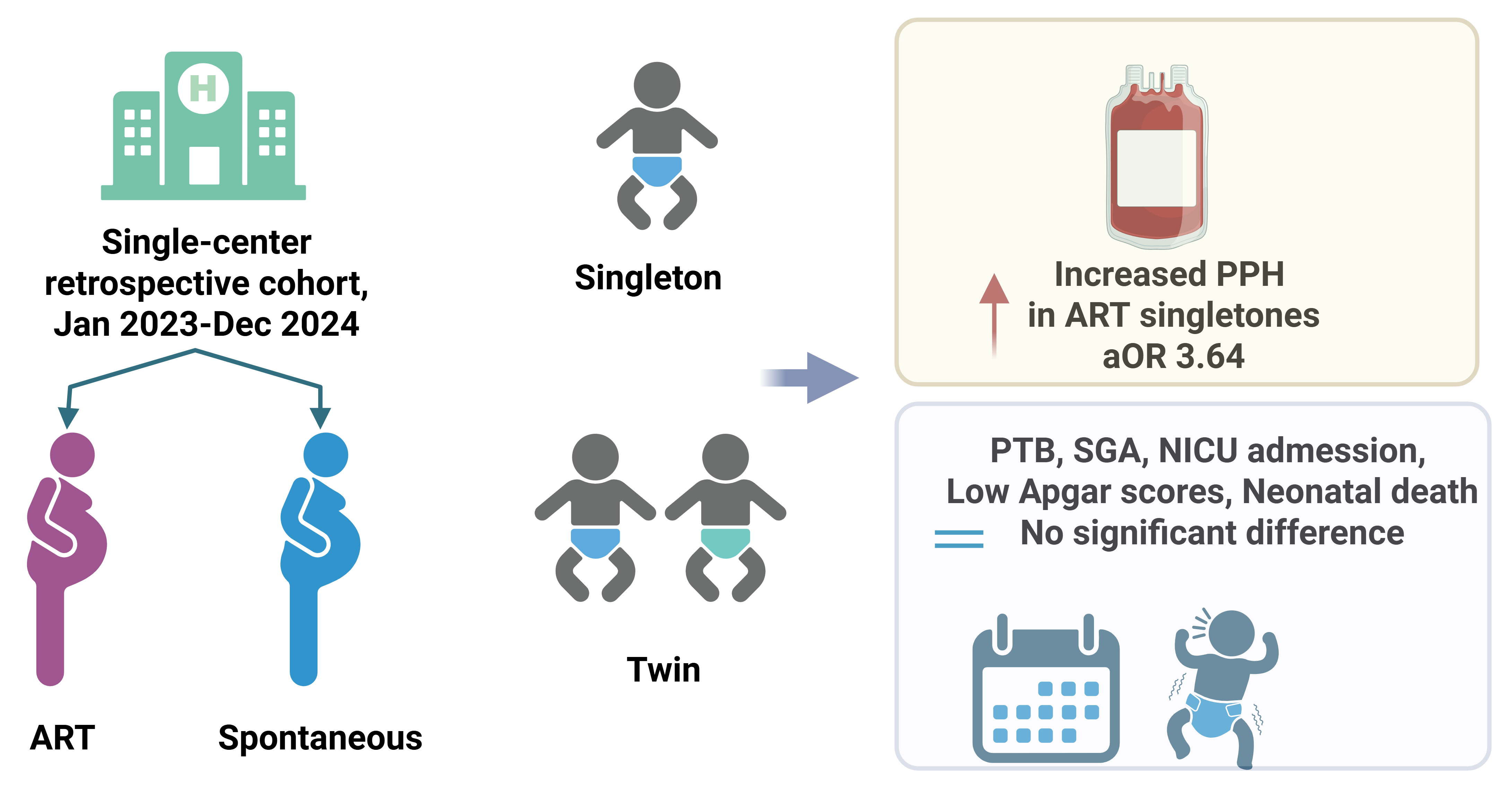
The global rise in pregnancies following assisted reproductive technology (ART) use has prompted ongoing evaluations into the impact of this technology on maternal and neonatal outcomes. Thus, this study aimed to compare outcomes between ART-conceived pregnancies and spontaneously conceived pregnancies, stratified by singleton and multiple pregnancies.
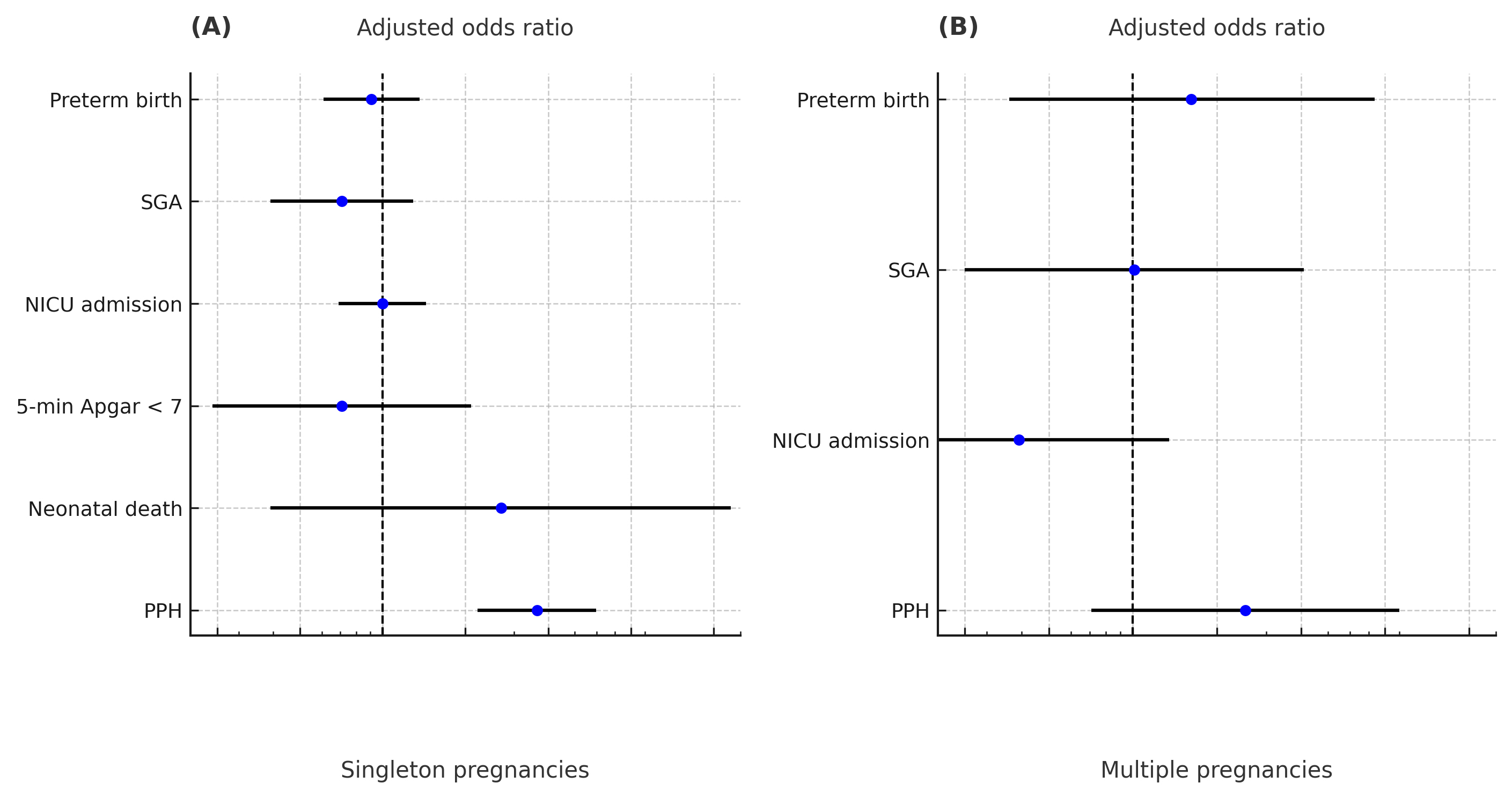
We conducted a single-center retrospective cohort study at Gyeongsang National University Changwon Hospital in South Korea, using the medical records of women who delivered between January 2023 and December 2024. A total of 921 pregnancies were included, comprising 816 singleton pregnancies and 105 multiple pregnancies. Maternal and neonatal baseline characteristics were compared between ART-mediated and spontaneous conceptions within each gestational category. Outcomes assessed included postpartum hemorrhage (PPH), preterm birth (PTB), small for gestational age (SGA), neonatal intensive care unit (NICU) admission, 5-minute Apgar score < 7, and neonatal death. Multivariable logistic regression was performed to estimate adjusted odds ratios (aORs), controlling for relevant confounders.
Most maternal and neonatal outcomes did not significantly differ between ART-mediated and spontaneous conceptions in either singleton or multiple pregnancies. There were no statistically significant differences in the rates of PTB, SGA, NICU admission, low 5-minute Apgar score, and neonatal death between the groups. However, there was a significantly higher incidence of PPH in ART-conceived singleton pregnancies (25.7% vs. 9.4%), which remained significant in the multivariable analysis (aOR: 3.64, 95% confidence interval (CI): 2.21–5.98; p < 0.001). No significant difference in PPH incidence was observed in the multiple pregnancy cohort.
Overall, most outcomes were comparable between ART-mediated and spontaneous conceptions. However, ART-conceived singleton pregnancies showed a significantly higher risk of PPH, even after adjusting for confounders. These findings underscore the need for heightened surveillance for PPH in ART-mediated singleton pregnancies, even in the absence of other risk factors.