1 Department of Gynaecology, St. Michael’s Hospital, BS2 8EG Bristol, UK
2 Department of Gynaecological Oncology, Westmead Hospital, 2145 Sydney, NSW, Australia
3 Department of Gynaecological Oncology, Royal Surrey NHS Foundation Trust, GU2 7XX Surrey, UK
Abstract
Objectives: The incidence of endometrial cancer (EC) is rising largely due to the increasing levels of obesity along with an ageing population. This has led to an increase in the incidence of premenopausal women with EC. 5% of cases are in patients less than 40 years old, 70% of which are nulliparous at diagnosis. Therefore, fertility considerations must be taken into account when managing these patients. The objectives of this review are to present the fertility-sparing management options available. Mechanism: A detailed computerized literature search of PubMed and MEDLINE up to 1st June 2022 was carried out in order to survey the evidence for fertility-sparing treatment. Studies including patients with endometrial hyperplasia and early-stage EC undergoing fertility-sparing management were included. Findings in Brief: Progestin acts by downregulating oestrogen receptors, thereby suppressing endometrial growth. Oral progestins and the levonorgestrel-releasing intrauterine system (IUS) have therefore been used as non-surgical hormonal treatment for EC. Megestrol acetate (MA) has been shown to produce the highest remission rates compared to other progestins in a systematic review and meta-analysis, but medroxyprogesterone acetate exhibited lower recurrence rates. The IUS for atypical hyperplasia (AH) and EC showed that the majority of patients responded by 3 months’ use. A minimum duration of hormonal treatment for AH and EC of 6 months has been advocated, based on randomised studies showing greater efficacy when compared to 3 months treatment. A meta-analysis and systematic review assessing the efficacy of both oral and intra-uterine progestins showed a higher pooled complete response (CR) than with IUS alone. Metformin, gonadotrophin-releasing hormone agonists and weight loss have also been added to progestin regimes with variable results on EC regression. Hysteroscopic resection allows for targeted excision of early-stage EC, but with the risk of perforation and so this has not been recommended by the British Gynaecological Cancer Society or the European Society of Gynaecological Oncology. Assisted reproduction treatment (ART) may be the quickest way to achieve pregnancy once CR is achieved. Pregnancy rates have varied from 32–100%, with live birth rates varying from 17.9–43.8%. Conclusions: EC incidence is on the increase in the premenopausal population along with obesity rates and the average first age of parenthood. Fertility-sparing management of EC should be considered for women where fertility is desired.
Keywords
- endometrial cancer
- fertility-sparing treatment
- morbid obesity
- fertility conservation
The incidence of endometrial cancer (EC) is rising largely due to the increasing levels of obesity along with an ageing population [1]. Type I endometrioid carcinoma is driven by oestrogen excess which occurs in obesity due to the peripheral conversion of adipose tissue to oestrogen. This leads to the unopposed stimulation and growth of the endometrium which in turn increases the risk of endometrial hyperplasia and EC. Up to 57% of newly diagnosed cases of EC are due to obesity [2]. This is of enormous concern with obesity levels in Europe projected to increase to 43% by 2025 [3].
EC mainly affects postmenopausal women and the average age at diagnosis is 60 years old [4]. However, the rise in obesity levels has led to an increase in the incidence of premenopausal women with EC. 5% of cases are in patients less than 40 years old [5, 6], 70% of which are nulliparous at diagnosis [7]. This coupled with an increase in the average age of childbearing means that more women will be affected with EC before having started or completed their family. Therefore, fertility considerations must be taken into account when counselling and managing these patients. Letourneau et al. [8] surveyed patients after treatment for EC and fertility was reported as one of the most important factors in determining quality of life.
The current gold standard treatment for early-stage EC is hysterectomy and bilateral salpingo-oophorectomy with or without pelvic node dissection. The objectives of this review are to present the fertility-sparing management options available to preserve fertility and assess follow-up and outcomes. A detailed literature search was carried out in order to survey the evidence for fertility-sparing treatment. The results of this search show that complete response to conservative treatment can be achieved in the majority with low rates of disease progression.
Fertility-sparing management of EC can be considered for patients with histologically confirmed grade 1 endometroid carcinoma without myometrial invasion and the absence of metastatic disease [4]. The most recent European Society of Gynaecological Oncology (ESGO) EC guideline highlights these indications and the possibility of fertility preservation [4]. Current evidence does not support fertility-sparing management of grade 2 or 3 disease without myometrial invasion or stages greater than the International Federation of Gynecology and Obstetrics (FIGO) 1A [4]. Molecular classifications should also be considered. Low risk groups with known molecular classifications for stage I DNA polymerase epsilon exonuclease domain mutations (POLEmut) and mismatch repair deficiency/non-specific molecular profile (MMRd/NSMP) endometrioid carcinoma with negative lymphovascular space invasion (LVSI) indicate good prognosis and could favour a conservative approach [4]. However, intermediate disease of stage 1B or positive LVSI or high grade p53abn cases would not be considered appropriate due to the higher risk of progression and recurrence [4]. The emerging molecular classification of EC will continue to help improve the risk stratification for patients desiring fertility-sparing treatments [2].
Staging investigations should be carried out in the same way as the conventional surgical pathway along with multidisciplinary discussion and decision making. ESGO advises that fertility-sparing management should only be incorporated by experienced gynaecological oncologists with a clear protocol in place, informed consent and strict follow-up measures [4]. Patients must be aware that fertility-sparing management of EC is not the gold standard treatment. They also must be willing to undergo follow-up with regular hysteroscopic surveillance and biopsies, which may not be acceptable to every patient. It is also crucial that patients are counselled to understand that their preoperative biopsy has its limitations and that hysteroscopic biopsy carries the highest correlation in predicting tumour grade [9]. 3–5% of patients with grade 1, stage 1A disease will have lymph node metastases [10], 5% ovarian involvement [11] or a synchronous ovarian carcinoma in 11–29% [12]. Laparoscopic evaluation has therefore been undertaken in some studies to assess these cases before proceeding with fertility-sparing management [13]. In the event that fertility-sparing management fails, hysterectomy will be offered.
A computerized literature review was conducted from 1950 until 1st June 2022. PubMed and MEDLINE were utilised to identify all relevant studies for patients with early-stage EC or atypical hyperplasia (AH) treated by fertility-sparing means. All applicable studies were appraised along with their references to identify other relevant articles. All studies were assessed by two independent reviewers (MB and AM). Eligibility was initially assessed by consideration of titles and abstracts. Articles were then obtained and the decision to include them was made after comprehensive and meticulous examination. Retrospective cohort studies, case-control studies, prospective studies and randomised control studies were considered for review. The most relevant studies have been reported in order to provide the best available evidence for fertility-sparing management of EC.
Progestin acts by downregulating oestrogen receptors, thereby suppressing endometrial growth and activating oestrogen metabolism [14]. It also exerts a direct cytotoxic, anti-tumour effect on the endometrium [15]. Oral progestins and the levonorgestrel-releasing intrauterine system (IUS) have therefore been used as non-surgical hormonal treatment for EC. Continuous medroxyprogesterone acetate (MPA) (400–600 mg/day) or megestrol acetate (MA) (160–320 mg/day) are two of the suggested oral progestin regimes with a minimum treatment of 6 months [2].
MA has been shown to produce the highest remission rates compared to other progestins in a systematic review and meta-analysis (odds ratio (OR) 2.70, 95% confidence interval (CI) 1.20–6.02%) [16], but MPA exhibited lower recurrence rates [2]. The bioavailability of MA over MPA is significantly higher and likely accounts for this difference in remission [17]. A meta-analysis of AH and EC by Wei et al. [18] showed a pooled complete response (CR) rate of progestin use of 71% (95% CI 63–77%). Zhang et al. [19] showed a similar CR rate in EC alone of 79.5% (95% CI 81.7–94.3%) but a recurrence rate of 27.3% (95% CI 18.2–37.6%). These studies have all been incorporated into Table 1 (Ref. [20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37]) to give an overall picture of CR rates.
| Authors | Study design | No. of patients | Ix | Rx | Median follow-up period | CR Overall (AH/EC) | PD Overall (AH/EC) | Pregnancy rate (AH/EC) | Live birth rate (AH/EC) |
|---|---|---|---|---|---|---|---|---|---|
| Kim et al. [30] | Retrospective | 50 | AH, EC | Progestin | 23 months | 35% | - | - | 10% |
| Kim et al. [25] | Prospective | 44 | EC | MPA + IUS | 6 months | 37.1% | 0% | - | - |
| Pal et al. [31] | Retrospective | 46 | AH, EC | IUS | 4.2 years | 75/67% | 6.7/22.2% | - | - |
| Hwang et al. [32] | Retrospective | 5 | Grade 2 EC | MPA + IUS | 44.4 months | 60% | 0% | - | - |
| Maggiore et al. [22] | Retrospective | 48 | AH, EC | IUS | 82.6 months | 89.3/81.3% | 3.6/12.5% | 54.5/100% | 17.9/43.8% |
| Tamauchi et al. [24] | Retrospective | 39 | AH, EC | MPA | 52 months | 93/89% | 0% | 35.9% | 25.6% |
| Yamagami et al. [20] | Retrospective | 162 | AH, EC | MPA | 71.3 months | 98.5% | 0/3.1% | 29.2/22.7% | - |
| 90.7/98.1% | |||||||||
| Yang et al. [33] | Retrospective | 160 | EC | HR + progestin | 20 months | 97.4% | 2.5/2.5% | 45% | 25% |
| Tock et al. [34] | Retrospective | 16 | AH, EC | HR + GnRH | 40.7 months | 66.7% | 0% | 53.3% | 43.75% |
| Giampaolino et al. [35] | Retrospective | 69 | AH, EC | HR + IUS | 24 months | 92.7/78.6% | 0/9.1% | - | 40% |
| Minig et al. [29] | Prospective | 34 | AH, EC | IUS + GnRH | 29 months | 95/57.1% | 5/28% | 32.4% | 20.6% |
| Casadio et al. [36] | Prospective | 9 | EC | HR + IUS | 6 months–5 years | 100% | 0% | - | - |
| Park et al. [37] | Retrospective | 148 | EC | Oral progestin | 41 months | 77.7% | 0% | - | 38.3% |
| Dolapcioglu et al. [23] | Prospective, randomised | 104 | AH | MPA or IUS | 24 months | 50% | - | - | - |
| 84% | |||||||||
| Westin et al. [21] | Prospective | 57 | AH, EC | IUS | 12 months | 83% (90.6/66.7%) | 10.6% | - | - |
| Janda et al. [26] | Prospective, randomised | 165 | AH, EC | IUS +/- metformin +/- weight loss | 6 months | 61% | - | - | - |
| 57% | |||||||||
| 67% | |||||||||
| Yang et al. [27] | Prospective, RCT | 150 | AH, EC | MA +/- metformin | 16 weeks & 30 weeks | MA = 20.7% + MF = 34.3% | - | - | - |
| Mitsuhashi et al. [28] | Prospective | 36 | AH, EC | MA + metformin | 38 months | 80.6% | 5.6% | - | - |
Ix, indication; Rx, treatment; CR, complete response; PD, progressive disease; AH, atypical hyperplasia; EC, endometrial cancer; MPA, medroxyprogesterone acetate; HR, hazard ratio; GnRH, gonadotrophin hormone-releasing hormone; IUS, levonorgestrel-releasing intrauterine system; MA, megestrol acetate; MF, metformin.
Yamagami et al. [20] addressed the issue of recurrence and repeat treatment in their retrospective series of 162 patients with AH and EC. If after 4 months CR occurred following hysteroscopic visualisation and curettage with MPA treatment, the progestin was then discontinued. If no resolution at this point, 2 monthly sampling was carried out until complete response was achieved. Follow-up was for 2 years with 3–4 monthly biopsies. They were able to demonstrate a CR of 90.7% (p = 0.097) in EC patients in the initial treatment group and 98.1% in the repeat treatment arm [20]. 6.2% of EC patients had stable disease with 3.1% progressing [20]. The length of treatment required was similar between the initial and retreatment groups for EC (6.1 versus 6.6 months).
Westin et al. [21] conducted a prospective, single-arm trial using IUS for AH and EC with a duration of 12 months. The majority of patients responded by 3 months. The CR rate in EC patients was 66.7% at 12 months, with 4.3% having a partial response (PR), 6.4% stable disease and 10.6% progressive disease amongst both groups [21]. 56.5% reported abnormal bleeding in the first 3 months. Non-responders were less likely to have pathological evidence of exogenous progesterone effect at 3 months (p = 0.001) with higher nuclear protein (Ki67) expression (p = 0.023) and lower baseline DKK3 expression (p = 0.030) [21]. Quality of life was also assessed with responders reporting significantly higher physical function and vitality scores compared to non-responders (p = 0.03, p = 0.04 respectively) [21]. There was no difference in body mass index (BMI) between responders and non-responders, but larger median uterine diameter meant non-response was more likely. Maggiore et al. [22] conducted a retrospective analysis of the IUS for treatment of EC, with 81.3% CR by 5 months, with CR achieved in 75% of those with grade 2 disease also. Progressive disease was seen in 12.5% of those with grade 1 EC with a relapse rate of 38.5% mostly seen at 25 months post treatment [22].
An IUS is recommended as first line treatment of AH by the Royal College of Obstetricians and Gynaecologists (RCOG) over oral progestins due to its higher disease regression rate, fewer side effects and advantageous bleeding profile compared to oral progestins [38]. This recommendation was based on a meta-analysis and systematic review on patients with simple hyperplasia and showed that the IUS achieved a higher regression rate compared with oral progestins after 3 months (OR 2.30, 95% CI 1.39–3.82%) and up to 24 months of treatment (OR 7.46, 95% CI 2.55–21.78%) [39]. A minimum duration of treatment of 6 months has been advocated, based on randomised studies showing greater efficacy when compared to 3 months treatment [23, 38]. Longer term data is lacking, and it is common practice to cease treatment after 6 months with oral agents [38], but 5 years with the IUS is encouraged [20, 24, 38]. A pooled CR rate for the IUS by Wei et al. [18] was 76% (95% CI 67–83%) with a relapse rate of 9% (95% CI 5–17%).
Baker et al. [40] conducted a meta-analysis and systematic review assessing the efficacy of both oral and intra-uterine progestins in achieving a CR in AH and EC. 219 patients were included with an even split between (complex atypical hyperplasia) CAH and EC [40]. 74% (95% CI 65–81%) of patients with AH and 72% (95% CI 62–80%) of patients with EC achieved a CR with oral progestins compared to 68% (95% CI 45–86%) with intrauterine progestins in EC [40]. Overall relapse was seen in 20.1% of patients after an initial CR [40]. A 2018 meta-analysis of 619 cases showed a CR with oral progestins of 76.3% (95% CI 70.7–81.1%), with a recurrence rate of 30.7% (95% CI 21–42.4%) [41]. The IUS group had a slightly lower CR of 72.9%, (95% CI 60.4–82.5%), with a recurrence rate of 11% (95% CI 5.1–22%) [41]. Both studies noted the lack of high quality evidence and called for prospective randomised control trials [40]. Kim et al. [25] conducted a multicentre prospective study to assess the efficacy of the IUS combined with MPA in EC patients. The CR was 37.1% at 6 months with partial response (PR) in 25.7%. No progression was noted. 20.5% of patients withdrew from the study. Wei et al. [18] showed a pooled CR of 87% (95% CI 75–93%) when both progestin and IUS are used with Zhang et al. [19] showing a higher pooled CR of 94.2% with IUS alone (95% CI 83.2–99.6%) and recurrence of 3.9% (95% CI 0.1–13%), which was significantly lower than with oral progestins alone (p = 0.0001).
Side effects and adverse outcomes of progestins are rarely reported in this group of patients. It is crucial in counselling to warn of these possible effects, particularly as the progestin doses are higher than conventional therapy for other benign treatments. Yamagami et al. [20] were one of the few papers to report adverse outcomes and side effects. These included weight gain, venous thromboembolism, liver dysfunction and allergic reaction. This represented less than 4% of cases [20].
The recent feMMe trial was a randomised control trial (RCT) of patients with
either AH or EC and BMI of greater than 30 kg/m
Chu et al. [44] conducted a systematic review of the use of metformin
to help prevent and treat EC. Metformin was not associated with a lower risk of
EC, but it did significantly improve the overall survival of patients with EC
compared to those not taking metformin (hazard ratio (HR) = 0.61, 95% CI
0.48–0.77%, p
Zhang et al. [19] have shown promising results with the use of gonadotrophin hormone-releasing hormone (GnRH) agonists and aromatase inhibitors in fertility sparing treatment for EC patients. As well as the overexpression of oestrogen and progesterone receptors in EC, GnRH receptors are also overexpressed. Minig et al. [29] prospectively examined the use of the IUS for 1 year with a GnRH analogue for 6 months. Only 14 patients with EC were included with a complete response in 57.1% and progression in 28% [29].
Obesity is a major risk factor for EC and therefore weight loss advice and planning should be an essential part of any fertility-sparing protocol. 90% of gynaecological patients have expressed the acceptability of discussing weight loss and 50% accepted referral to bariatric services [45]. Evidence of weight loss and recurrence risk after conservative management is lacking. A 2018 Cochrane review analysed the effect of interventions for weight reduction in improving survival in women with EC, but found evidence was limited and of low quality [43]. Combined behaviour and lifestyle interventions did not improve overall survival (relative risk (RR) 0.23, 95% CI 0.01–4.55%, p = 0.34), nor were they associated with significant weight loss (mean difference –1.88 kg, 95% CI –5.98–2.21 kg, p = 0.37) [43].
The impact of bariatric surgery in EC patients is also deficient. Fast track
access to a bariatric service for consideration of weight loss surgery should be
offered to all patients in line with NICE guidance if they have a BMI of over 50
kg/m
Hysteroscopic resection allows for targeted excision of early-stage EC, along with a more detailed evaluation of margin status and molecular classification than can be gained from dilatation and curettage (D&C) alone [2]. However, there is risk of perforation in pursuing hysteroscopic resection and this treatment has not been recommended by British gynaecological cancer society (BGCS) or ESGO. Hysteroscopic resection has been carried out prior to commencement of progestin treatment, but case series remain small and complications not always recorded.
Giampaolino et al. [35] carried out a series of 69 patients with both
AH and EC treated with hysteroscopic resection followed by IUS insertion. Only 14
of these had EC [35]. 78.6% in the malignant group had CR with 18.2% having a
subsequent relapse after 24 month follow-up and 9.1% having progression [35].
Yang et al. [33] conducted a retrospective study and analysed 40
patients with EC managed with hysteroscopic resection of suspected lesions.
Progestin therapy was started after hysteroscopic evaluation with MA 160 mg/day,
50% were also on metformin as part of their cancer treatment [33]. CR was seen
in 97.3% of patients at 18 months follow-up, with mean treatment to achieve CR
seen at 6.4
Tock et al. [34] carried out a retrospective study of 8 patients with EC, assessing the combination of endometrial resection followed by a GnRH agonist with a 3 month follow-up interval. 57% had CR at 3 months with 43% having stable disease [34]. No patients had relapse or progression after a median follow-up of 40.7 months. No intrauterine adhesions occurred but no adverse hysteroscopic events were recorded.
Endometrial ablation is not advised as an alternative treatment for EC as complete destruction cannot be guaranteed, disease may persist and surveillance can be made challenging with intrauterine adhesions [38].
The RCOG advises that there must be at least one negative endometrial biopsy before trying to conceive with AH, but referral to a fertility specialist should be sought before attempting to conceive [38]. European society of human reproduction and embryology (ESHRE) has produced a guideline on female fertility preservation, acknowledging fertility loss as a detrimental impact of cancer treatment [50]. Assisted reproduction treatment (ART) may be the quickest way to achieve pregnancy whilst also reducing the time frame before definitive surgery can be carried out. ART also minimizes the window of unopposed oestrogen stimulation of the endometrium whilst aiming to ensure the shortest time in which relapse or disease progression could occur.
Yang et al. [27] showed a pregnancy rate of 37.5% for their patients undergoing fertility-sparing treatment of EC. A live birth rate of 25% was reported in those actively trying to conceive, but this was a mixture of both AH and EC patients [42]. Maggiore et al. [22] showed a pregnancy rate of 100% in those with EC, 75% of which underwent in vitro fertilisation (IVF) with a live birth rate of 43.8%. Wei et al.’s [18] meta-analysis of AH and EC showed a pooled pregnancy rate of 34% (95% CI 30–38%) after progestin treatment, with a 20% live birth rate. Zhang et al.’s [19] live birth rate for EC patients alone was higher at 32.3% (95% CI 22.9–42.5%).
In Giampaolino’s [35] series, 40% that had their IUS removed following hysteroscopic resection achieved a live birth after natural conception in the 12 months of follow-up. Wei et al.’s [18] meta-analysis of IUS treatment showed a pooled pregnancy rate of 18% (95% CI 7–37%) with a live birth rate of 14%. When the IUS and progestin treatment was undertaken, pooled pregnancy rate increased to 40% (95% CI 20–63%) with a 35% live birth rate [18]. Fan et al.’s [41] meta-analysis highlighted a pregnancy rate of 52.1%, 95% CI 41.2–66% with oral progestins, 56% (95% CI 37.3–73.1%) after treatment with the IUS and 47.8% (95% CI 37.3–73.1%) after hysteroscopic resection and progestin therapy.
Chae et al. [42] also looked at pregnancy outcomes after
fertility-sparing management for AH and EC after CR. Progestin and metformin
compared to progestin only achieved similar, non-significant pregnancy and live
birth rates. 54% became pregnant in the combined treatment group versus 48% in
the progestin only portion [42]. 66.6% of these patients achieved a full term
birth, 3.3% preterm birth and 23.3% miscarriages [42]. The median time from end
of treatment to successful pregnancy was 7.67 months [42]. Only 1 pregnancy out
of 30 resulted from natural conception, the rest required ART of varying degrees.
The only multivariate analysis that was shown to have an effect on predicting
pregnancy failure was grade of disease (OR 6.2, 95% CI 1–38.9%, p
It is important to note that despite CR with conservative treatment, young obese EC patients will still face the challenges of fertility and obstetric outcomes that are associated with the metabolic syndrome of obesity. Adverse outcomes of those with obesity include increased rates of pregnancy induced hypertension, pre-eclampsia and gestational diabetes. Prepregnancy counselling by a medical obstetric team should also be conducted so patients are aware of these added risks.
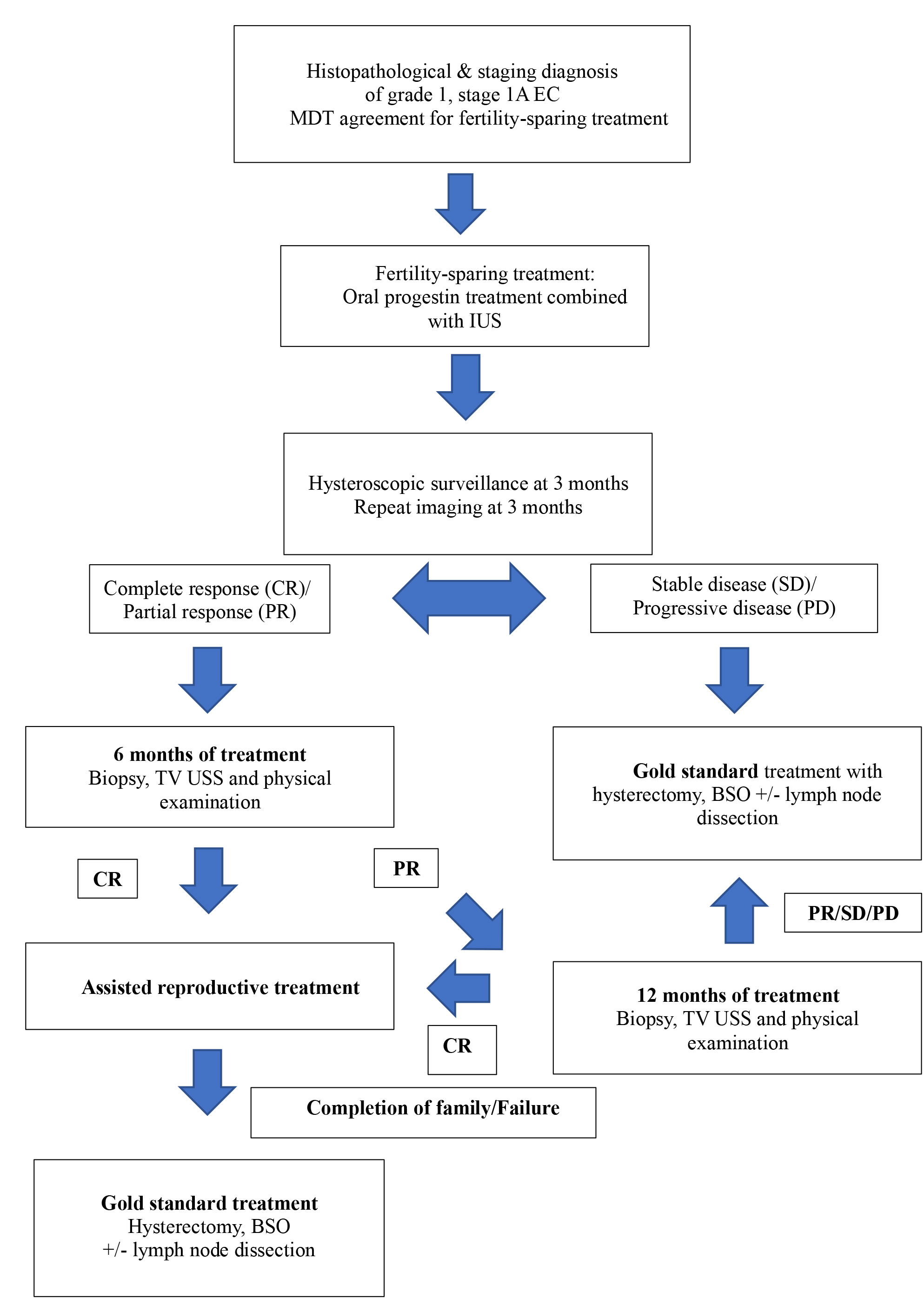
Assessing response to fertility-sparing treatment is needed along with ensuring progression of disease has not occurred. ESGO guidelines advise that hysteroscopic visualisation and biopsy along with repeat imaging must be carried out at 3–4 and 6 months [4]. If no response at 6 months is seen, standard surgical management should then be recommended [4]. Continuous hormonal treatment should be used until pregnancy is desired. Six-monthly follow-up is then advised with transvaginal ultrasound (TVUSS) and physical examination [4]. Hysteroscopic and endometrial biopsy are only advised if TVUSS indicates abnormal findings or there is abnormal uterine bleeding. Hysterectomy and bilateral salpingo-oophorectomy is recommended as soon as childbearing is complete due to the risk of recurrence and progression. The RCOG greentop guideline recommends fertility-sparing surveillance of AH be managed with 3-monthly biopsies until two consecutive negative samples, and then 6–12 monthly biopsies [38]. A flowchart of suggested management is presented below in Fig. 1.
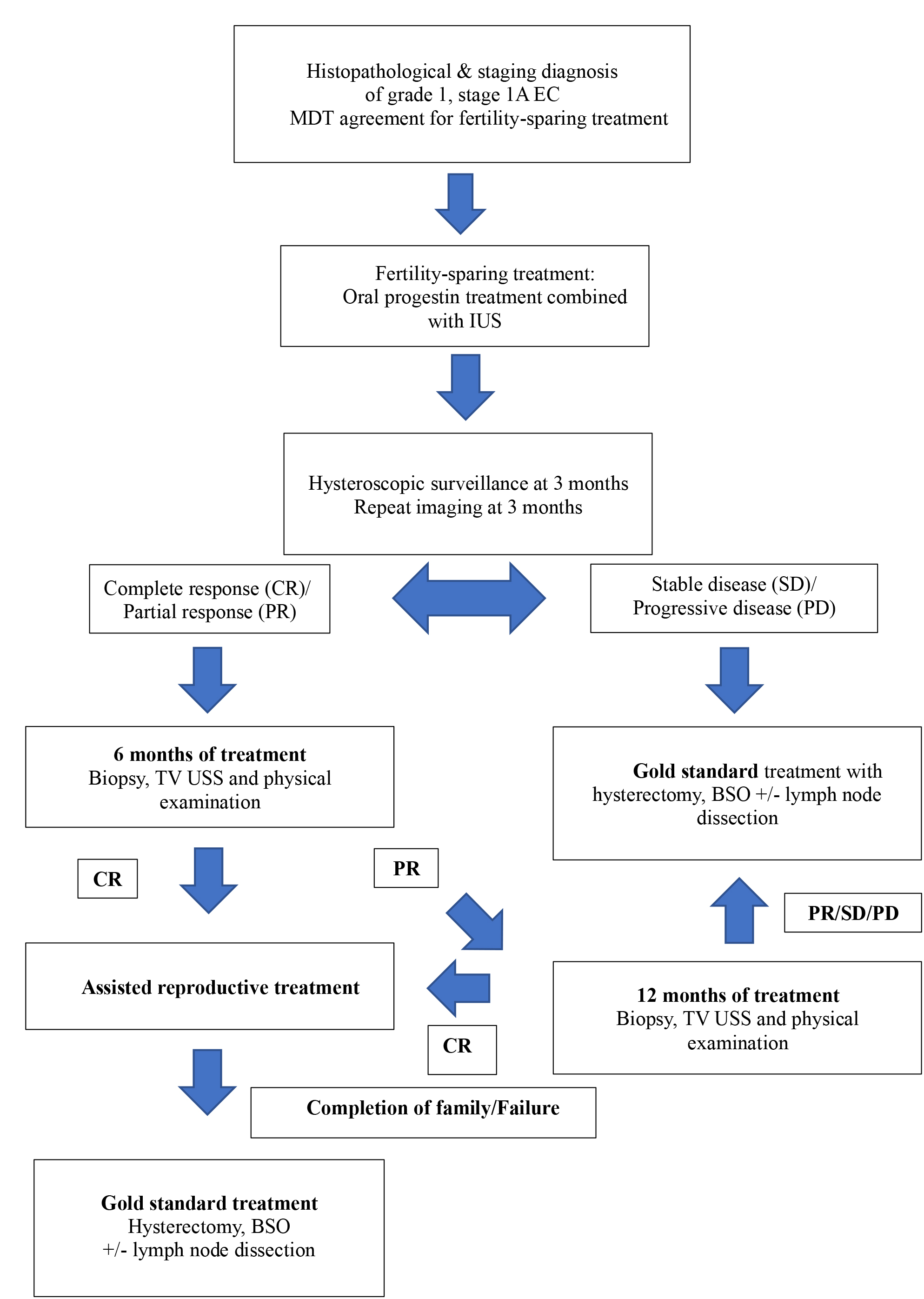 Fig. 1.
Fig. 1.Flowchart of management of fertility-sparing treatment of EC.
It is crucial that patients undergoing fertility-sparing treatment are given the best available evidence of the risk of relapse and progression of cancer. Disease progression whilst on oral progestins was reported as 2.7% in a meta-analysis and systematic review by Baker et al. [40], whilst another review highlighted 33.1% went on to have a hysterectomy for various reasons and myometrial invasion was found in 14.8% of those cases [16]. Remission probability plateaus at 12 months and recurrence probability increases continually for at least 5 years [16]. Koskas et al. [16] looked at recurrence and could find not factors which led to an increased likelihood of the event. They showed that the recurrence probability increased with longer length of time, the 4-, 6-, 12-, 18- and 24- month recurrence probabilities were 3.6%, 9.6%, 17.2%, 26% and 29.2% respectively [16].
Progestin and metformin treatment combined have lower disease relapse than progestin alone [42]. However combined therapy was not associated with different remission rates, pregnancy or live birth rates [42]. Other progestin regimes compared to MA were associated with an increased probability of progression, OR 3.95, 95% CI 1.44–10.81% [16]. The relapse rate after hysteroscopic resection from Yang et al.’s [33] series was 11.1% seen at a median of 7 months. Only 1 patient out of 40 showed progression to superficial myometrial invasion confirmed on histology after hysterectomy [33].
Patients at higher risk of relapse with AH are those with BMI
Pregnancy has been shown to slow the rate of recurrence of endometrial cancer
after complete remission. Median disease free survival was shown by Chae
et al. [42] to be 26 months in those that had a pregnancy, compared to
12 months in the non-pregnant group (p
Overall survival after fertility-sparing treatment of EC at the 2-, 5- and 10-year mark were all 99% respectively for EC after initial treatment, with 100% respectively amongst the retreatment group in Yamagami et al.’s [20] analysis. Greenwald et al. [51] assessed a cohort of 161 (2.5%) women whom initially received hormonal therapy for grade 1 and 2, stage 1 EC and followed them up for a median of 6.9 years in comparison to those that received standard surgery (6178 patients, 97.5%) to assess long-term survival. All-cause mortality was not significantly different between the groups, 14.1% in the hormone group versus 9.3% who underwent surgery [51]. Cancer-specific mortality was non-significantly higher in the hormone therapy group of 9.2% versus 2.1% in the surgery group. This difference was accounted for by 3 late deaths in the hormone cohort, and remained non-significantly higher when grade 1 EC only was examined; 10 yr mortality of 15.67% versus 7.83% in the conventional treatment group [51]. BMI or parity were not collected and could account for the differences [51]. Therefore, the use of hormone therapy as an alternative to standard surgical treatment does not appear to affect long-term survival albeit with the limitations of these studies, more studies are needed to assess survival in this cohort of patients. A centralized database of these patients receiving fertility preserving treatment is required to give more accurate survival data, as advocated by the Gynecological InterGroup [52].
This review has been able to incooperate all the relevant studies in a field not widely explored in gynaecological oncology with few randomised control trials. This review has been able to also appraise the more recent randomised feMMe trial which highlights the important contribution of weight loss as an adjunct to tackling EC in fertility-sparing management. This review is limited by the fact that there are few randomised studies assessing the fertility-sparing approach and other studies have low patient numbers, but highlights the need for more robust evidence in this area, particularly as this is going to become an increasing problem in line with the escalating obesity rates amongst this patient population.
This review can help shape an evidence-based fertility-sparing management protocol in clinical practice. The importance of a weight loss programme with access to bariatric services should be part of a holistic approach in conjunction with an expediated referral to fertility services. A progestin used in combination with metformin should be considered to lower relapse rates. MA has been shown to have higher remission rates yet MPA shows less recurrence. The IUS is also effective but without the same progestin side effect profile, so treatment can be tailored to individual patients and their morbidities.
EC incidence is on the increase in the premenopausal population along with obesity rates and the average first age of parenthood. Fertility-sparing management of EC has not traditionally been considered a feasible option for women. However, due to changing patient demographics, it is imperative that these options be discussed with patients where fertility is desired and that they are managed through a specialist gynae-oncology multi-disciplinary team (MDT). The use of weight loss as an adjunct to treatment with progestins should be part of the overall management along with the concurrent use of metformin to lower relapse rates. The choice of progestin needs to be individualised taking in to consideration patients’ wishes and tolerance of oral progestins.
AM conducted the literature review and wrote the manuscript. JC/MB supervised, read, and approved the final manuscript. All authors read and approved the final manuscript.
Not applicable.
We would like to thank all the reviewers for their opinions and suggestions.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.