Aim: To explore the efficacy of presetting catheter sheaths for uterine arterial embolization in the cesarean section of pernicious preplacental placenta. Materials and Methods: The clinical records of 37 patients with pernicious preplacental placenta were retrospectively analyzed. Sixteen patients who underwent cesarean section postoperative uterine artery embolization (UAE) were classified into group A, while 21 patients who received preset femoral catheterization followed with immediate UAE after the fetus was delivered by cesarean section were classified into group B. The therapeutic effects were compared. Results: The average amount of blood loss and infusion of patients in groups A and in B was 2,621 ± 626 ml and 6.23 ± 2.66 U and 1455 ± 486 ml and 3.03 ± 2.12 U, respectively (p < 0.01). One patient of group A received hysterectomy and no hysterectomy was seen in patients of group B. Conclusion: Intraoperative UAE using preset femoral artery catheterization prior to cesarean section has effectively reduced blood loss and infusion.
The concept of pernicious placental previa was initially proposed by Chattopadhyay et al. in 1993 [1]. It was defined as a special placenta previa with a previous cesarean section history, and the placenta attached to the uterine scar tissue. Pernicious placenta previa is usually complicated with placenta accreta, and the fatal hemorrhage often occurs during cesarean section, which is one of the major causes for the maternal and fetal death [2]. The intervention therapy was firstly introduced by Brown et al. in 1997 [3] as the successful treatment of postpartum hemorrhage. Cesarean section joint with uterine artery embolization (UAE) has been proven to be an effective therapy to reduce blood loss and secondary hysterectomy. However, the risk of radiation exposure for the fetus has been by far wildly widespread. The clinical application of intraoperative UAE using preset femoral artery catheterization prior to cesarean section was valued and reported as follows.
Thirty-seven near full-term pregnant patients with pernicious placenta previa complicated with placenta accreta admitted to this hospital between February 2010 and June 2016 were classified into two groups according to the different therapeutic regimes. Sixteen patients who underwent immediate UAE after cesarean section was classified into group A (control group) and another 21 patients who received preset femoral catheterization and immediate UAE under digital subtraction angiography (DSA) once the fetus was delivered through cesarean section were classified into group B (study group). The general information of the two groups is shown in Table 1. The two groups were comparable regarding the age and gestational week. This study was approved the ethic committee of The Second Affiliated Hospital of Soochow University and it conforms to the provisions of the Declaration of Helsinki (as revised in Tokyo 2004). Informed consent was obtained from each patient.
| Group | n | Age (y) | Gestational weeks (w) | Blood loss (ml) | Blood transfusion (U) | DIC | Hysterec-tomy (n) | FT (s) | CD (mGy) | Neonatal asphyxia (n) | Mean Apgar score | Neonatal weight (g) |
| A | 16 | 27.5±2.1 | 35.6±4.1 |
2621 ±626 |
6.23±2.66 |
3 | 1 | 593±243 |
578±187 | 2 | 9.450±43 | 2553.24 |
| B | 21 | 27.2±1.9 | 35.2±6.3 | 1455 ±486 | 3.03±2.12 | 0 | 0 | 126.80±31.21 | 123.47±38.40 | 1 | 9.39 |
2606.64 |
The surgeries were performed in the operation room equipped with DSA. Cesarean section was performed by obstetricians in group A. The placenta was removed once the fetus was delivered, and the hemostasis of surgical traumatic surface was achieved. When the cesarean section was completed, the Seldinger conventional right femoral artery puncture with indwelling of a 5F catheter sheath was carried out by the doctors from interventional department. The guide wire and the 5F pig-tail catheter were inserted under the guidance of DSA. The shape of internal iliac artery was visualized by angiography (Figure 1). UAE was performed by absorbable gelatin of 500-700 µm when the 5F Roberts uterine catheter (RUC) was inserted into bilateral uterine arteries (Figures 2 and 3). Upon the completion of embolization, the 5F pig-tail catheter was then inserted into renal artery level for angiography, to ensure no blood supply from the branches of ovarian artery or internal iliac artery and embolize them if necessary.
 Figure 1.
Figure 1.— The shape of bilateral internal iliac artery (black arrow) is shown under angiography by 5F pigtail catheter (white arrow).
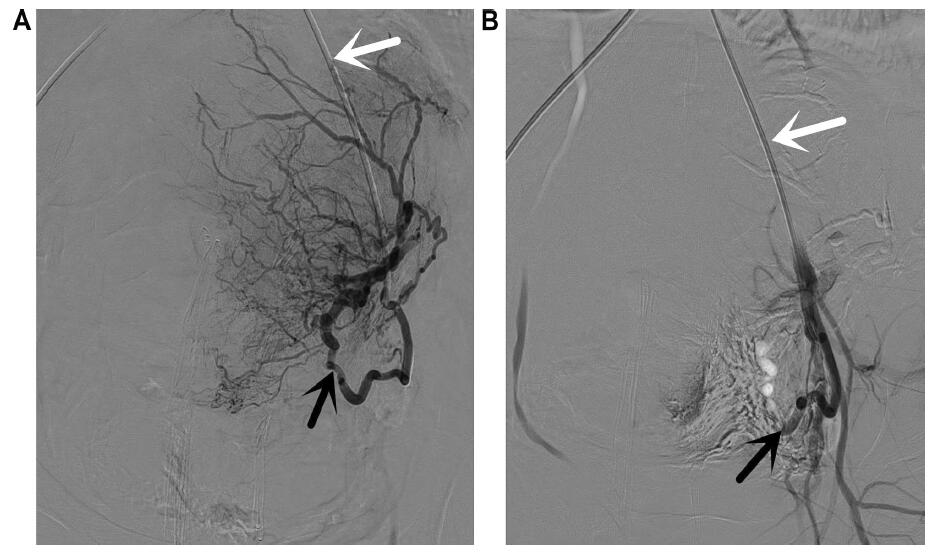 Figure 2.
Figure 2.— First episode of embolization. A: Catheterization of the left uterine artery (black arrow) with a RUC (white arrow). B: Control after gelatin sponge particle embolization of the left uterine artery (black arrow).
 Figure 3.
Figure 3.— Second episode of embolization. A: Catheterization of the right uterine artery (black arrow) with a RUC (white arrow). B: Control after gelatin sponge particle embolization of the right uterine artery (black arrow).
For group B patients, the Seldinger conventional right femoral artery puncture with indwelling of 5F catheter sheath was carried out before cesarean section, without uterine artery catheterization under DSA. After the fetus was delivered, the uterine cavity at the lower uterine segment was filled with cotton pads for pressure hemostasis; meanwhile, UAE was immediately performed with the same surgical approach as what was done for group A patients. At last, the placenta was removed by the obstetrician when the embolization was conformed to be completed.
The data was statistically analyzed by SPSS19.0. Measurement data was analyzed by χ2 test and count data was analyzed by t test. P < 0.05 was considered as statistical significance.
The average amount of blood loss and infusion of patients in groups A and in B was 2,621 ± 626 ml and 6.23 ± 2.66 U and 1,455 ± 486 ml and 3.03 ± 2.12 U, respectively (p < 0.01). Difference between groups was statistically significant. The mean fluoroscopy time (FT) in group A was 593 ± 243 seconds with the mean cutaneous dose (CD) in puerperae of 126.80 ± 31.21 mGy, and it was 578 ± 187 seconds and 123.47±38.40 mGy, respectively in group B (p > 0.05). Disseminated intravascular coagulation (DIC) occurred to three patients in group A (3/16, 18.75%), One of them receiving hysterectomy, postpartum neonatal asphyxia was observed in two newborns, the mean Apgar score of other newborns was 9.45 ± 0.43. No hysterectomy was seen in patients in group B and postpartum neonatal asphyxia was observed in one newborn (1/20, 5.00%). The mean Apgar score of the other newborns was 9.39 ± 0.78 (Table 1). Neither group had serious complications.
Cesarean section history is one of the causative factors for placenta accreta. The damage on the endometrium by cesarean section allows the invasion of villi and placenta into the myometrium or even into the uterine serous layer, which leads to the formation of placenta previa and penetrating placenta accreta. The incidence of placenta accreta has gradually increased in recent years, and 70.2% is complicated with placenta previa [4]. The risk of pernicious placenta previa complicated with placenta accreta is fairly high. Rapid and massive intraoperative hemorrhage could often occur, which seriously threatens the maternal life. Studies done by Akar et al. [5] have shown that 66%, 15%, and 6.5% patients with pernicious placenta previa suffered from hemorrhage before or after delivery with the amount of > 2,000 ml, > 5, 000 ml, and > 10,000 ml, respectively. Hysterectomy could be considered when the hemorrhage exceeds 3,000 ml with no effective control and concurrent with DIC. In the study of group A, one of the patients received embolization immediately after cesarean section was concurrent with DIC, and the blood volume was as high as 3,800 ml. The hysterectomy was performed, considering ovarian artery participate in the blood supply.
Cheng et al. [6] believed that artery embolization, rather than conventional surgical treatment, should be primarily considered as the preferred option for patients with postpartum hemorrhage and unsatisfactory conservative treatment outcome. Currently, the pelvic artery embolization technique has been broadly utilized in other countries for the treatment of postpartum hemorrhage with a success rate of 85% to 95% [7]. In this study, the success rate of intra-pelvic artery embolization technique was 97.3% (36/37), which was consistent with other reports.
The blood supply at the lower uterine segment is abundant. However, with the poor myometrial contraction, the blood sinus is difficult to close at the placenta abruption surface. Therefore, the risk of massive hemorrhage is very high during or after a cesarean section. It is especially true when the placenta is implanted into the anterior wall of lower fragment uterine; massive hemorrhage due to the damage on the placenta could be induced when the uterine is incised open. Meanwhile, the amniotic fluid could enter the blood sinus through the surgical wound and induce acute DIC, further leading to severe coagulation disorder and more extensive hemorrhage. The post-cesarean section intervention therapy might take more time and miss the timing for rescue. Therefore, UAE preformation during cesarean section is necessary. Moreover, it was reported by Descargues et al. [7] that the therapeutic effect of intraoperative embolization was significantly superior to postoperative embolization, which is consistent to what has been observed by research: the average blood volume of patients in group B was 1455 ± 486) ml, significantly lower than that in group A (2621 ± 626) ml, while the average blood transfusion in group B was significantly lower than that in group A. In addition, the long-term follow up by Descargues et al. indicated that UAE did not affect postoperative menstruation recovery and fertility, and suggested that UAE was safe for both maternal and fetal perspectives.
There was no statistically difference of FT and CD between the two groups. UAE in group B was performed in average within around 3.5 ± 1.1 minutes after the fetus was delivered and preset femoral artery catheterization saved time. Since the placenta attaching area was kept intact during the operation, there was no placenta abruption. Therefore, the risk of massive hemorrhage was further minimized. Additionally, preset femoral artery catheterization avoids fetal radiation exposure, and minimizes the risk of radiation damage. According to the literature [8], fluoroscopically-guided presetting UAE together with cesarean section brings a certain psychological burden to the newborn family and it is widespread.
In recent years, it has been reported [9] that prophylactic occlusion balloon catheters (POBCs) contributes to reduction of blood loss and preservation of the uterus in women with pernicious placenta previa complicated with placenta accreta. The complications include rupture of blood vessels, ischemia of distal extremities, reperfusion injury, and thrombosis [9]. There are fewer postoperative complications of UAE and are less symptomatic, including puncture site hematoma and ischemic pain after embolization. Severe complications include the infarction and infection in the uterine, upper segment of vagina and bladder, acute lower extremity arterial embolism, and rare radiation diseases [5]. In the current study, patients in both groups were treated with symptomatic and supportive treatments including anti-infections, uterine contraction promotion, and oral mifepristone. Lower abdominal and perineal pain with different degrees was reported by six patients after embolization, and the pain was relieved around one week later. Transient postoperative increased body temperature was reported by five patients, with the highest temperature of 38.5°C, and alleviated by physical cooling method. No other severe complication was found. The patients were followed up for one to three months postoperatively; menstruation recovered to normal in 35 patients except in one. The serum hCG level and B ultrasound uterine examination were all normal for the patient with abnormal menstruation, and continue to be followed up to five months, and normal menstruation was restored.
Intraoperative UAE using preset femoral artery catheterization prior to cesarean section is safe and reliable. It effectively reduced blood loss and blood transfusion. Meanwhile, the radiation exposure to fetus was limited.
