- Academic Editors
-
-
-
†These authors contributed equally.
This study intended to investigate the correlation between insulin resistance (IR) and coagulation parameters in women with polycystic ovary syndrome (PCOS) and their effects on infertility.
We retrospectively included 380 PCOS patients and 143 healthy controls between January 2018 and January 2021. Clinical data, including age; body mass index; white blood cell (WBC), neutrophil (NE), lymphocyte (Lym), and platelet (PLT) counts; and D-dimer, plasma sex hormone, fasting blood sugar, and fasting insulin levels, were collected. The relationship between these markers and PCOS was assessed.
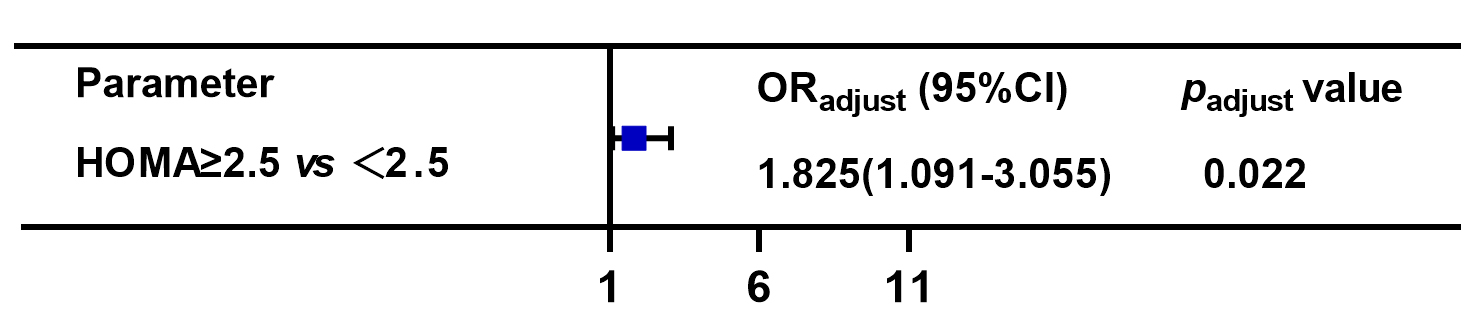
Elevated homeostatic model assessment of insulin resistance score was independently related to infertility in women with PCOS (odds ratio [OR] = 1.825, 95% confidence interval [CI]: 1.091–3.055, p = 0.022). WBC (7.29 [5.99–8.59] vs. 6.25 [5.33–7.40], p < 0.001), NE (3.91 [3.22–4.98] vs. 3.36 [2.62–4.51], p = 0.001), PLT (276 [244.5–317.5] vs. 251.5 [219.25–281.5], p < 0.001), and Lym (2.51 [2.02–3.11] vs. 2.08 [1.85–2.53], p < 0.001) counts, and D-dimer levels (0.22 [0.15–0.42] vs. 0.20 [0.12–0.31], p = 0.023) in the serum were markedly higher in PCOS patients with IR. Furthermore, multivariate logistic regression analysis revealed that increased serum PLT count (OR = 3.066, 95% CI: 1.052–8.939, p = 0.040) and BMI (OR = 5.06, 95% CI: 1.166–21.963, p = 0.030) were independently correlated with the risk of IR in PCOS patients. Moreover, increased PLT count was independently related to infertility (OR = 3.380, 95% CI: 1.272‒8.982, p = 0.015).
Elevated PLT count serve as an independent responsible role for infertility in PCOS women with IR, which indicate that PLT count might be a potential predictive marker for infertility in PCOS women with IR.