†These authors contributed equally.
Academic Editor: Michael H. Dahan
Background: The aim of this study was to investigate the prevalence and
characteristics of SCCmec genotypes and drug resistance of
methicillin-resistant Staphylococcus aureus (MRSA) isolated from
intensive care units (ICU) at obstetrics & gynaecology departments in a tertiary
hospital. Methods: MRSA obtained from patients admitted to the ICU were
isolated and identified by using the Vitek 2 Compact System with GP21 342 cards.
Antimicrobial susceptibility profiles and MRSA screening were determined by using
the broth microdilution method according to CLSI guidelines. Determination of
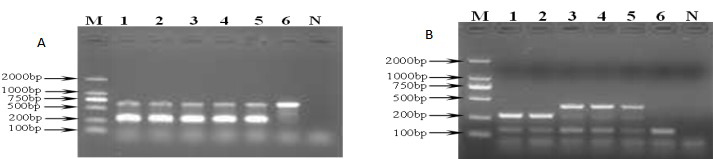
resistant genes and SCCmec genotypes were performed by multiplex PCR.
Results: Of the 283 patients evaluated, 120 (42.4%) isolates were
phenotypically and genotypically confirmed to be MRSA. Among 120 strains, 15
(12.5%) strains were SCCmec type II, 96 (80%) strains were
SCCmec type III and 9 (7.5%) strains were undifferentiated type. All MRSA
strains were recognized as multidrug resistant, exhibiting 100% resistance to
cefoxitin and oxacillin, followed by erythromycin and levofloxacin (more than
80% and 90% respectively). Different SCCmec genotypes in MRAS isolates
showed distinct antimicrobial agent patterns. SCCmec type II was highly
resistant to clindamycin (93.3%) with lower resistance to tetracycline (26.7%)
with SCCmec type III being highly resistant to gentamicin
(91.7%). Undifferentiated strains were resistant to Cotrimoxazole (77.8%).
There was a statistical difference among type II, type III and
Undifferentiated strains (P