-
- Academic Editor
-
-
-
†These authors contributed equally.
Low-grade squamous intraepithelial lesions (LSIL) are early pathological changes associated with cervical cancer, exhibiting varying progression rates. The risk factors for progression from LSIL to high-grade squamous intraepithelial lesions (HSIL) and the development of a predictive model for this progression have not been thoroughly investigated.
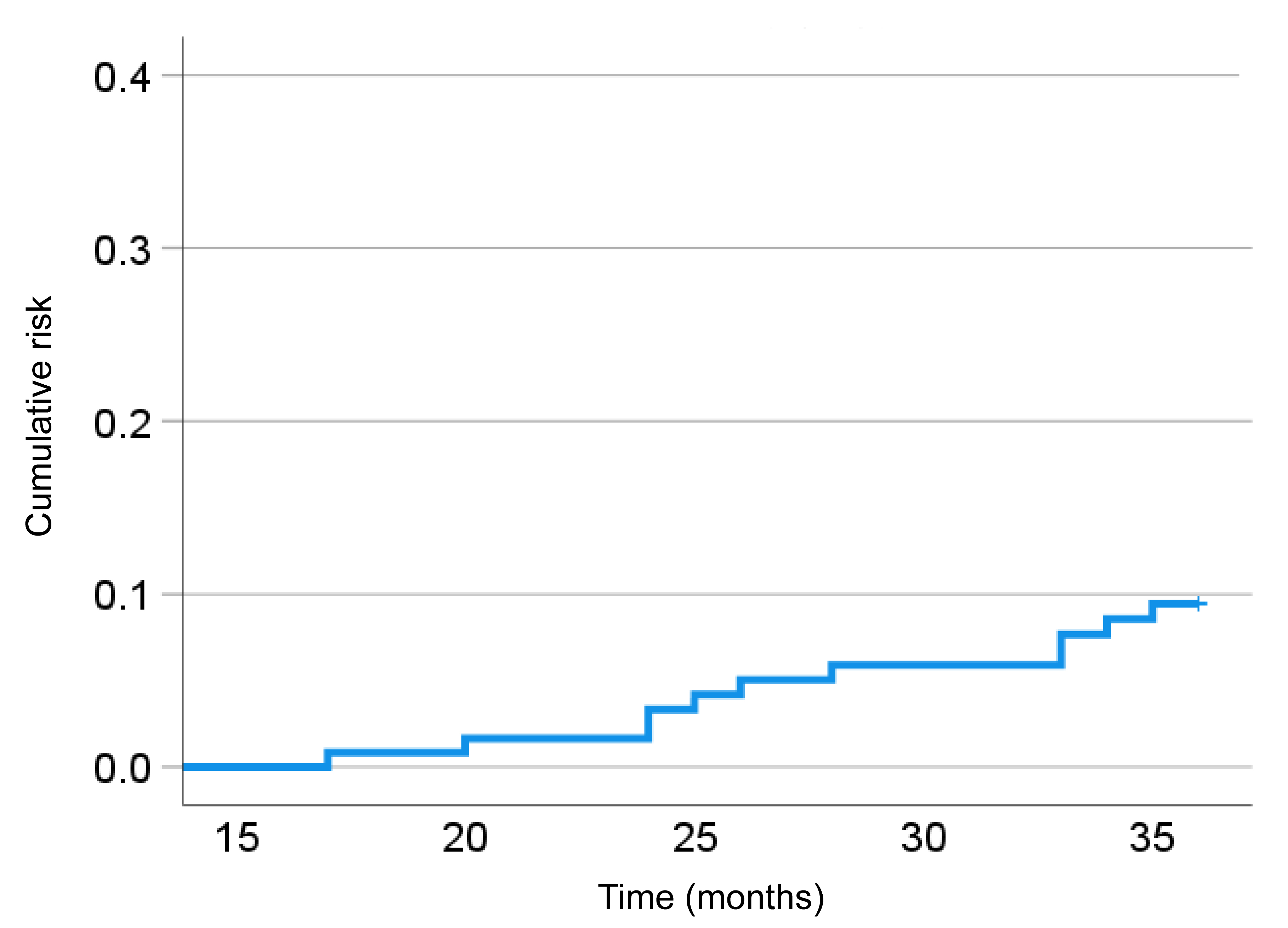
This single-center, retrospective study followed 122 patients diagnosed with LSIL, who were monitored without treatment, over a 3-year period. Clinical and pathological data were collected, and univariate and multivariate logistic regression analyses were performed to identify independent risk factors for progression to HSIL. A predictive model was developed based on these factors and validated using both training and validation cohorts.
Of the 122 patients, 11 (9.01%) progressed to HSIL within 3 years. Univariate analysis revealed that persistent high-risk human papillomavirus (HPV) infection, HPV16/18 genotype, and persistent or recurrent symptoms significantly increased the risk of progression to HSIL. Multivariate analysis confirmed that persistent high-risk HPV infection (odds ratio (OR) = 7.67, p = 0.027) and persistent or recurrent symptoms (OR = 21.07, p < 0.001) were independent risk factors for progression to HSIL. A nomogram incorporating these factors demonstrated excellent predictive performance in both the training cohort (area under the curve (AUC) = 0.92) and the validation cohort (AUC = 0.88). Calibration and decision curve analysis further validated the model’s reliability and clinical applicability.
Persistent high-risk HPV infection and recurrent symptoms are key predictors of LSIL progression to HSIL. The developed predictive model can assist clinicians in identifying high-risk patients for early intervention, thus improving clinical management and optimizing healthcare resource utilization.