Background: Cases of infective endocarditis (IE) with 30 mm
vegetations are rare and are associated with high mortality. Clinical experience,
clear therapeutic standards, and outcome evidence about these cases are still
lacking. Methods: Detailed clinical data from patients suffering from IE
complicated with 30 mm vegetations were collected from a hospital medical
record system. Age- and sex-matched IE cases with 10–20 mm vegetations were used
as a control group. Results: Twenty-two patients with 30 mm IE
vegetations confirmed by biopsy and transthoracic echocardiography (TTE) were
included. Thirteen (59.0%) patients had basic cardiac diseases, mainly
congenital heart disease (CHD), rheumatic heart disease, and device-related
issues. Fever (81.8%), heart murmur (86.4%), heart failure (86.4%), and
embolism (50.0%) were common clinical manifestations and complications. TTE
showed the diameter of vegetations was 34.5 (30.0–39.8) mm. The vegetations were
usually accompanied by severe valvular regurgitation and pulmonary hypertension,
and were most often located in the mitral valve (38.4%). Laboratory examinations
indicated anemia, hypoalbuminemia, heart failure and inflammation. The rate of
positive blood culture was 68.2%. Streptococcus viridans was the most frequent
pathogen (26.7%). All individuals underwent vegetectomy and valve replacement or
repair surgery, within 2 days of diagnosis. Compared with 10–20 mm vegetations
group, 30 mm vegetations group had more complicated basic cardiac diseases,
more special microbial infection, higher levels of procalcitonin (PCT) and
D-dimer, more common heart failure and embolism. They received more biological
valve replacements, and had longer intensive care unit length of stay (ICU-LOS).
A few patients developed significant postoperative adverse events, including
intracerebral hemorrhage (ICH), septic shock, and new symptomatic thrombosis.
Re-exploratory thoracotomy was performed in two cases. All patients survived
during 6-month follow-up without IE recurrence in 30 mm vegetations group,
while there was one death and one recurrence in the 10–20 mm vegetations group.
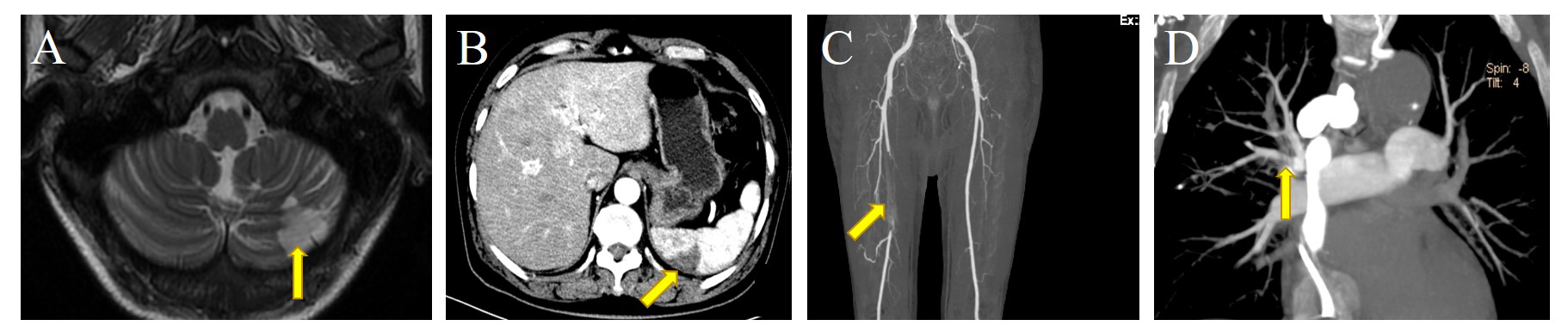
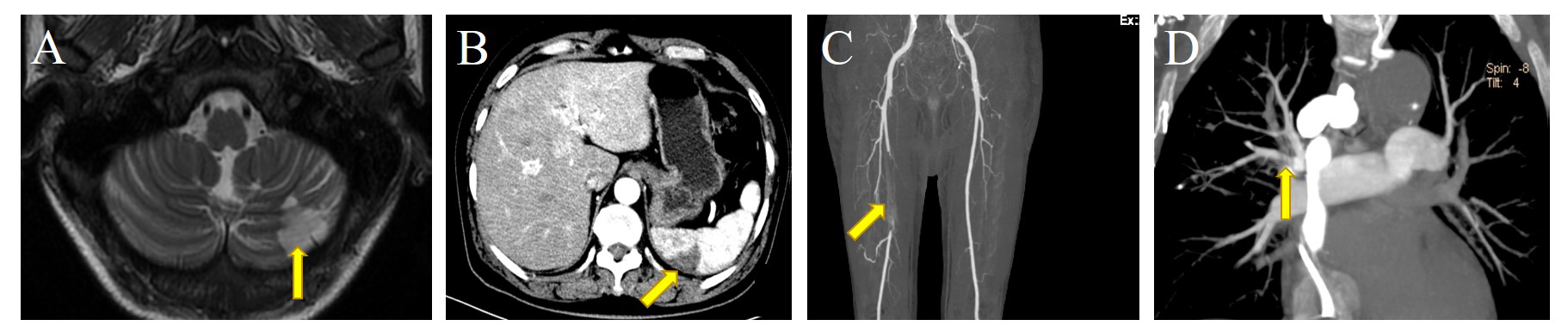
Conclusions: For IE complicated with 30 mm vegetations, clinical
characteristics are diverse and vegetations on TTE are prone to misdiagnosis as
thrombus or tumors. This article also emphasizes the use of 30 mm IE
vegetations as an independent indication for early surgery to improve prognosis.