- Academic Editor
Intramural pregnancy (IMP) is an extremely rare subtype of ectopic pregnancy, defined by the implantation of the gestational sac within the uterine myometrium, with no communication to the endometrial cavity, fallopian tubes, or uterine serosa. Compared with the other common ectopic pregnancies, IMP accounts for less than 1% of all ectopic cases, rendering it diagnostically challenging in clinical practice. Meanwhile, IMP carries substantial risks stemming from its atypical location, including uterine rupture, life-threatening hemorrhage, and maternal mortality, which underscores the critical need for early recognition. However, IMP is often missed in timely diagnosis due to its nonspecific clinical presentation and overlapping ultrasonic imaging features with other conditions such as cornual pregnancy and subserosal pregnancy. Transvaginal three-dimensional ultrasound (TDU) and magnetic resonance imaging (MRI) can clearly delineate the relationship between the gestational sac, uterine myometrium, and serosa, thereby enabling timely detection of early-stage IMP and informing clinical management.
A 27-year-old Gravida 2, Para 1 (G2P1) woman experienced 44 days of amenorrhea, accompanied by lower abdominal pain and irregular vaginal bleeding. Emergency transvaginal ultrasound examination indicated that the gestational sac was located in the left uterine horn, with dimensions of approximately 21 mm × 16 mm × 11 mm, suggesting a possible left uterine horn pregnancy, which was inconsistent with the successive results by TDU and magnetic resonance (MR) suggesting a uterine IMP. Subsequently, the intramural uterine tissue was removed by laparoscopy, and finally it was confirmed by pathological findings to be a uterine IMP.
IMP is rare and can have severe consequences if not treated promptly. TDU and MR are beneficial for early and accurate diagnosis, facilitating timely clinical treatment.
Ectopic pregnancy is a common acute abdominal disorder in obstetrics and gynecology [1]. With the increasing rates of induced abortions and cesarean sections, the incidence of ectopic pregnancy is on the rise, including those occurring in unusual locations. Intramural pregnancy (IMP) is a relatively rare type, with an incidence of less than 1% [2]. In natural pregnancies, it occurs in approximately 1 in 30,000 cases, and according to the existing literature on intramural pregnancies, only 56 cases have been published [3]. This condition is highly prone to misdiagnosis, and once the gestational sac ruptures, the situation can become extremely dangerous, even life-threatening, with reported mortality rates as high as 20% [4, 5, 6]. Therefore, early diagnosis is of great significance for clinical management. This article retrospectively analyzes a case of IMP and explores the value of transvaginal three-dimensional ultrasound (TDU) and magnetic resonance (MR) in its early diagnosis.
A 27-year-old Gravida 2, Para 1 (G2P1) woman presented with lower abdominal pain
and irregular vaginal bleeding for over ten days. On February 19, her
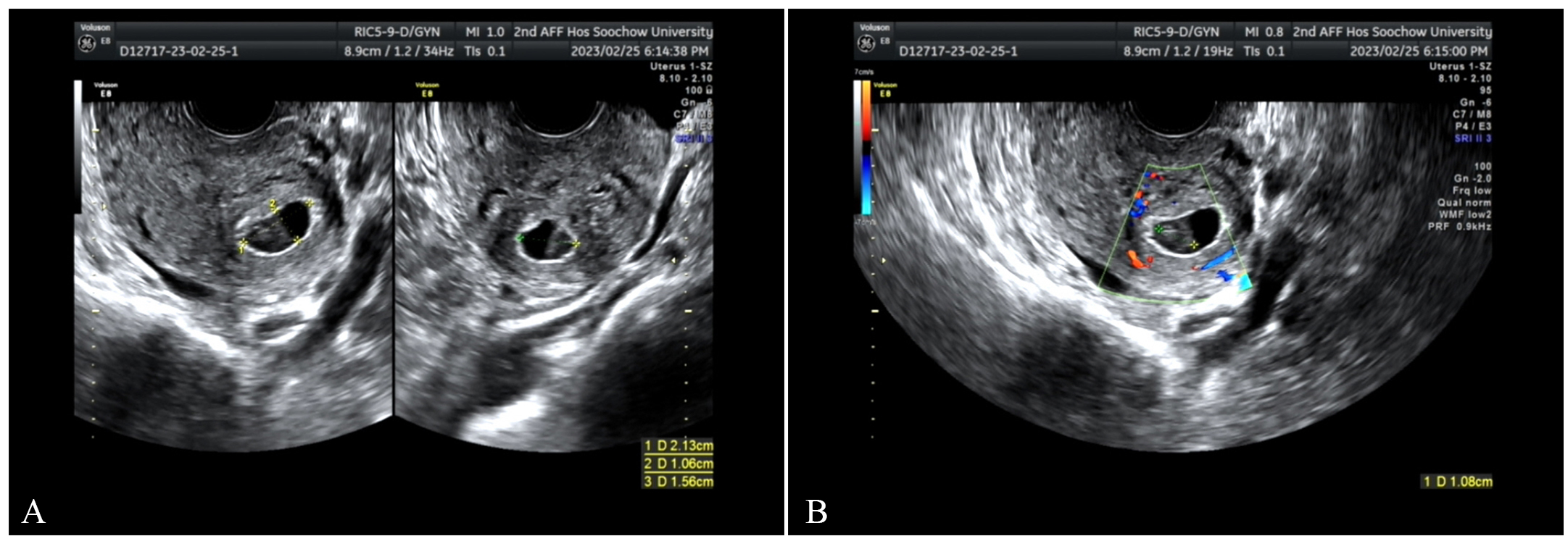 Fig. 1.
Fig. 1.
On February 26, transvaginal ultrasound scan. (A) A gestational sac
was seen near the uterine angle, measuring approximately 21 mm
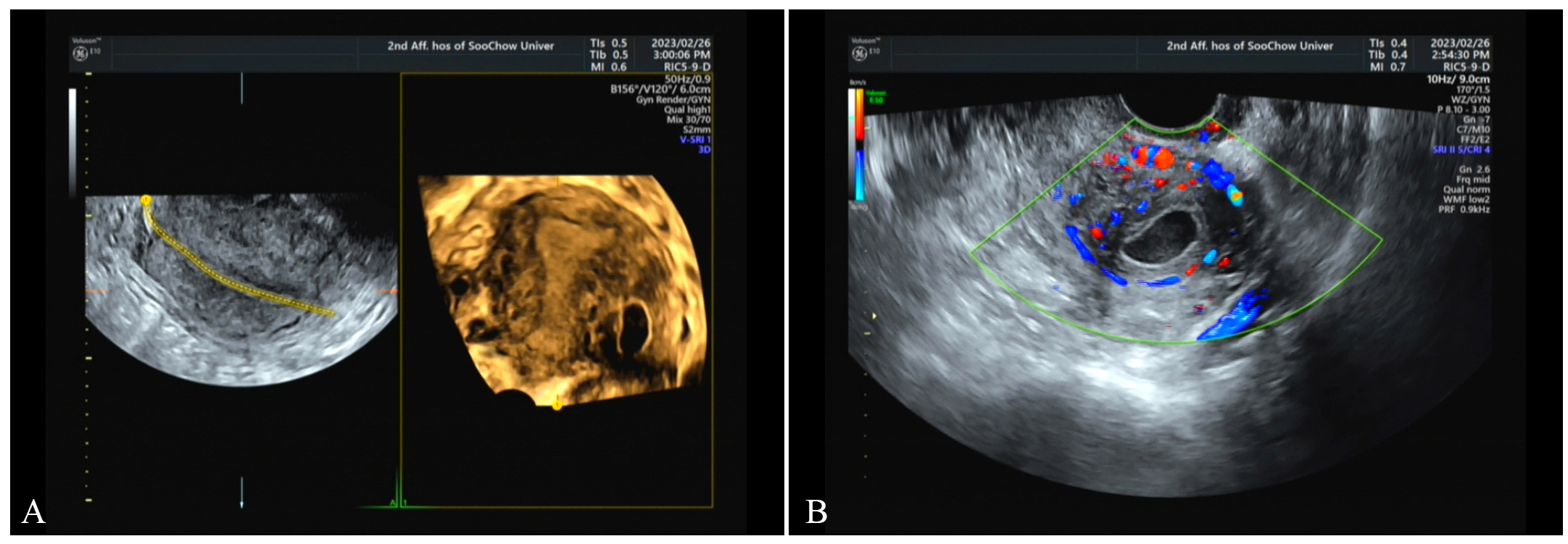 Fig. 2.
Fig. 2.
On February 28, transvaginal three-dimensional ultrasound (TDU). (A) There was an echo of the gestational sac between the muscle walls. (B) Blood flow signals around it are increased.
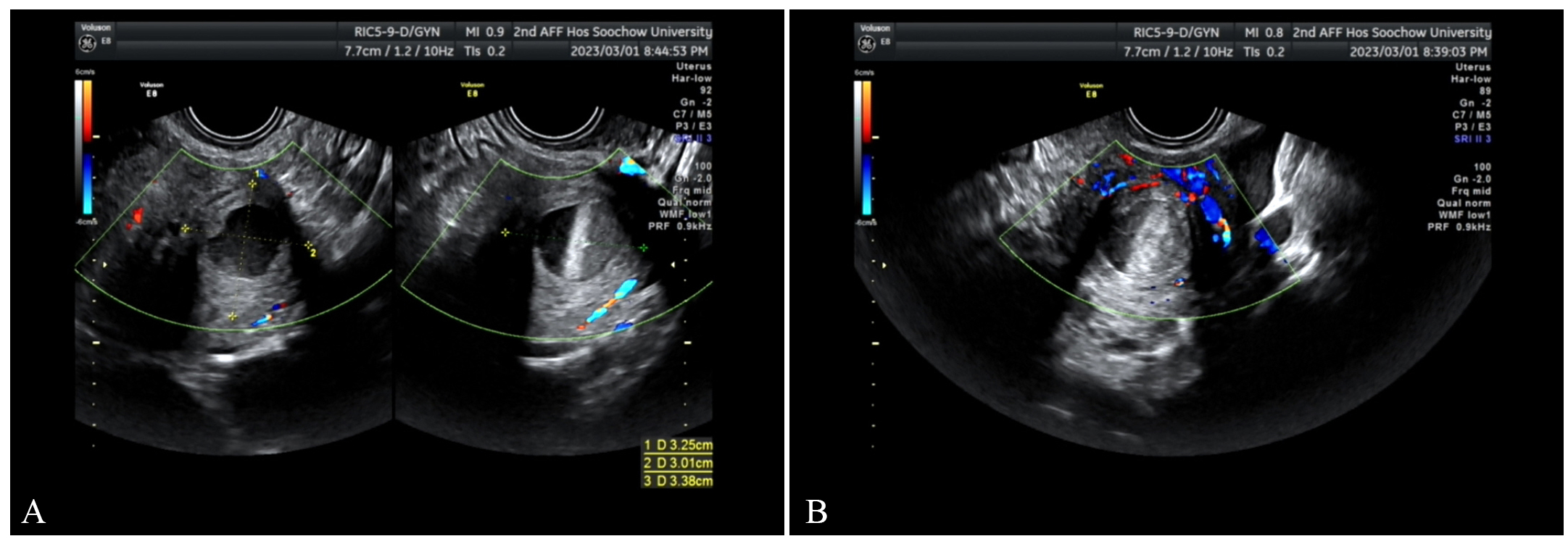 Fig. 3.
Fig. 3.
March 1, transvaginal ultrasound scan. (A) The mass has enlarged compared with previous findings. (B) The surrounding blood flow signals have increased.
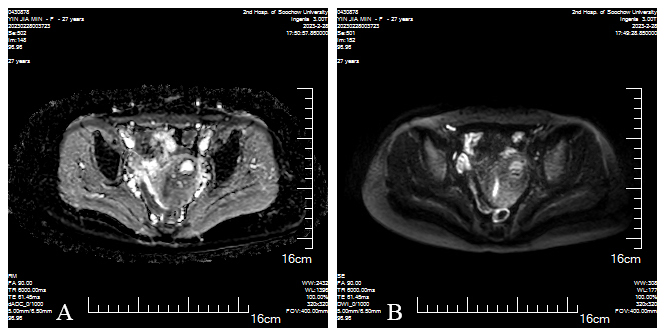 Fig. 4.
Fig. 4.
March 2, dADC (D-1), DWI (D-2) showed low signal intensity on the left side of the uterus. (A) dADC and (B) DWI both confirm low signal intensity on the left side of the uterus, with fluid present within this lesion, a possibility of gestational sac rupture and bleeding is suggested.
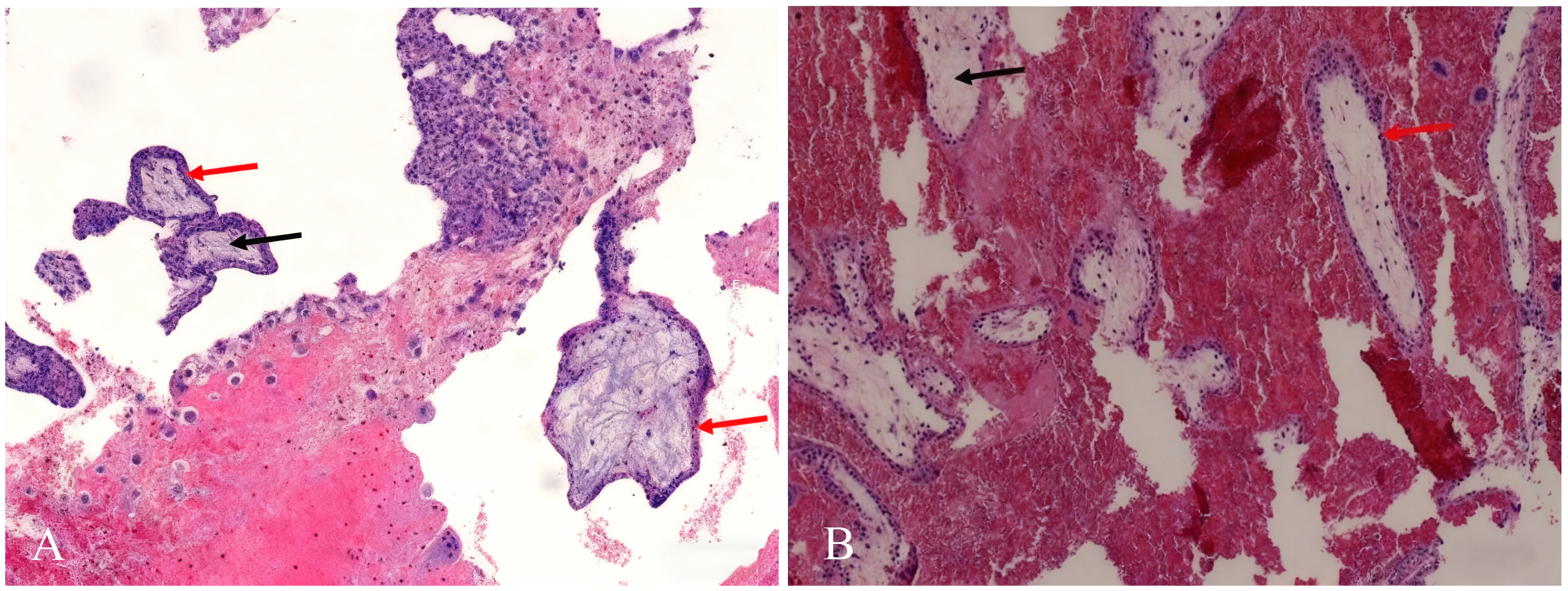 Fig. 5.
Fig. 5.
H&E stain
 Fig. 6.
Fig. 6.
IMP refers to the implantation of a fertilized egg in the myometrium of the uterus, without connection to the fallopian tube or uterine cavity. Its pathogenesis remains unclear but might be related to the following factors. Firstly, when an individual has a history of uterine cavity operations, especially induced abortion, which can easily damage the endometrium and the adjacent muscle layer. This allows fertilized eggs to enter the muscle layer through the damaged endometrium, leading to IMP. In this case, the patient had previously had two pregnancies, giving birth to a healthy baby boy four years ago, and having an abortion two years ago, which might have been the cause of the IMP.
Secondly, adenomyosis may also be associated with this condition. The fertilized egg can enter the muscle wall through the sinus channels formed by the ectopic endometrium in the myometrium, resulting in IMP. In addition, embryo transfer may damage the myometrium, meaning the fertilized egg is implanted in the myometrium, which forms the IMP. As the gestational sac in the myometrium gradually grows, it could easily invade the myometrial blood vessels, leading to uterine rupture and massive bleeding, which could endanger the patient’s life. Therefore, early diagnosis of IMP is of critical importance.
TDU enables comprehensive scanning of the uterus in sagittal, coronal, and other planes, facilitating the determination of whether the gestational sac communicates with the fallopian tubes or uterine cavity, thereby accurately identifying the location of an ectopic pregnancy. Conventional transvaginal ultrasound can provide information on the longitudinal and transverse sections of the uterus but fails to precisely distinguish the relationships between the uterine cavity, uterine horns, and interstitial regions in the coronal plane, which may lead to misdiagnosis as a cornual or interstitial pregnancy [7]. In this case, our initial transvaginal ultrasound incorrectly diagnosed the patient with uterine horn pregnancy.
Furthermore, TDU can accurately visualize the position and size of the
gestational sac within the myometrium, its relationship with the uterine cavity,
and the distance from the uterine serosal layer. This allows for differentiation
from a subserosal pregnancy [8], a rare type of intramural ectopic pregnancy
characterized by a gestational sac partially enclosed only by the uterine serosa,
with myometrial invasion
The pivotal role ultrasound plays in the diagnosis of ectopic pregnancy [11, 12] is widely recognized, and it is the preferred imaging modality for this reason. However, in certain scenarios, such as heavy vaginal bleeding, patient refusal of TDU, or significant intestinal gas interference that severely impairs ultrasound accuracy, MR imaging can instead be utilized. MR clearly delineates the myometrium and scar tissue, accurately identifies the implantation site of the gestational sac, serving as a valuable supplement to TDU. The combined use of these two modalities in the early stages, with mutual confirmation, enhances confidence in the clinical diagnosis and management of IMP, particularly when complicated by rupture. In this case, the patient presented with persistent and worsening lower abdominal pain. TDU diagnosed an IMP with increasing abnormal echoes, while MR revealed an abnormal signal focus in the left uterine wall, suggesting a possible rupture and bleeding of the gestational sac. Clinicians comprehensively evaluated these findings and performed timely surgery, which successfully alleviated the patient’s symptoms.
IMP is extremely rare, resulting in an early diagnosis rate of less than 50% [13]. In severe cases, it can even endanger the patient’s life. For patients with suboptimal treatment outcomes, early transvaginal TDU and MR examinations are necessary. These tests can help detect and distinguish special ectopic pregnancies as early as possible [14], thereby assisting clinicians in making correct treatment decisions.
All data generated or analyzed during this study are included in this published article.
CW and HL designed the research study. FL and WG carried out the research. All authors contributed to the editorial modifications of the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was carried out in accordance with the guidelines of the Declaration of Helsinki. This medical study has been granted ethics exemption by the Ethics Committee of the Second Affiliated Hospital of Soochow University, in compliance with applicable ethical guidelines. A written consent was signed by the patients or their families.
We would like to thank the Suzhou Science and Technology Development Plan Project for supporting the publication costs of this paper.
This research received no external funding.
The authors declare no conflict of interest.
During the preparation of this work, the authors used Doubao to check for spelling and grammatical errors. After utilizing this tool, the authors further reviewed and edited the content as necessary, and take full responsibility for the final content of this publication.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/CEOG41228.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
