- Academic Editor
†These authors contributed equally.
The global rise in pregnancies following assisted reproductive technology (ART) use has prompted ongoing evaluations into the impact of this technology on maternal and neonatal outcomes. Thus, this study aimed to compare outcomes between ART-conceived pregnancies and spontaneously conceived pregnancies, stratified by singleton and multiple pregnancies.
We conducted a single-center retrospective cohort study at Gyeongsang National University Changwon Hospital in South Korea, using the medical records of women who delivered between January 2023 and December 2024. A total of 921 pregnancies were included, comprising 816 singleton pregnancies and 105 multiple pregnancies. Maternal and neonatal baseline characteristics were compared between ART-mediated and spontaneous conceptions within each gestational category. Outcomes assessed included postpartum hemorrhage (PPH), preterm birth (PTB), small for gestational age (SGA), neonatal intensive care unit (NICU) admission, 5-minute Apgar score < 7, and neonatal death. Multivariable logistic regression was performed to estimate adjusted odds ratios (aORs), controlling for relevant confounders.
Most maternal and neonatal outcomes did not significantly differ between ART-mediated and spontaneous conceptions in either singleton or multiple pregnancies. There were no statistically significant differences in the rates of PTB, SGA, NICU admission, low 5-minute Apgar score, and neonatal death between the groups. However, there was a significantly higher incidence of PPH in ART-conceived singleton pregnancies (25.7% vs. 9.4%), which remained significant in the multivariable analysis (aOR: 3.64, 95% confidence interval (CI): 2.21–5.98; p < 0.001). No significant difference in PPH incidence was observed in the multiple pregnancy cohort.
Overall, most outcomes were comparable between ART-mediated and spontaneous conceptions. However, ART-conceived singleton pregnancies showed a significantly higher risk of PPH, even after adjusting for confounders. These findings underscore the need for heightened surveillance for PPH in ART-mediated singleton pregnancies, even in the absence of other risk factors.
Since the birth of the first in vitro fertilization (IVF) baby in 1978, the global use of assisted reproductive technology (ART) has grown substantially, with an estimated 13 million ART-conceived children born worldwide to date [1]. Currently, approximately one ART-conceived infant is born every 35 seconds, and ART births account for around 5–10% of all deliveries in some high-income countries [1]. This rapid growth has firmly established ART as a mainstream clinical tool for women and families requiring reproductive assistance. Given the increasing prevalence of ART, concerns have emerged about its safety, particularly the impact on maternal and neonatal health.
Various studies have linked ART-conceived pregnancies to increased risks of adverse perinatal and neonatal outcomes, including preterm birth (PTB), low birth weight or small for gestational age (SGA), cesarean delivery, postpartum hemorrhage (PPH), and hypertensive disorders [2, 3, 4]. However, some studies have found no significant differences in key perinatal outcomes between pregnancies conceived through ART and those conceived naturally [5, 6]. These conflicting findings likely reflect heterogeneity in study design, populations, and analytic approaches. Some studies focused exclusively on singletons [3, 7], whereas others included multiples without proper adjustment. Differences in controlling for maternal characteristics [2, 4], stratifying by plurality [2, 4, 8], and defining outcomes [3, 7] may have contributed to inconsistent results. These discrepancies raise questions about whether the observed risks are intrinsic to ART procedures, stem from underlying maternal characteristics, or are largely due to the higher incidence of multifetal gestation associated with ART [7, 8].
For evidence-based clinical counseling and management, it is necessary to clarify whether ART independently contributes to adverse perinatal and neonatal outcomes. To address this issue, we conducted a retrospective cohort analysis at a single institution to evaluate the impact of ART on perinatal and neonatal outcomes, including PTB, neonatal intensive care unit (NICU) admission, 5-minute Apgar score, birth weight, and PPH. Importantly, we stratified the analysis by singleton and multiple pregnancies to isolate the effects of ART from those of multifetal gestation, thereby providing clearer evidence for clinicians and patients.
This retrospective cohort study was conducted at Gyeongsang National University Changwon Hospital, a tertiary referral center in South Korea, a tertiary referral center in South Korea. The study population consisted of all women who delivered live-born infants at the institution between January 2023 and December 2024. Maternal and neonatal data were retrospectively collected from electronic medical records, which included maternal demographic and clinical characteristics, obstetric history (e.g., parity and multifetal gestation), and perinatal and neonatal outcomes. Multiple pregnancies were restricted to twin gestations; triplet or higher-order gestations were excluded as they represent a heterogeneous group with significantly different outcomes.
The study population was stratified by pregnancy type into singleton and multiple pregnancies. Within each stratum, women who conceived through medically assisted techniques, including IVF, intracytoplasmic sperm injection (ICSI), or frozen embryo transfer, were classified as the ART group. The non-ART group included pregnancies conceived spontaneously, without the use of ART methods such as IVF, ICSI, or embryo transfer. Some women in the non-ART group may have received infertility-related interventions such as ovulation induction or intrauterine insemination; however, as these interventions do not involve extracorporeal manipulation of gametes or embryos, they were not classified as the ART group according to international standards [9]. Moreover, multiple pregnancies were analyzed as a separate cohort due to their distinct clinical characteristics and population risk profiles when compared to those of singleton pregnancies.
The primary outcomes assessed in this study included PTB (
In addition to neonatal outcomes, selected maternal pregnancy outcomes (short
cervix, hypertensive disorders of pregnancy (HDP), and placenta previa) were
included in the analysis to evaluate their potential association with ART. A
short cervix was defined as a cervical length
Baseline maternal characteristics, obstetric complications, perinatal events,
and neonatal outcomes were compared between the ART and non-ART groups within
each gestational category (singleton and multiple pregnancies). Continuous
variables (e.g., maternal age, gestational age at delivery, and birth weight) are
presented as the mean
To assess the independent association between ART and each binary outcome,
multivariable logistic regression models were constructed. The outcomes included
PTB (
All statistical analyses were performed using Web-R ver. 3.4.1
(http://web-r.org), a web-based statistical analysis program. Additionally, R (R
Foundation for Statistical Computing, Vienna, Austria; version 4.5.1) was used to
reconstruct and verify results from the raw dataset. Statistical significance was
defined as a two-sided p-value
A total of 921 pregnancies were analyzed, comprising 816 singleton pregnancies (88.6%) and 105 multiple pregnancies (11.4%). Among singleton pregnancies, 175 pregnancies (21.4%) were conceived through ART, and 641 pregnancies (78.6%) were conceived spontaneously. Among multiple pregnancies, 78 pregnancies (74.3%) were conceived through ART, and 27 pregnancies (25.7%) occurred naturally. Maternal and neonatal characteristics grouped by ART exposure for singleton and multiple pregnancies are presented in Tables 1,2 respectively.
| Variables | ART (n = 175) | Non-ART (n = 641) | p-value | |
| Maternal characteristics | ||||
| Age (years) | 35.3 |
33.1 |
||
| Pre-pregnancy BMI (kg/m2) | 24.1 |
23.2 |
0.023 | |
| BMI at delivery (kg/m2) | 28.4 |
27.8 |
0.092 | |
| Primipara | 143 (81.7%) | 370 (57.7%) | ||
| Pregnancy & perinatal outcomes | ||||
| Short cervix | 38 (21.7%) | 76 (11.9%) | 0.001 | |
| Gestational diabetes mellitus | 28 (16.0%) | 81 (12.6%) | 0.335 | |
| Hypertensive disorders of pregnancy | 17 (9.7%) | 48 (7.5%) | 0.536 | |
| Cesarean delivery | 158 (90.3%) | 512 (79.9%) | 0.001 | |
| Placenta previa | 17 (9.7%) | 24 (3.7%) | ||
| Postpartum hemorrhage | 45 (25.7%) | 60 (9.4%) | ||
| Blood transfusion | 10 (5.7%) | 15 (2.3%) | 0.003 | |
| Intrauterine balloon tamponade | 40 (22.9%) | 55 (8.6%) | ||
| Uterine artery embolization | 2 (1.1%) | 3 (0.5%) | 0.288 | |
| Peripartum hysterectomy | 0 (0.0%) | 5 (0.8%) | 0.584 | |
| Admission to ICU | 0 (0.0%) | 4 (0.6%) | 0.584 | |
| Neonatal outcomes | ||||
| Gestational age at delivery (weeks) | 36.8 |
36.8 |
0.941 | |
| Female newborn | 85 (48.6%) | 328 (51.2%) | 0.601 | |
| Birth weight (g) | 2817.1 |
2773.2 |
0.619 | |
| Small for gestational age | 19 (10.9%) | 76 (11.9%) | 0.705 | |
| Apgar score at 1 minute | 7.3 |
7.4 |
0.367 | |
| Apgar score at 5 minutes | 8.5 |
8.5 |
0.547 | |
| Umbilical cord blood gas pH | 7.3 |
7.3 |
0.102 | |
| Umbilical cord blood base excess (mmol/L) | –4.0 |
–3.7 |
0.187 | |
| Admission to NICU | 62 (35.6%) | 224 (35.0%) | 0.722 | |
| Duration of NICU stay (days) | 20.2 |
26.8 |
0.052 | |
| Respiratory support | 67 (38.3%) | 249 (39.0%) | 0.825 | |
| Fetal malformation | 32 (18.3%) | 123 (19.2%) | 0.845 | |
| Neonatal death | 3 (1.7%) | 4 (0.6%) | 0.172 | |
Data are presented as the mean
| Variables | ART (n = 78) | Non-ART (n = 27) | p-value | |
| Maternal characteristics | ||||
| Age (years) | 34.7 |
31.8 |
||
| Pre-pregnancy BMI (kg/m2) | 23.5 |
22.6 |
0.217 | |
| BMI at delivery (kg/m2) | 29.3 |
28.4 |
0.342 | |
| Primipara | 65 (83.3%) | 17 (63.0%) | 0.027 | |
| DCDA twins | 63 (80.8%) | 19 (70.4%) | 0.287 | |
| MCDA twins | 8 (10.3%) | 8 (29.6%) | 0.027 | |
| Pregnancy & perinatal outcomes | ||||
| Short cervix | 16 (20.5%) | 2 (7.4%) | 0.148 | |
| Gestational diabetes mellitus | 13 (16.7%) | 3 (11.1%) | 0.757 | |
| Hypertensive disorders of pregnancy | 7 (9.0%) | 3 (11.1%) | 0.715 | |
| Cesarean delivery | 77 (98.7%) | 25 (92.6%) | 0.162 | |
| Placenta previa | 1 (1.3%) | 1 (3.7%) | 0.450 | |
| Postpartum hemorrhage | 22 (28.2%) | 6 (22.2%) | 0.545 | |
| Blood transfusion | 7 (9.0%) | 3 (11.1%) | 0.715 | |
| Intrauterine balloon tamponade | 20 (25.6%) | 5 (18.5%) | 0.454 | |
| Uterine artery embolization | 3 (3.8%) | 2 (7.4%) | 0.601 | |
| Peripartum hysterectomy | 1 (1.3%) | 1 (3.7%) | 0.450 | |
| Admission to ICU | 1 (1.3%) | 1 (3.7%) | 0.450 | |
| Neonatal outcomes | ||||
| Gestational age at delivery (weeks) | 35.2 |
35.1 |
0.846 | |
| Female newborn | 39 (50.0%) | 15 (53.6%) | 0.746 | |
| Birth weight (g) | 2319.9 |
2249.6 |
0.448 | |
| Small for gestational age | 11 (14.1%) | 4 (14.3%) | 1.000 | |
| Apgar score at 1 minute | 7.2 |
7.0 |
0.380 | |
| Apgar score at 5 minutes | 8.4 |
8.2 |
0.339 | |
| Umbilical cord blood gas pH | 7.3 |
7.31 |
0.656 | |
| Umbilical cord blood base Excess (mmol/L) | –4.3 |
–4.9 |
0.241 | |
| Admission to NICU | 32 (41.0%) | 14 (50.0%) | 0.411 | |
| Duration of NICU stay (days) | 18.2 |
21.5 |
0.651 | |
| Respiratory support | 30 (38.5%) | 11 (39.3%) | 0.939 | |
| Fetal malformation | 10 (12.8%) | 3 (10.7%) | 1.000 | |
| Neonatal death | 2 (2.6%) | 1 (3.6%) | 1.000 | |
Data are presented as the mean
Women with ART-conceived singleton pregnancies were significantly older (35.3
In terms of delivery outcomes, PPH occurred more frequently in ART-conceived
singleton pregnancies (25.7% vs. 9.4%, p
Neonatal outcomes, including gestational age at delivery (36.8
In the multiple pregnancy cohort, women who conceived via ART were significantly
older (34.7
Cesarean section was the predominant mode of delivery in both groups, with no statistically significant difference (98.7% vs. 92.6%, p = 0.162). PPH was more frequent in the ART group but not statistically significant (28.2% vs. 22.2%, p = 0.545). Similarly, intrauterine balloon tamponade, blood transfusion, and ICU admission did not differ significantly.
Neonatal outcomes were largely comparable between ART and non-ART multiple
pregnancies. The mean gestational age at delivery (35.2
Multivariable logistic regression was performed to evaluate whether ART could independently predict adverse outcomes, adjusting for maternal age, pre-pregnancy BMI, parity, GDM, HDP, gestational age at delivery (excluded from the PTB model), and mode of delivery (Fig. 1 and Table 3).
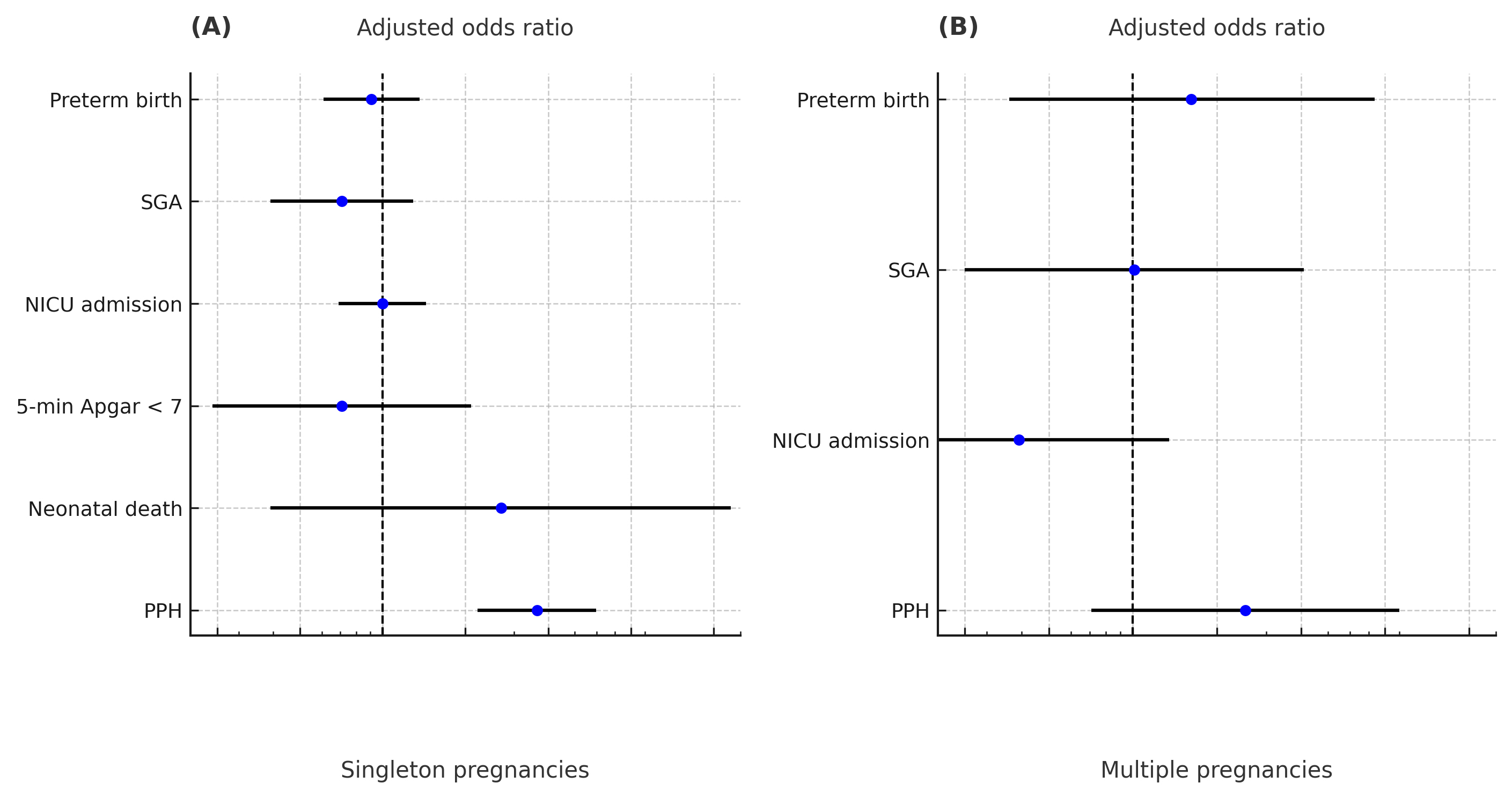 Fig. 1.
Fig. 1.
Forest plot showing the association between ART and adverse obstetric and neonatal outcomes in (A) singleton and (B) multiple pregnancies. The vertical dashed line represents an odds ratio of 1. Adjusted odds ratios (aORs, blue dot) and 95% confidence intervals (CIs, error bars) were calculated by multivariable logistic regression with adjustment for maternal age, pre-pregnancy BMI, parity, GDM, HDP, gestational age at delivery, and mode of delivery. Gestational age at delivery was excluded from the PTB model. SGA, small for gestational age; PPH, postpartum hemorrhage; GDM, gestational diabetes mellitus; HDP, hypertensive disorders of pregnancy; PTB, preterm birth.
| Outcomes | Singleton aOR (95% CI) | p-value | Multiple aOR (95% CI) | p-value |
| Preterm birth ( |
0.91 (0.61–1.36) | 0.647 | 1.62 (0.36–7.35) | 0.533 |
| SGA | 0.71 (0.39–1.29) | 0.256 | 1.01 (0.25–4.10) | 0.993 |
| NICU admission | 1.00 (0.69–1.44) | 1.000 | 0.39 (0.11–1.35) | 0.136 |
| 5-minute Apgar score |
0.71 (0.24–2.10) | 0.533 | — | — |
| Neonatal death | 2.70 (0.39–18.52) | 0.312 | — | — |
| PPH | 3.64 (2.21–5.98) | 2.53 (0.71–9.02) | 0.152 |
Multivariable logistic regression models were adjusted for maternal age, pre-pregnancy BMI, parity, GDM, HDP, gestational age at delivery (excluded in the PTB model), and mode of delivery.
Adjusted analyses for 5-minute Apgar score
In singleton pregnancies, ART was significantly associated with an increased
risk of PPH (aOR: 3.64, 95% CI: 2.21–5.98, p
In multiple pregnancies, none of the outcomes showed a statistically significant association with ART. Additionally, aORs for PTB (aOR: 1.62, 95% CI: 0.36–7.35, p = 0.533), SGA (aOR: 1.01, 95% CI: 0.25–4.10, p = 0.993), NICU admission (aOR: 0.39, 95% CI: 0.11–1.35, p = 0.136), and PPH (aOR: 2.53, 95% CI: 0.71–9.02, p = 0.152) were all found to be non-significant.
Logistic regression was not performed for 5-minute Apgar score
This study evaluated the obstetric, perinatal, and short-term neonatal outcomes of pregnancies conceived via ART compared to those conceived spontaneously, with analyses stratified by singleton and multiple pregnancies. Overall, most obstetric complications and neonatal outcomes were comparable between the ART and non-ART groups. However, ART-conceived singleton pregnancies demonstrated higher rates of short cervix and PPH. In comparison to women in the non-ART group, those in the ART group were also older and more likely to be nulliparous. In the multiple pregnancy cohort, ART pregnancies showed a lower proportion of MCDA twins. Multivariable logistic regression revealed that ART was not independently associated with adverse short-term perinatal or neonatal outcomes, except for an increased risk of PPH in singleton pregnancies.
Previous studies have reported elevated risks of obstetric and perinatal complications associated with ART. Chen et al. [4] demonstrated significantly higher rates of PTB, NICU admission, low birth weight, and PPH in the ART group compared to the spontaneously conceived group, with differences persisting even after adjusting for confounders. Similarly, a single-center study by Marsubrin et al. [2] observed higher incidences of PTB, respiratory distress syndrome, and NICU admission, along with longer hospitalization, among ART-conceived neonates compared to those conceived naturally.
In contrast, this study did not show significant differences in PTB, low birth weight, NICU admission, and Apgar score between the ART and non-ART groups, particularly in the analysis of singleton pregnancies. Apart from the elevated risk of PPH and short cervix, ART was not identified as an independent risk factor for short-term perinatal morbidity. These findings remained consistent in sensitivity analyses excluding borderline gestational age cases, supporting the robustness of the results. These contrasting results may be attributed to key differences in study design and population characteristics. In both prior studies, the ART group included a higher proportion of multiple gestations, a well-established risk factor for adverse neonatal outcomes. For instance, Marsubrin et al. [2] reported that approximately 38% of ART pregnancies were multifetal, which may have contributed to the higher rates of preterm birth and NICU admission observed in that study. In this analysis, we stratified outcomes by plurality and focused primarily on singleton pregnancies, thereby minimizing the confounding impact of multiple gestation.
While Chen et al. [4] used multicenter data and Marsubrin et al. [2] conducted a single-center study, both studies offered limited detail on how maternal variables and outcome definitions were standardized across their datasets. In contrast, this study utilized electronic medical record data from a single tertiary institution, where definitions and measurement protocols were applied consistently. We conducted multivariable logistic regression controlling for maternal age, BMI, parity, and major medical conditions such as hypertension and diabetes, allowing more rigorous adjustment for potential confounders. These differences suggest that the risks associated with ART may vary depending on maternal characteristics, the clinical environment, and how outcomes are defined and analyzed. The present finding supports the view that ART may not independently contribute to short-term perinatal morbidity when appropriately adjusted and evaluated within a contemporary and controlled clinical setting.
The findings reflect limitations in earlier studies, many of which did not sufficiently adjust for critical confounding factors such as maternal age, multifetal gestation, and baseline comorbidities. In a sibling cohort study comparing ART and naturally conceived pregnancies, Romundstad et al. [16] reported that differences in birth weight and preterm delivery largely disappeared or lost statistical significance after controlling for maternal demographics and health factors. Similarly, a population-based analysis in the United States [17] found that although ART pregnancies were initially associated with higher rates of PTB and low birth weight, these elevated risks were attenuated when focusing on singleton gestations and adjusting for maternal characteristics.
Pandey et al. [3] reported increased perinatal risks in ART-conceived singleton births in a meta-analysis. However, these findings may partially reflect earlier ART protocols, such as frequent multiple embryo transfers and less advanced embryo culture methods. Differences in study populations or unmeasured residual confounding related to subfertility may also contribute to these discrepancies. In contrast, this study is based on recent clinical data and thus reflects contemporary ART practice, such as elective single embryo transfer and improved obstetric surveillance [18]. The consistent clinical environment of this single-center cohort may have minimized variability and confounding, though at the cost of generalizability and reduced power to detect small effects. Overall, these contrasting findings reflect improvements in ART safety over time, emphasizing the need to re-evaluate ART-associated risks in the context of modern practice through updated, large-scale studies.
Despite the overall reassuring results, this study found a significantly higher rate of PPH among ART-conceived singleton pregnancies. This finding is consistent with prior research identifying ART as a risk factor for PPH and related interventions such as blood transfusion [19]. This elevated risk is thought to result from multiple pathophysiological mechanisms, such as abnormal placental implantation, impaired vascular development due to hormonal stimulation, and uterine atony. In this cohort, the incidence of PPH in the ART group was high at 25.7% compared to 9.4% in the non-ART group. ART pregnancies also required more interventions for bleeding control, including intrauterine balloon tamponade and blood transfusion.
Although previous studies have reported PPH rates of approximately 11.1–19.2%
in ART pregnancies [4, 19], the incidence observed in the present study’s
ART-conceived singleton cohort was comparatively higher (25.7%). This may
reflect the high-risk nature of the study population and differences in
diagnostic criteria and surveillance methods. In this study, PPH was defined as
clinically significant bleeding or an estimated blood loss of
Another notable finding was the increased incidence of short cervical length in singleton pregnancies conceived via ART. This may reflect procedural factors (e.g., cervical instrumentation during embryo transfer or prior uterine procedures), as well as underlying infertility-related conditions (e.g., congenital uterine anomalies, polycystic ovary syndrome, or previous surgical curettage), which are more prevalent in ART populations [21, 22]. These conditions are independently associated with cervical insufficiency and PTB. Therefore, routine mid-trimester cervical length screening should be considered in ART-conceived singleton pregnancies regardless of obstetric history. Early detection can facilitate timely interventions such as progesterone therapy or cervical cerclage when indicated.
Taken together, the present findings are reassuring for women conceiving via ART. With proper management, ART pregnancies may achieve perinatal outcomes comparable to those of spontaneous conceptions. Importantly, ART itself does not appear to be an intrinsic risk factor for most adverse outcomes; rather, associated risks often stem from modifiable contributors such as multifetal gestation and maternal comorbidities. In particular, preventing multiple pregnancies is a key strategy in mitigating ART-related risks. Elective single embryo transfer has been shown to reduce the incidence of twin gestations without compromising live birth rates [23]. Minimizing iatrogenic multiple births allows clinicians to significantly reduce PTB and other complications linked to ART. Additionally, optimizing maternal health, such as managing chronic hypertension or diabetes, during ART pregnancies can improve outcomes and address negative perceptions about infertility treatments. Current evidence suggests that ART, when practiced according to modern protocols, does not inherently jeopardize perinatal health. This information may help reduce patient anxiety and promote more informed and confident decision-making.
This study has several limitations. It was conducted retrospectively at a single tertiary medical center, with a modest sample size and a two-year inclusion period. These factors may have limited the ability of the study to detect rare events such as perinatal mortality or long-term neonatal sequelae. In particular, the very small number of neonatal death events, especially in the multiple pregnancy cohort, may have limited the statistical power to detect meaningful differences for this outcome. Additionally, we were unable to compare outcomes across different ART modalities (e.g., IVF vs. ICSI) or fully control for all potential confounders, such as specific infertility diagnoses, socioeconomic status, and maternal lifestyle factors. These unmeasured variables may have influenced the observed associations and should be considered when interpreting the findings. ART-related factors such as ovarian stimulation protocols, embryo transfer methods, and infertility etiology could not be assessed in this study due to lack of available information. These variables may influence outcomes such as postpartum hemorrhage and cervical length and warrant further investigation in studies with more detailed ART data. As an observational study, causality could not be established, and residual confounding from unmeasured variables may persist despite adjustment.
Nevertheless, this study has certain methodological strengths. Notably, we analyzed singleton and multiple pregnancies separately, allowing for a more accurate estimation of the effects of ART independent of plurality—a critical confounder in ART research. By stratifying analyses in this manner, we reduced the bias from the overrepresentation of multifetal gestation in ART populations and avoided misleading comparisons between heterogeneous pregnancy types. Moreover, all data were obtained from a single institution with standardized clinical protocols, ensuring consistency in diagnosis, management, and documentation. We also used multivariable logistic regression models to adjust for key maternal and obstetric factors, enhancing the internal validity of our findings. Moving forward, larger multicenter studies with long-term follow-up are needed to assess delayed or subtle outcomes in ART-conceived offspring and better evaluate the safety profile of different ART modalities. Such studies will support more robust, evidence-based counseling and enhance care for individuals pursuing ART.
In conclusion, this study demonstrated that conception via ART was not independently associated with increased risks of major perinatal or neonatal complications after adjusting for maternal and obstetric confounders. The elevated risks traditionally attributed to ART appeared to stem primarily from multifetal gestation and maternal health factors, rather than ART procedures. The findings underscore the importance of targeted strategies to mitigate risks in ART pregnancies—specifically, the prevention of multifetal gestation and proactive management of maternal comorbidities. By implementing such strategies, the outcomes of ART pregnancies can approach those of spontaneously conceived pregnancies. Continued emphasis on promoting singleton pregnancies and optimizing perinatal care is essential for improving the safety and success of ART. Future research should focus on long-term neonatal outcomes and the comparative safety of specific ART modalities to further inform clinical practice and patient counseling.
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
JEP designed the research study. JY, HCJ, and JEP performed the research. JCB contributed to data acquisition and part of the data analysis process. JY, HCJ, and JEP analyzed the data. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors participated in the work and agreed to be accountable for all aspects of the work.
This cohort study was approved by the Ethics Committee of Gyeongsang National University Changwon Hospital (IRB number: GNUCH 2025-07-023) and was conducted according to the principles of the Declaration of Helsinki. Informed consent was waived by the Ethics Committee because of the use of retrospective and deidentified data.
The authors would like to thank the staff and patients of Gyeongsang National University Changwon Hospital for their cooperation and support.
This research received no external funding.
The authors declare no conflict of interest.
The authors declare that AI-assisted technologies, specifically OpenAI’s ChatGPT, were used to support the writing process of this manuscript. The tool was employed solely for language refinement and grammar correction. All intellectual contributions, data interpretation, and conclusions presented in this manuscript were made by the authors. The use of AI was strictly for enhancing the manuscript’s presentation and did not influence the scientific content or the integrity of the research. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/CEOG45477.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
