- Academic Editor
-
-
-
Uterine fibroids represent the most frequent benign tumor of the uterus in women of reproductive age. They may be discovered accidentally or can be symptomatic. They pose substantial intraoperative challenges due to the increased risk of bleeding. Despite the rising incidence of fibroids during pregnancy, there is no consensus on the optimal strategy to minimize bleeding during cesarean section (C-section). This review aims to synthesize and critically examine the current evidence on medical, surgical, interventional, and innovative experimental approaches for reducing intraoperative bleeding during C-section. We aim to provide an up-to-date, evidence-based overview to guide clinical decision-making and highlight a gap in knowledge for future research.
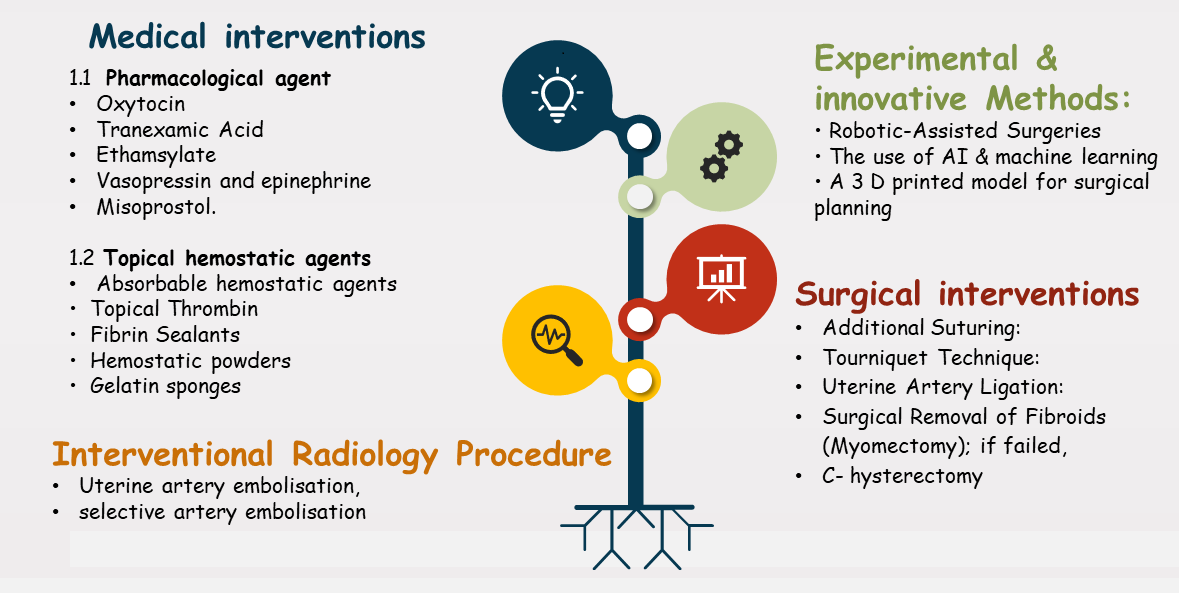
Three electronic databases were searched using the keywords: “fibroids”, “intraoperative bleeding”, “cesarean myomectomy”, and “pregnancy”, following the inclusion criteria set. Eligible studies were analyzed, and the extracted data were examined for duplication before inclusion in the review. Four major categories of interventions were identified for reducing intraoperative bleeding: medical, surgical, innovative, and experimental methods. For each technique, relevant data were recorded and synthesized into tables.
Medical techniques were effective, although they had side effects, and their efficacy could be enhanced when used in combination. Surgical techniques proved effective when medical approaches failed, especially in complicated cases. Emerging modalities show promising efficacy with minimal impact on future fertility, but they need further validation.
A personalized, multidisciplinary approach is needed to effectively reduce and manage intraoperative bleeding. Current practice should shift toward risk stratification using predictive tools to estimate bleeding preoperatively. Surgical teams should develop personalized bleeding-control strategies incorporating appropriate pharmacological agents. Future research should examine the integration of artificial intelligence (AI)-based risk modeling and three-dimensional (3D)-printed surgical planning to optimize maternal safety while preserving fertility.