-
- Academic Editor
-
-
-
Adequate thyroid hormone production is critical for fertility and the successful maintenance of pregnancy. Thyroid autoimmunity (TAI), characterized by the presence of thyroid peroxidase antibodies (TPOAb) and anti-thyroglobulin antibodies (TgAb), is the most common cause of thyroid dysfunction in women of reproductive age. The association between TAI and adverse reproductive outcomes, including infertility and pregnancy complications, has garnered significant attention, particularly in the context of assisted reproductive technology (ART).
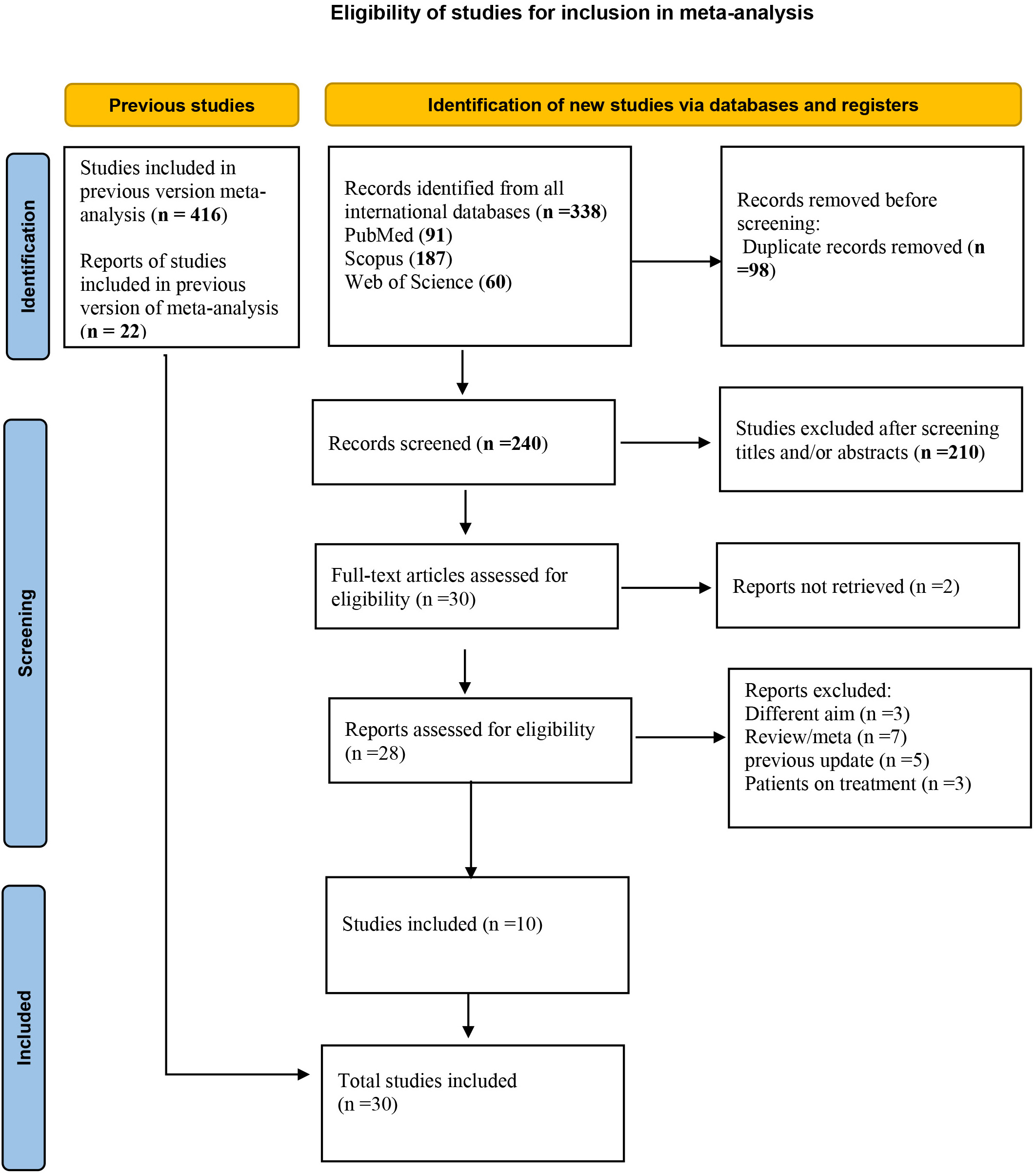
This study is a systematic review and meta-analysis designed to examine the relationship between TAI and outcomes of ART. A comprehensive literature search was conducted in PubMed, Scopus, and Web of Science databases to identify relevant studies published up to May 1, 2022. In addition, articles published between May 2022 and May 2025 were included, along with earlier studies that were part of previous meta-analyses or provided novel and relevant findings. Studies were eligible for inclusion if they compared ART outcomes between women with TAI (defined by the presence of TPOAb and/or TgAb) and euthyroid women without thyroid autoantibodies. Evaluated outcomes included clinical pregnancy, miscarriage, live birth, implantation, and fertilization rates (FR). Statistical analysis was conducted using STATA version 18, with pooled odds ratios (ORs) and 95% confidence intervals (CIs), calculated using a random-effects model. Study heterogeneity was assessed using the I2 statistic.
A total of 30 studies were included in the meta-analysis to assess the association between TAI and ART outcomes. TAI was not significantly associated with clinical pregnancy rate (CPR) (OR: 0.91; 95% CI: 0.76–1.08), miscarriage rate (MR) (OR: 1.13; 95% CI: 0.93–1.38), or live birth rate (LBR) (OR: 0.97; 95% CI: 0.78–1.22). However, significant negative associations were found between TAI and both implantation rate (IR) (OR: 0.82; 95% CI: 0.72–0.93) and FR (OR: 0.87; 95% CI: 0.83–0.90). Subgroup analysis revealed a more pronounced adverse effect of TAI on CPR among women undergoing in vitro fertilization (IVF) compared to intracytoplasmic sperm injection (ICSI). These findings suggest TAI may impair specific ART outcomes, particularly embryo implantation and fertilization.
Autoimmune thyroid disease may affect certain ART outcomes, such as a reducing FR; however, no significant difference was observed in LBRs, suggesting that it may not significantly impact the overall success of ART in terms of live births. Monitoring thyroid function in women with TAI undergoing ART is recommended by multiple endocrinology society guidelines and may offer significant clinical beneficial. This includes assessing thyroid-stimulating hormone (TSH) levels at the time of the second positive human chorionic gonadotropin (hCG) result, which confirms pregnancy.
The study has been registered on https://www.crd.york.ac.uk/prospero/ (registration number: CRD42023488835; registration link: https://www.crd.york.ac.uk/PROSPERO/view/CRD42023488835).