-
- Academic Editor
-
-
-
Ovarian yolk sac tumor (OYST) is a rare and malignant subtype of malignant ovarian germ cell tumors (MOGCT). Due to its rarity, few large-scale studies have systematically evaluated the prognostic factors for this tumor type. In the present study, our aim was to identify independent prognostic factors for OYST and develop a nomogram to predict patient survival.
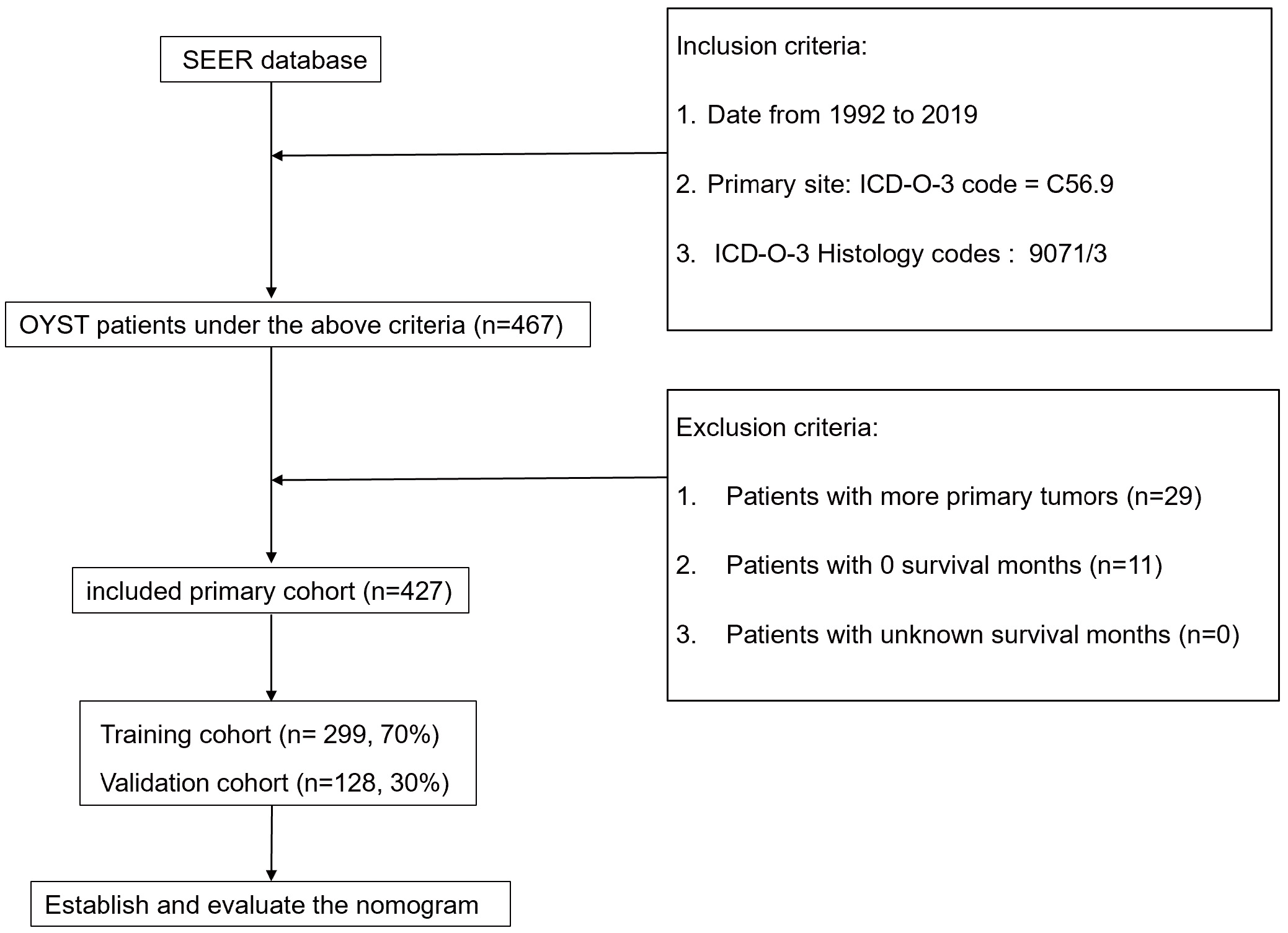
Data from 427 OYST patients diagnosed between 1992 and 2019 were extracted from the Surveillance, Epidemiology, and End Results (SEER) database. Patients were randomly divided into training (n = 299) and validation (n = 128) cohorts. Univariate Cox regression, Least Absolute Shrinkage and Selection Operator (LASSO) regression, and multivariate Cox analysis were used to identify prognostic factors. A nomogram was constructed based on age, American Joint Committee on Cancer (AJCC) stage, regional lymph node status, and liver metastasis. The model’s accuracy and clinical utility were evaluated using the concordance index (C-index), calibration curves, time-dependent receiver operating characteristic (ROC) curves, and decision curve analysis (DCA).
Age, AJCC stage, regional lymph node status, and liver metastasis were identified as independent prognostic factors for OYST. The nomogram demonstrated strong predictive accuracy, with C-indices of 0.868 and 0.813 in the training and validation cohorts, respectively. Calibration curves confirmed the agreement between predicted and observed survival rates. The time-dependent ROC curves showed area under the curves (AUCs) exceeding 0.8 for 3-, 5-, and 10-year survival predictions. DCA revealed that the nomogram provided a superior net benefit compared to the AJCC staging system. A risk stratification system based on the nomogram effectively differentiated high- and low-risk patients, with Kaplan-Meier survival analysis indicating significantly worse outcomes for high-risk patients.
The nomogram developed in this study provides accurate and clinically relevant predictions for the survival of OYST patients. Furthermore, it offers a valuable tool for individualized prognostic assessment and postoperative decision-making. Prospective, multicenter studies are needed to validate and further refine this model.