- Academic Editor
†These authors contributed equally.
Group visits have been widely utilized in the management of chronic diseases and have demonstrated favorable clinical outcomes. Therefore, by leveraging this model, we implemented group visits for patients undergoing preimplantation genetic testing (PGT). This study aimed to explore the effects of the group visit model on patient anxiety levels, social support, disease-related knowledge, and satisfaction with health education of patients undergoing PGT.
A total of 120 patients undergoing PGT for the first time at our reproductive center from 5 March 2022 to 31 October 2022 were randomly divided into the control and intervention groups. The control group received routine health education, and the intervention group received family-centered group health education. The knowledge of PGT, satisfaction with health education, along with anxiety and social support levels, were compared between the two groups before and after the intervention. The differences were statistically significant at p < 0.05.
Overall, 113 participants completed the intervention, with 55 assigned to the control group and 58 to the intervention group. Participants in the intervention group exhibited significantly reduced anxiety levels and substantial improvements in social support, disease knowledge, and satisfaction with health education compared to those in the control group.
The implementation of family-centered group health education for patients undergoing PGT is effective in clinical practice and warrants widespread adoption.
The study has been registered on https://www.chictr.org.cn/ (registration number: ChiCTR2300069544; registration link: https://www.chictr.org.cn/showproj.html?proj=172588).
Preimplantation genetic testing (PGT) is a testing technique that integrates assisted reproductive technology (ART) with molecular genetics. It involves analyzing the DNA from oocytes (polar bodies) or embryos (either at the cleavage stage or the blastocyst stage) before implantation. This testing is conducted to determine human leukocyte antigen (HLA) typing or to identify any genetic abnormalities before implantation [1]. In 1990, Handyside et al. [2] pioneered genetic testing technology, assisting a couple with a sex chromosome linkage disorder to conceive a healthy baby successfully. PGT technology is advancing rapidly and is extensively utilized for patients with monogenic genetic disorders, chromosomal abnormalities, recurrent pregnancy loss, and other genetic conditions. With the continuous development of detection methods, diagnostic accuracy has now exceeded 97% [1]. PGT requires coordinated multidisciplinary care involving reproductive medicine, embryology, genetics, and nursing teams. It encompasses a range of complex procedures such as ovulation induction, oocyte retrieval, sperm extraction, in vitro fertilization (IVF), embryo culture, embryo biopsy, genetic testing, and embryo transfer (ET).
Patients often lack understanding of diseases, treatment procedures, medications, and complication prevention, creating a strong need for clear information. Conventional health education depends on verbal instruction, which can inundate patients with information, leading to poor retention and ineffective results. Such overwhelming experiences can cause psychological stress during treatment, which may negatively affect the diagnostic accuracy, treatment effectiveness, and pregnancy outcomes. Although treatment requires the husband’s cooperation, it is often the female patient who attends appointments alone, leading to feelings of isolation and a lack of support. Research indicates that patients undergoing PGT experience diminished social support and high levels of anxiety [3].
The group visits model serves as a framework for managing diseases by bringing together individuals with a high frequency of medical resource utilization and those with similar or diverse diagnoses [4]. This model facilitates the implementation of health education and individualized diagnosis and treatment conducted by qualified health service personnel. This approach has been applied in clinics since the 1990s [5]. Currently, the model is widely used in patients with hypertension, diabetes, obstetric conditions, and other health issues, yielding satisfactory results [4, 5, 6, 7]. Therefore, this study aims to investigate the effect of the family-centered group health education model on anxiety levels, social support, disease knowledge, and health education satisfaction among patients undergoing PGT.
From 5 March 2022 to 31 October 2022, 120 PGT couples who met the inclusion and exclusion criteria and sought treatment at our reproductive endocrinology department were selected. Subjects were assigned randomly to the control or intervention groups (n = 60 cases/group). This study was approved by the ethics committee of our hospital (IRB-20200292-R), with informed consent obtained from both patients and their families.
Inclusion criteria: (1) Female patients aged 20–45 years; (2) Patients with PGT indications [8], who underwent PGT treatment for the first time; (3) Proficient in using mobile phone software; (4) Education level of junior high school or above, with normal audiovisual reading and writing abilities; (5) Patients with clear consciousness, and no psychological or psychiatric disorders; and (6) Patients who voluntarily agree to participate in the study.
Exclusion criteria: Individuals for whom one or both spouses have severe physical illnesses.
Dropout criteria: (1) Patients who changed treatment plan midway. (2) Individuals who exhibit poor compliance during the intervention process. (3) Participants who did not complete the required four health education sessions.
Sample size calculation: According to the primary outcome measure, the Hamilton Anxiety Scale (HAMA), using the following formula, incorporating pre-experimental results.
In the formula, n1 and n2 are the sample sizes required for each
group. The significance level is
Medical staff conducted conventional PGT health education to provide pertinent information to patients. The topics covered included the following: (1) Genetic counseling: Geneticists provided counselling on the types of genetic abnormalities, their pathogenesis, and the concepts, purposes, significance, and risks of PGT. (2) File establishment, informed consent signing, mock ET, and ovulation induction: Doctors and nurses in the outpatient department explained the PGT process, including the costs involved, testing plans, required documents, instructions for administering ovulation induction medications, follicle monitoring, laboratory tests, and guidance for sperm collection. (3) Ovum and sperm retrieval, IVF, embryo culture, embryo biopsy, genetic testing, and ET: Preoperative and postoperative health education, as well as discharge education, were conducted by the ward’s doctors and nurses. If patients experienced negative emotions during treatment, the medical staff offered prompt comfort and support, addressed any concerns, and provided personalized question-and-answer (Q&A) services through the WeChat public account backend.
A family-centered group health education model was adopted, focusing on families that included the patient and her husband. This model involved offline group instruction in small groups of 3 to 5 families, along with online Q&A sessions and the dissemination of scientific content aimed at enhancing their understanding and application of knowledge and processes. Each offline session lasted 60 minutes, divided into 30 minutes of instruction followed by 30 minutes of post-class discussion. Participation necessitated the completion of four offline sessions. The specific steps for implementation were as follows:
2.2.2.1 Establishment of a Professional Intervention Team
The team was composed of a variety of specialists, including the chief nurse of the reproductive endocrinology department, a senior physician in reproductive endocrinology, a laboratory embryology specialist, a level 2 psychological counselor, two specialized ART nurses, and two senior nurses. As the project leader, the chief nurse oversaw and coordinated relevant matters. Before implementation, she guided the team by explaining the research purpose, plan, and questionnaire procedures. The physician and the embryology specialist provided specialized knowledge needed for course materials and educational content, ensuring the patients’ inquiries were addressed with accurate and comprehensive scientific information. The senior nurses were responsible for random grouping, developing course material for offline classes, and collecting relevant science articles and videos for online distribution. The psychological counselor collected and reviewed the questionnaires and provided psychological counseling to patients. A nurse specialized in assisted reproduction updated and reviewed the course materials and educational content, and facilitated face-to-face teaching lessons as well as online Q&A sessions. Another assisted reproduction specialty nurses and the psychological counselor collected and analyzed the data. All group education materials (including lecture slides, WeChat-delivered science articles, and videos) underwent rigorous review by our multidisciplinary team before implementation. The group of educators uniformly completed standardized training and competency assessments. The nurses in charge of group education monitored real-time attendance and verified signed course certificates to ensure full program adherence.
2.2.2.2 Offline Group-Based Health Education
The management team members continuously updated the course material based on the feedback from the patients in the previous group session. Ultimately, the teaching content was refined into four themes: tips for registration, precautions during ovulation induction, cooperation before and after egg retrieval and sperm collection, and key points pre- and post-transplantation. The nurses in charge of group education tracked the progress of each couple and scheduled offline group-based classes for couples with similar treatment progress through phone calls and WeChat group sign-ups. Each session included 3–5 couples and lasted for 30 minutes. At the end of the course, the instructor posed review questions to reinforce key concepts and assess knowledge retention. After each class, a stamp and signature were provided, and the next class time was scheduled based on the patient’s follow-up appointment. Each PGT couple participated in each themed course once, with at least a 3-day interval between the courses.
2.2.2.3 After-Class Group Discussion
Live questioning sessions were organized for patients with lingering concerns, where both the instructor and other patients contributed joint responses to enhance the teaching effect. Patients were motivated to communicate with one another, share their treatment experiences, express their negative feelings, and provide comfort. This exchange aimed to foster positive energy and assist patients in cultivating positive emotions.
2.2.2.4 Health Education WeChat Group
The health education WeChat group encompassed management team members and all patients in the intervention group. Upon enrollment, patients joined the group by scanning a quick response (QR) code. During treatment, patients were able to consult through the WeChat group, where the research team provided timely answers and resolved doubts. During the study period, the research team regularly produced science popularization articles and videos, which were shared weekly with the education WeChat group. Patients who successfully conceived were invited to share their experiences and insights with the group, enhancing the confidence of others in their treatment journey. As each offline course concluded, participants raised questions regarding the popular science articles distributed throughout the two-course period, which aimed to enhance the effectiveness of online science education. The online educational materials, including science popularization articles and videos, covered a broad range of topics such as distinctions among the first, second, and third generations of IVF, an overview of the PGT process, key considerations and packing guidelines for egg retrieval hospitalization, discharge instructions, common questions regarding fresh ET, the development process of embryos, embryo grades, essential baby-related terminology, how a 99% sperm deformity can still result in conception, and reasons why embryos fail to implant, among other topics.
This self-designed questionnaire was used to gather patients’ information, including medical records and contact numbers, age, reasons for undergoing PGT, family income, educational level, and occupation.
The HAMA scale [9], developed by Hamilton, is divided into two major factor
structures: psychological and somatic, with 14 items in total. It uses a 5-point
Likert scale, ranging from 0 to 4, with 0 indicating “no symptom” and 4
denoting “extremely severe symptom”. A higher score indicates a higher level of
anxiety. It is one of the most commonly used scales in psychiatric clinical
practice. The psychological anxiety subscale consists of 7 items (items 1, 2, 3,
4, 5, 6, and 14), whereas the somatic anxiety subscale consists of 7 items (items
7, 8, 9, 10, 11, 12, and 13). According to the National Scale Collaboration Group
data, scores
The SSRS [10] scale, compiled by Professor Shuiyuan Xiao in 1986, consists of
three dimensions: objective support, subjective support, and the utilization of
social support, with 10 items in total and a maximum score of 66. A higher total
score indicates a better social support status. Social support scores of
This self-designed test (shown in Supplementary Table 1) was used to
evaluate the mastery of PGT knowledge. After compilation, the questionnaire was
discussed and finalized by medical, nursing, and laboratory experts. The
questionnaire includes 11 items: reasons for undergoing PGT, procedures, risks,
costs, precautions during ovulation induction, precautions before and after egg
retrieval, precautions before and after ET, PGT testing methods, timing of
testing, precautions for males, and required documents. Each item is divided into
5 levels: very unfamiliar, somewhat unfamiliar, moderately familiar, quite
familiar, and very familiar, with scores ranging from 1 to 5 and 55 points in
total. A higher score indicates a higher level of awareness. The Cronbach’s alpha
of the PGT knowledge questionnaire in 113 PGT patients in this study was 0.770.
The validity analysis demonstrated excellent construct validity
(Kaiser-Meyer-Olkin (KMO) = 0.896; Bartlett’s
The questionnaire (shown in Supplementary Table 2) referred to the
health education module content in the “Inpatient Nursing Service Satisfaction
Scale” developed by Feng et al. [11] with slight modifications. It
consists of four items: hospital service guidance, education format,
pre-treatment notification, and discharge guidance. Items were evaluated on a
scale from very dissatisfied to very satisfied, with seven levels in total. The
seven options are assigned scores from 1 to 7, respectively. The Cronbach ’s
alpha of the health education satisfaction questionnaire in 113 PGT patients in
this study was 0.852. The validity analysis demonstrated excellent construct
validity (KMO = 0.869; Bartlett’s
The numbers from 1 to 120 were written on uniform-sized paper, and 120 small paper strips were placed into a sealed opaque envelope, which was kept by the group members until the end of recruitment. Strips with single-digit numbers were assigned to the intervention group, while those with double-digit numbers were assigned to the control group.
Due to the nature of the intervention, neither the participants nor the researchers could be fully blinded to the study conditions. During the study, the grouping and data evaluation, and statistical analysis were carried out by different personnel. The grouping allocation of patients is only informed by the grouping personnel and the group health education personnel. The data evaluation and statistical analysis personnel were not informed of the grouping allocation, and the data evaluation was conducted designated evaluator in a private consultation room through one-on-one patient assessment, to avoid the interference of other personnel. If the evaluator became aware of the patient’s group assignments during the intervention phase, the patient was withdrawn from the study. Participants remained blinded to the research hypothesis and any additional interventions.
Two key evaluation points were chosen: the cycle entry day and the day before oocyte pickup. (1) Cycle entry day (before intervention): during this phase, general information about the patients was collected. Patients filled out the PGT knowledge questionnaire, HAMA, and SSRS. Patients in the intervention group scanned the QR code to join the WeChat group and were given an offline class attendance sheet. (2) Day before oocyte retrieval (after intervention): the PGT knowledge questionnaire, health education satisfaction rating scale, SSRS, and HAMA were completed to assess the impact of family-centered group health education on PGT patients’ cognition, social support, anxiety levels, and satisfaction with health education during the treatment cycle. Psychological counselors and trained nurses in assisted reproduction conducted the questionnaire. They explained the significance, purpose, content, and requirements of the study to the patients and their families, obtaining informed consent. A unified guidance language was used to assist patients in filling out the questionnaires. All questionnaires were collected on-site, and the investigator promptly verified their validity and completeness to address any missing items and rectify errors.
Statistical software SPSS 26.0 (IBM Corp., Chicago, IL, USA) was used for data
analysis. Categorical data were expressed as counts and percentages [n (%)].
When the total number of cases (N) was
A total of 120 PGT patients were enrolled, of whom two changed their treatment
plan halfway through, and five patients failed to follow up. Ultimately, 113 PGT
patients completed the intervention, including 58 patients in the intervention
group and 55 in the control group (Fig. 1), which is within the expected sample
size range and meets the sample size requirement. No statistically significant
differences were found between the two groups regarding age, education level,
family income, occupation, and reasons for undergoing PGT (p
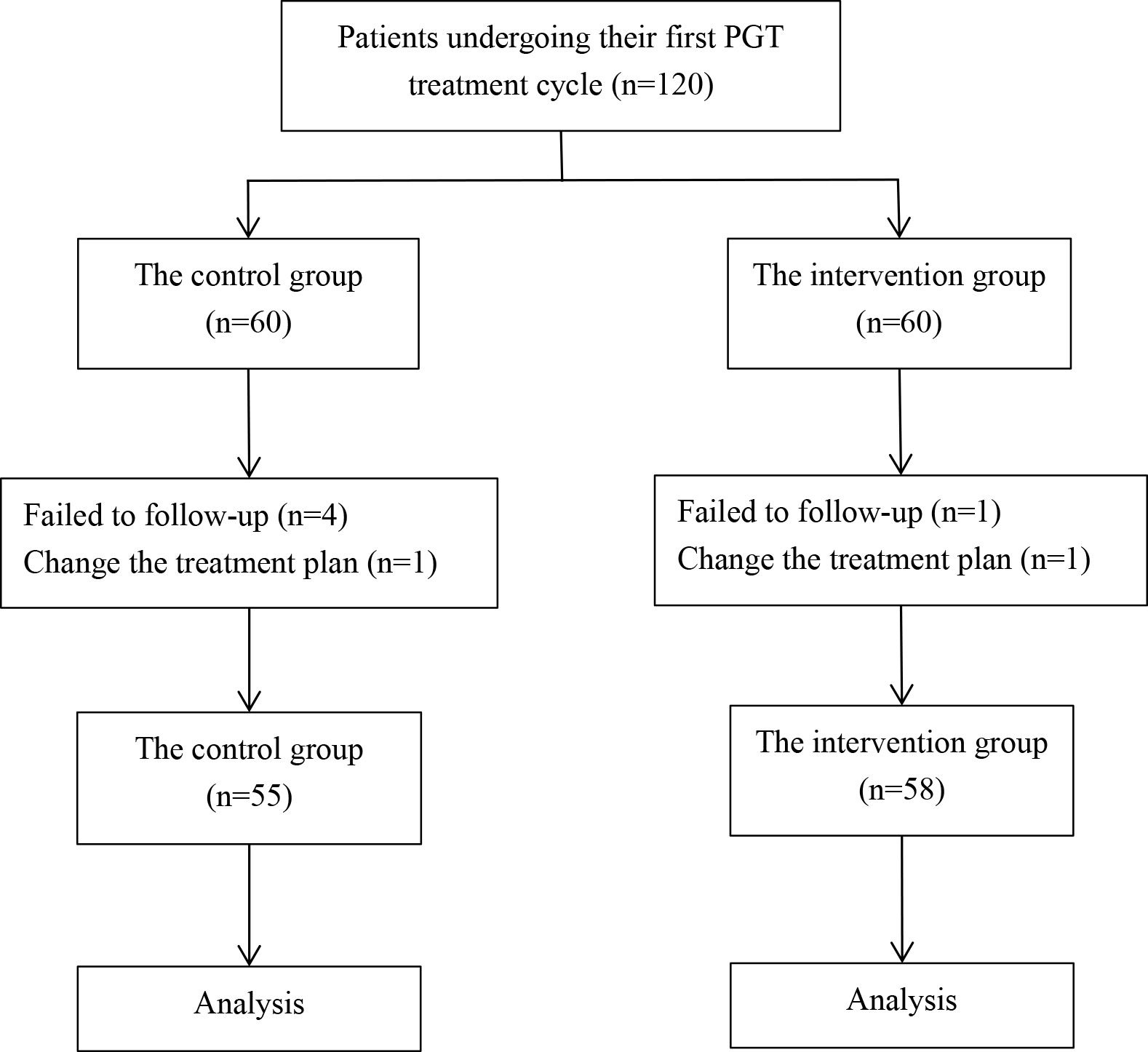 Fig. 1.
Fig. 1.
Flow chart. The flowchart illustrates the step-by-step process of this study. PGT, preimplantation genetic testing; n, number of samples.
| Items | Intervention group (n = 58) | Control group (n = 55) | p | ||
| Age (years) (%) | 1.187 | 0.276 | |||
| 49 (84.5) | 42 (76.4) | ||||
| 9 (15.5) | 13 (23.6) | ||||
| Educational level (%) | 1.974 | 0.160 | |||
| High school and below | 15 (25.9) | 21 (38.2) | |||
| Junior college and above | 43 (74.1) | 34 (61.8) | |||
| Family income ($) (%) | 0.154 | 0.926 | |||
| 17 (29.3) | 18 (32.7) | ||||
| 14,000–28,000 | 21 (36.2) | 19 (34.5) | |||
| 20 (34.5) | 18 (32.7) | ||||
| Occupation (%) | 2.392 | 0.302 | |||
| Staff | 43 (74.1) | 47 (85.5) | |||
| Self-employed | 7 (12.1) | 3 (5.5) | |||
| Jobless | 8 (13.8) | 5 (9.1) | |||
| The reasons for undergoing PGT (%) | 0.747 | 0.688 | |||
| Female | 22 (37.9) | 20 (36.4) | |||
| Male | 18 (31.0) | 21 (38.2) | |||
| Other | 18 (31.0) | 14 (25.5) | |||
| PGT indication (%) | 1.198 | 0.549 | |||
| Chromosome abnormality | 30 (51.7) | 34 (61.8) | |||
| Genetic abnormality | 14 (24.1) | 11 (20.0) | |||
| Abortion ( |
14 (24.1) | 10 (18.2) | |||
At baseline assessment, the intervention group (n = 58) exhibited 17 cases
(29.3%) of probable anxiety and 8 cases (13.8%) of definite anxiety, while the
control group (n = 55) showed 20 cases (36.4%) of probable anxiety, 3 cases
(5.5%) of definite anxiety, and 2 cases (3.6%) of significant anxiety.
Following the intervention, the anxiety profile demonstrated notable changes: in
the intervention group, probable anxiety cases decreased to 16 (27.6%) with only
2 cases (3.4%) of definite anxiety remaining; conversely, the control group
displayed an increase to 24 cases (43.6%) of probable anxiety along with 5 cases
(9.1%) of definite anxiety and persistent 2 cases (3.6%) of significant
anxiety. No statistically significant differences in the total HAMA and dimension
scores were found between the intervention and control groups pre-intervention
(p
| Items | Time | Intervention group (n = 58) | Control group (n = 55) | Z | p |
| HAMA total score | Pre-intervention | 6.00 (4.00, 9.25) | 6.00 (4.00, 10.00) | –0.646 | 0.518 |
| Post-intervention | 4.00 (2.75, 7.00) | 7.00 (4.00, 11.00) | 3.078 | 0.002** | |
| Z | 3.201 | –0.420 | |||
| p | 0.001** | 0.675 | |||
| Somatic anxiety | Pre-intervention | 1.00 (1.00, 3.00) | 2.00 (0.00, 4.00) | 0.044 | 0.965 |
| Post-intervention | 1.00 (0.00, 2.00) | 2.00 (1.00, 4.00) | 3.196 | 0.001** | |
| Z | 2.578 | –1.168 | |||
| p | 0.010* | 0.243 | |||
| Psychological anxiety | Pre-intervention | 4.00 (3.00, 6.25) | 5.00 (3.00, 7.00) | –0.851 | 0.395 |
| Post-intervention | 3.00 (2.00, 5.25) | 6.00 (2.00, 7.00) | 2.691 | 0.007** | |
| Z | 3.146 | 0.199 | |||
| p | 0.002** | 0.843 |
Note: Data are shown as median and quartile spacing [M (P25, P75)]. * means
p
No statistically significant difference was found between the intervention and
control groups in the total social support score and dimension scores
pre-intervention (p
| Item | Time | Intervention group (n = 58) | Control group (n = 55) | t/Z | p |
| SSRS total score | Pre-intervention | 36.17 |
37.31 |
–1.120(1) | 0.265 |
| Post-intervention | 40.02 |
37.00 (33.00, 42.00) | 2.236(2) | 0.025* | |
| t/Z | –5.538(1) | –0.720(2) | |||
| p | 0.471 | ||||
| Subjective support | Pre-intervention | 20.41 |
21.24 |
–1.265(1) | 0.208 |
| Post-intervention | 22.24 |
21.00 (19.00, 24.00) | 1.594(2) | 0.111 | |
| t/Z | –5.536(1) | –0.782(2) | |||
| p | 0.434 | ||||
| Objective support | Pre-intervention | 8.60 |
8.00 (7.00, 9.00) | 1.122(2) | 0.262 |
| Post-intervention | 10.00 (8.00, 11.25) | 8.00 (8.00, 10.00) | 2.536(2) | 0.011* | |
| t/Z | –3.804(2) | –2.105(2) | |||
| p | 0.002** | 0.035* | |||
| Utilization of support | Pre-intervention | 7.16 |
7.00 (7.00, 9.00) | 1.450(2) | 0.147 |
| Post-intervention | 8.12 |
7.00 (6.00, 9.00) | 2.215(2) | 0.027* | |
| t/Z | –3.710(1) | –1.186(2) | |||
| p | 0.236 |
Note: Data are shown as mean
No statistically significant difference in PGT knowledge questionnaire scores
was found between the two groups pre-intervention (p
| Item | Time | Intervention group (n = 58) | Control group (n = 55) | Z | p |
| PGT knowledge questionnaire | Pre-intervention | 29.00 (25.75, 33.00) | 30.00 (26.00, 36.00) | –1.413 | 0.158 |
| Post-intervention | 48.00 (44.00, 52.25) | 40.51 |
–5.321 | ||
| Z | –6.569 | –5.509 | |||
| p |
Note: Data are shown as mean
The health education satisfaction score of the intervention group was higher
than that of the control group post-intervention, and the difference was
statistically significant (p
| Group | n | Education satisfaction scores | Z | p |
| M (P25, P75) | ||||
| Intervention group | 58 | 28 (27, 28) | 4.058 | |
| Control group | 55 | 26 (24, 28) |
Note: Data are shown as median and quartile spacing [M (P25, P75)]. *** means
p
Anxiety is a common manifestation of various mental disorders, characterized by
intense, overwhelming, and persistent feelings of worry and fear that can
escalate within minutes, often accompanied by physiological symptoms. Patients
undergoing ART for pregnancy frequently experience adverse emotions, including
anxiety and apprehension, because of the intricate nature of the process, high
costs, and unpredictable treatment outcomes [12, 13]. Furthermore, many patients’
spouses are who are unable to accompany them during treatment, resulting in a
lack of psychological and social support, which exacerbates their negative
emotions. In this study, the HAMA was employed to provide more objective
assessments, minimizing patient subjectivity. However, administering the HAMA
requires trained professionals with specialized expertise for proper evaluation.
A study has reported [14] that a considerable proportion of IVF patients still
have substantial emotional problems from before treatment and up to six months
after treatment. In the six months following unsuccessful treatment,
Social support involves individuals assisting vulnerable groups through supportive actions, helping them manage challenges effectively. It is divided into objective support, subjective support, and utilization of support [18]. PGT patients often have a history of abnormal fertility, recurrent miscarriages, chromosomal abnormalities, or carry abnormal genes [19]. Patients, influenced by the traditional Chinese culture, might experience guilt toward their families and concerns about how friends and relatives perceive them. This can result in an avoidance of treatment, reluctance to confront the support and concern from loved ones, and a decline in interpersonal communication and social engagement. Furthermore, the patient’s husband may not be frequently present during treatment, leading to a lack of social support for the patient. Matsubayashi et al. [20] suggest that adverse emotions in patients undergoing ART-assisted pregnancies largely stem from insufficient family support and care, underscoring the crucial role of family involvement and companionship throughout the treatment process. Research shows that greater social support correlates with more spiritual and material aid, improved disease knowledge, better marital quality, and reduced anxiety levels [21, 22]. This study adopted a family-centered group health education approach, allowing patients and family members to participate together, thereby strengthening their communication and enhancing the patient’s psychological and social support. To assess the influence of family-centered education on patients’ social support, the SSRS was selected for its efficiency and strong practicality compared to alternative assessment tools. Our findings showed that the total social support, objective support scores and support utilization of the intervention group were higher than those of the conventional control group. However, there were no statistically significant differences observed in the dimensions of patients’ subjective support may be attributed to several potential factors, including insufficient intervention frequency, limited intervention methods and formats, and possibly inadequate sample size. These aspects will be systematically improved in future studies.
Routine health education for ART patients primarily involves verbal explanations from medical staff, where patients typically receive information about the disease and treatment plans in a passive manner. However, this approach has several drawbacks, including unilateral one-sided information delivery and a lack of engagement due to repetitive formats [23]. Moreover, different medical professionals manage various stages of treatment, leading to inconsistencies in health education. As a result, there is often low cooperation between doctors and patients, which can hinder treatment. The management structure implemented in our research integrates professionals from reproductive medicine, laboratory embryology, and nursing specialties. The intervention team develops the curriculum, encompassing face-to-face instruction and online Q&A sessions that systematically, comprehensively, and continuously address every stage of PGT treatment. Integrating images, videos, live demonstrations, and various teaching techniques creates an educational experience that engages both visual and auditory senses. This approach not only makes health education more appealing but also sidesteps the downsides of conventional rote learning. The results show that the disease knowledge questionnaire scores of the patients in the intervention group were significantly higher than those in the control group. This indicates that the family-centered group health education model is more effective in addressing the disease and treatment needs of patients and their spouses, consistent with the research findings of Yang et al. [24].
The family-centered group health education model employs a group teaching format that incorporates various methods, including video and audio playback, live explanations, and visual displays. These approaches offer a broader range and deeper content. It also meets patients’ disease knowledge needs and ensures timely access to disease and treatment knowledge through online science articles, videos, and WeChat Q&A. A thorough understanding of the treatment process helps patients make informed decisions, thereby enhancing their overall medical experience. Compared to conventional health education, the family-centered group health education model transforms patients from passive recipients to active participants. This shift not only promotes a mutually trusting relationship between nurses and patients [25] but also more effectively addresses patients’ concerns. This model reduces feelings of loneliness by fostering support from medical staff, family members, and peers. Moreover, the communication platform it establishes enables patients to connect with others who share similar experiences, facilitating mutual support and promoting navigation of the treatment process. A survey on health education satisfaction was also conducted post-intervention. It was found that the health education satisfaction scores of the intervention group were significantly higher than those of the control group, indicating that the family-centered group health education model can effectively improve patient satisfaction.
This study aimed at the unique population of PGT patients, which enhanced the specificity of the study. At present, there are few reports on health education for PGT patients, and the application of the group management model in this population is particularly scarce. Therefore, this study has certain innovations. However, due to the limitations in time, manpower, resources, and funding, this study was conducted at a single reproductive center. As a result, the representativeness of the study population may be limited, which restricts the generalizability of findings to some extent. This study focuses on investigating HAMA and social support and analyzes and discusses them. Because the PGT knowledge questionnaire and the health education satisfaction questionnaire are self-made and lack universality, the investigation and discussion are insufficient. The intervention time was relatively short, and there was no long-term follow-up of patients; therefore, the sustained impact of the intervention could not be assessed. These limitations will be addressed and improved upon in future research.
In summary, the present study explored the effectiveness of a family-centered group health education model in 58 patients undergoing PGT, yielding favorable outcomes. This innovative approach not only alleviates anxiety for patients but also significantly enhances their comprehension of the disease. These positive outcomes highlight the need for serious consideration of broader implementation and dissemination. To validate and strengthen these findings, future studies should adopt multicenter, inter-regional, multi-ethnic, and longitudinal designs.
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
LX, YY, YL, XY and SW participated in the study design. YL participated in health education, YM and YY participated in question-answering collection and data analysis. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was conducted in accordance with the Declaration of Helsinki. All subjects gave their informed consent for inclusion before they participated in the study. This study was approved by the Ethics Committee of Women’s Hospital, School of Medicine, Zhejiang University (Approval Number: IRB-20200292-R).
The authors would like to thank the couple who participated in this study. We would also like to thank the department of reproductive endocrinology of our hospital, the medical staff cooperation and support.
This work was supported by the Medical Science and Technology Project of Zhejiang Province (Number: 2024KY1154).
The authors declare no conflict of interest.
During the preparation of this work, the authors used ChatGPT-3.5 and Deepseek to check spelling and grammar. After using this tool, the authors reviewed and edited the content as needed and took full responsibility for the final publication.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/CEOG40748.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
