†These authors contributed equally.
Academic Editors: Christian Hengstenberg and George Dangas
Background: The feasibility and long-term outcomes of the
CrossBoss/Stingray for treating coronary chronic total occlusions (CTO) with
distal diffuse disease landing zone remain unclear. Methods: Consecutive
CTO patients with distal diffuse lesions that underwent percutaneous coronary
intervention by the CrossBoss/Stingray system at Xijing Hospital from April 2016
to October 2020, were included. Patients were analyzed by two groups according to
the extent of stenosis in the distal landing zone:
50%–70% stenosis (moderate stenosis group)
and
Chronic total occlusions (CTOs) are found approximately in 20% to 50% of patients with symptomatic coronary artery disease [1, 2], but the optimal strategies and techniques for its treatment remain in debate [3, 4]. With the development of coronary interventional techniques and interventional devices, antegrade dissection and re-entry (ADR) has been a widely applied strategy for the percutaneous coronary intervention (PCI) of CTO [5]. Studies have shown that the use of device based ADR, namely with the CrossBoss/Stingray system (Boston Scientific, Marlborough, MA, USA), has increased the success rate of ADR-based CTO PCI [6].
Theoretically, long lesion lengths (
In the present study, we aimed to (1) evaluate the success rate and long-term
clinical outcomes of the CrossBoss/Stingray system for CTO with a distal diffuse
disease landing zone. (2) Compare the success rate and clinical outcomes between
patients with moderate (50%–70%) or severe stenosis (
The study was a prospective, single center, observational study. Consecutive patients with a distal diffuse disease that undergoing PCI for CTO lesions using the CrossBoss/Stingray system, who were admitted to Xijing Hospital (Xi’an, China) from April 2016 to October 2020, were included in the present study. The study protocol was approved by the local institutional review board of Xijing Hospital and complied with the declaration of Helsinki. All written informed consents were obtained.
Patients with CTO were treated with aspirin (100 mg/day) and clopidogrel (75
mg/day) or ticagrelor (180 mg/day) before the procedure for at least 5 days.
Patients were maintained on aspirin 100 mg and clopidogrel 75 mg or ticagrelor
180mg daily after PCI. Heparin was used as the anticoagulant to maintain an
activated clotting time of
Patients were stratified according to the diameter stenosis of the distal
diffuse disease landing zone into two groups: (1) stenosis of the distal landing
zone between 50%–70% (moderate stenosis group). (2) Stenosis of the distal
landing zone
The primary efficacy outcome was the frequency of true lumen guidewire placement distal to the CTO (technical success). The composite endpoint of all-cause death, any stroke, or any revascularization was also explored in the current study. Any revascularization was defined as repeat revascularization including the target lesion revascularization, target vessel revascularization, and non-target vessel revascularization, regardless of the strategy of revascularization (PCI or CABG). Clinical outcomes were collected by telephone or clinic visit, and the events were adjudicated by an independent clinical event committee.
Continuous variables are presented as mean
Between April 2016 and October 2020, 153 consecutive CTO patients underwent PCI
using the CrossBoss/Stingray system, of whom 91 (59.5%) patients were with the
distal diffuse disease landing zone. Among those 91 patients, 32 patients were
characterized in the moderate stenosis group and 59 were in the severe stenosis
group (Fig. 1). The baseline clinical and procedural characteristics are shown in
Table 1. Overall, the mean age of the patients was 61.7
 Fig. 1.
Fig. 1.The study flow chart. Enrollment and clinical follow-up of CTO patients with a diffuse distal disease landing zone who underwent PCI using the CrossBoss/Stingray system in the present study. Data of 153 consecutive CTO patients who underwent PCI using the CrossBoss/Stingray system were prospectively collected, of whom 91 (59.5%) patients were with a diffuse distal disease landing zone and were finally included in the study.
| Variables | Overall (n = 91) | Moderate stenosis group (n = 32) | Severe stenosis group (n = 59) | p |
| Age | 61.7 |
62.3 |
61.4 |
0.940 |
| Gender | ||||
| Male | 85.7 (78/91) | 90.6 (29/32) | 83.1 (49/59) | 0.531 |
| Diabetes | 37.4 (34/91) | 37.5 (12/32) | 37.3 (22/59) | 0.984 |
| Insulin treatment | 18.7 (17/91) | 18.8 (6/32) | 18.6 (11/59) | 0.990 |
| Hypertension | 65.9 (60/91) | 68.8 (22/32) | 64.4 (38/59) | 0.676 |
| Dyslipidemia | 61.5 (56/91) | 71.9 (23/32) | 55.9 (33/59) | 0.136 |
| Current smoking | 28.6 (26/91) | 28.1 (9/32) | 28.8 (17/59) | 0.945 |
| Prior CABG | 2.2 (2/91) | 3.1 (1/32) | 1.7 (1/59) | 0.657 |
| Prior stroke | 11 (10/91) | 9.4 (3/32) | 11.9 (7/59) | 0.717 |
| Prior MI | 30.8 (28/91) | 31.3 (10/32) | 30.5 (18/59) | 0.942 |
| PVD | 5.6 (5/90) | 6.3 (2/32) | 5.2 (3/58) | 1.000 |
| NYHA classification | 0.338 | |||
| 1 | 13.5 (12/10) | 15.6 (5/32) | 12.3 (7/57) | |
| 2 | 71.9 (64/10) | 78.1 (25/32) | 68.4 (39/57) | |
| 3 | 11.2 (10/89) | 3.1 (1/32) | 15.8 (9/57) | |
| 4 | 3.4 (3/89) | 3.1 (1/32) | 3.5 (2/57) | |
| LVEF | 51% |
49% |
52% |
0.116 |
| Creatine | 97.0 (82.8–110.0) | 99.5% (84.3–109.3) | 96.0 (80.5–110.8) | 0.746 |
| J-CTO score | 2.5 |
2.3 |
2.6 |
0.297 |
| Target vessel | 0.629 | |||
| LAD | 39.6% (36/91) | 15.4% (14/32) | 24.2% (22/59) | |
| LCX | 4.4% (4/91) | 2.2% (2/32) | 2.2% (2/59) | |
| RCA | 56.0% (51/91) | 17.6% (16/32) | 38.5% (35/59) | |
| Disease type | ||||
| Single vessel disease | 17.6% (16/91) | 21.9% (7/32) | 15.3% (9/59) | 0.632 |
| Two vessels disease | 23.1% (21/91) | 25.0% (8/32) | 22.0% (13/59) | 0.636 |
| Three vessels disease | 59.3% (54/91) | 53.1% (17/32) | 62.7% (37/59) | 0.341 |
| Number of CTO lesions | 1.4 |
1.3 |
1.4 |
0.552 |
| Procedure time (min) | 110.5 |
127.5 |
102.2 |
0.109 |
| IVUS guidance | 39.6% (36/91) | 34.4% (11/32) | 42.4% (25/59) | 0.456 |
| P2Y12 inhibitors at discharge | 0.110 | |||
| Clopidogrel | 38.9% (35/90) | 51.6% (16/31) | 32.2% (19/59) | |
| Ticagrelor | 61.1% (55/90) | 48.4% (15/31) | 67.8% (40/59) | |
| DAPT duration | 0.106 | |||
| 33.0% (30/91) | 28.1% (9/32) | 35.6% (21/59) | ||
| 61.5% (56/91) | 59.4% (19/32) | 62.7% (37/59) | ||
| CABG, coronary bypass artery grafting; CTO, chronic total occlusions; LAD, left anterior descending artery; LCX, left circumflex artery; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NYHA, New York Heart Association; PVD, peripheral vascular disease; RCA, right coronary artery. | ||||
Among the total 153 consecutive CTO patients, technical success was achieved in 86.3% (132/153) patients. Compared to patients with a diffuse landing zone, patients with a good landing zone had a higher technical success rate (90.3% [56/62] vs. 79.1% [72/91], p = 0.066). Among patients with a diffuse landing zone, the technical success rates were comparable between the moderate stenosis group and the severe stenosis group: 78.1% (25/32) and 79.7% (47/59), respectively (p = 0.608) (Table 2). No coronary artery perforation occurred among all patients. One cardiovascular death occurred after 3 days of the index procedure during the hospitalization. No other adverse events occurred in hospital. An example of using the Corssboss/Stingray system for a LAD CTO patient with a distal diffuse disease landing zone is shown in Fig. 2, and an RCA CTO case is shown in Fig. 3.
| Endpoint | Overall (n = 91) | Moderate stenosis group (n = 32) | Severe stenosis group (n = 59) | p |
| Technical success | 79.1% (72/91) | 78.1% (25/32) | 79.7% (47/59) | 0.608 |
| Composite endpoints | 50.4% (39/91) | 45.1% (14/32) | 54.3% (25/59) | 0.797 |
| All-cause death | 16.6% (10/91) | 9.7% (3/32) | 21% (7/59) | 0.670 |
| Cardiovascular death | 12.1% (7/91) | 6.7% (2/32) | 15.6% (5/59) | 0.660 |
| Any revascularization | 36.5% (31/91) | 38.5% (12/32) | 36.3% (19/59) | 0.525 |
| Target vessel revascularization | 12.8% (9/91) | 17.4% (5/32) | 10.8% (4/59) | 0.158 |
| Target lesion revascularization | 11.8% (8/91) | 14.5% (4/32) | 10.8% (4/59) | 0.314 |
| Any stroke | 1.1% (1/91) | 0% (0/32) | 1.7% (1/59) | 0.461 |
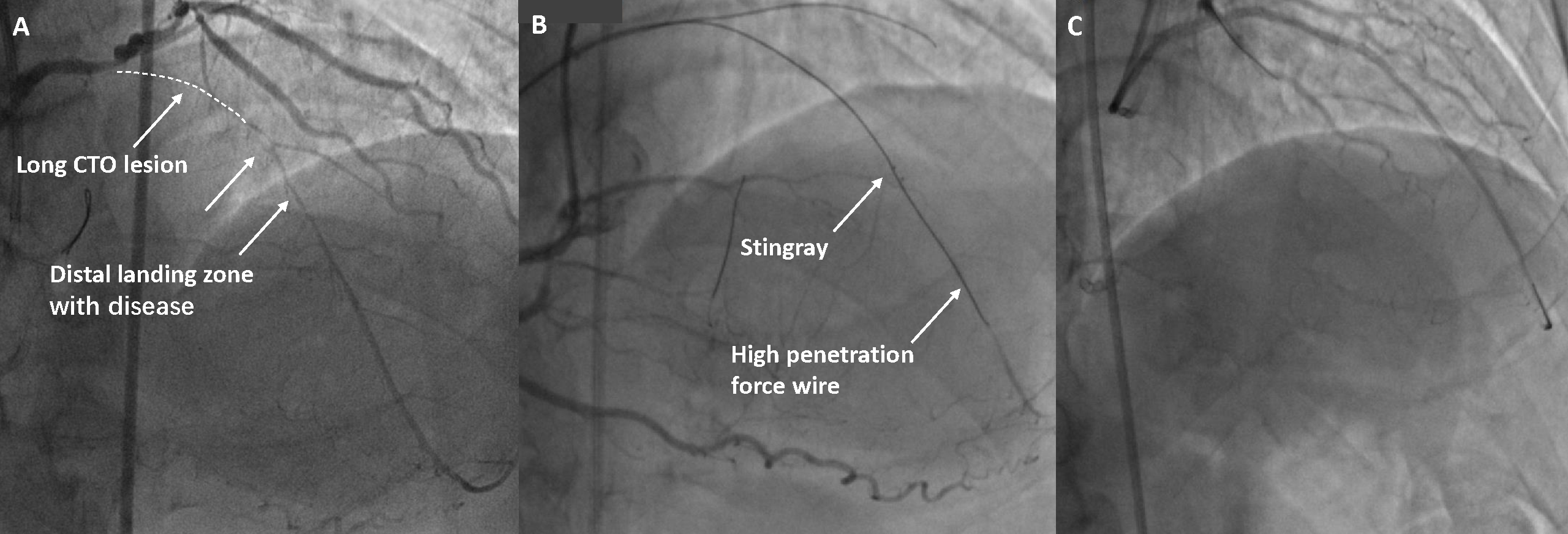 Fig. 2.
Fig. 2.Example of using the Corssboss/Stingray for a LAD CTO case. (A) Proximal LAD had a long CTO with a diffuse lesion in the distal landing zone. (B) The Stingray was exchanged into the vessel, inflated, and orientated with the target vessel on the left of the balloon. A high penetration force, tapered tip wire (Conquest Pro 12) was used to re-enter. (C) Final result after stent deployment and optimization. CTO, chronic total occlusion; LAD, left anterior descending artery.
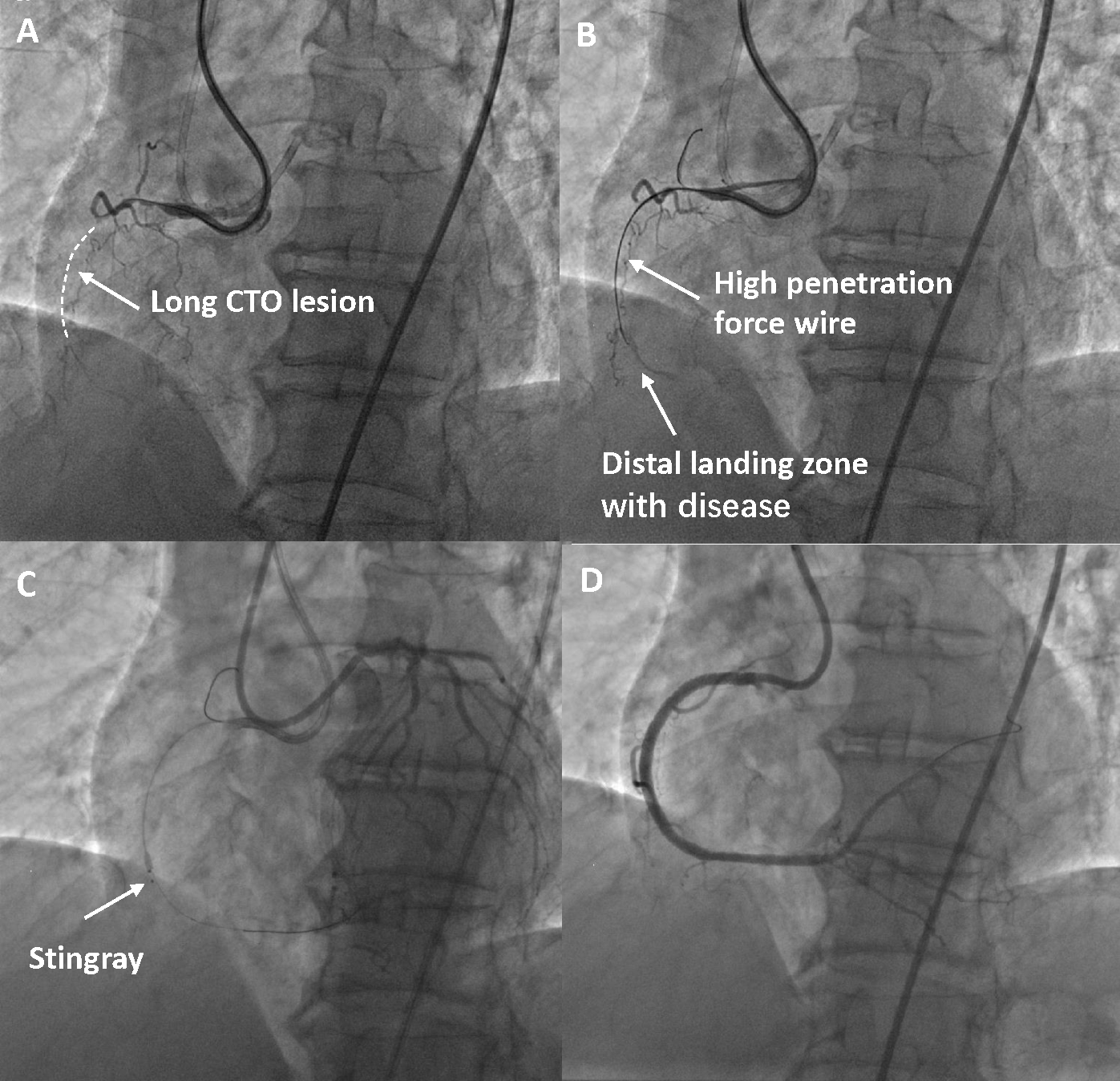 Fig. 3.
Fig. 3.Example of using the Corssboss/Stingray for an RCA CTO case. (A) There is a long CTO lesion of the middle RCA with a diffuse lesion in the distal landing zone. (B) A high penetration force wire advances into the CTO and beyond the distal cap but is in the subintimal space. (C) The Stingray is exchanged into the vessel, inflated, and orientated with the target vessel. (D) Final result after stent deployment and optimization. CTO, chronic total occlusion; RCA, right coronary artery.
Clinical outcomes were collected by telephone (58%) or clinic visit (42%). The median duration of follow-up was 29.0 months (IQR: 21.0–36.5) overall, 29.5 months (IQR: 23.5–36.3) in the moderate stenosis group, and 29.0 months (IQR: 20.0–38.0) in the severe stenosis group, respectively. The estimated rate of the composite endpoint was 50.4% in the overall population (Fig. 4). The rates of individual components were as follows: all-cause death 16.6%, any stroke: 1.1%, and any revascularization 36.5%. The incidences of the composite endpoint were not significantly different between the 2 groups (45.1% in the moderate stenosis group and 54.3% in the severe stenosis group, respectively, p = 0.797) (Table 2).
 Fig. 4.
Fig. 4.
Kaplan-Meier curves for the composite endpoint (all-cause death,
any stroke, or any revascularization) in patients with stenosis of the distal
landing zone between 50%–70% (moderate stenosis group, blue line) and those
with stenosis of the distal landing zone
The present study for the first time evaluated the feasibility and long-term outcomes of CrossBoss/Stingray for CTO with the diffuse distal disease. The main finding of the present analysis can be summarized as follows: (1) CTO patients with the distal diffuse disease landing zone (59.5%) are relatively common. (2) CrossBoss/Stingray had a relatively high technical success rate (79.1%) in patients with the distal diffuse disease landing zone. (3) Similar and acceptable technical success rates were observed between patients with severe stenosis at the distal landing zone and those with moderate stenosis. (4) In CTO patients with a distal diffuse disease landing zone, the rate of the long-term composite endpoint of all-cause death, any stroke, or any revascularization was high (50.4%), which was mainly driven by a high rate of any revascularization (36.5%).
PCI of CTO is a major challenge for interventional cardiologists [10]. It
remains a hot research topic in the field of interventional cardiology, and
several interventional techniques, as well as devices, have been reported in the
past few years. The ADR strategy was preferred in patients with defined proximal
cap anatomy, longer length (
The commonest CTO PCI procedural complication is perforation [12], however,
there was no coronary artery perforation in our study. This favorable safety
profile of CrossBoss/Stingray system might be due to the cases recorded in the
current analyses being after the initial training process and mostly performed by
the experienced operators (
Despite previous studies have demonstrated that successful CTO PCI is effective
on the relief of angina [14, 15], the debate is ongoing with respect to the net
clinical benefit of successful CTO PCI, especially after the release of the EURO
CTO trail [16] and the DECISION CTO trial [17, 18]. In our present analysis, we
observed a relatively high rate of the composite endpoint of all-cause death, any
stroke, or any revascularization with a median follow-up of 29 months, which was
mainly driven by the high rate of any revascularization. The rate of all-cause
mortality was higher than previous studies [17, 19], indicating the high-risk
feature of this challenging population. In our study, the majority of patients
had multivessel disease (2 vessels disease: 23.1%, 3 vessels disease: 59.3%).
The number of diseased vessels was 2.4
Finding a good re-entry zone is crucial for patients with poor quality distal vessels. The suitability of a re-entry zone could be affected by multiple factors, including calcification, bending, plaque load/thickness, lumen size, hematoma size, distal lumen pressure, stability of Stingray balloon, and operator experience [11]. The preprocedural CT is always useful to find a suitable re-entry area. Preprocedural analysis with CT could help us decide on a good re-entry zone based on evaluation of the thickness of the plaque and calcium location, enhanced with angiographic coregistration [23]. In the present study, preprocedural CT was available in 53 cases, providing useful information to find a good re-entry zone to achieve a high success rate of CTO PCI.
CTO with severe distal diffuse disease always represents a small distal lumen,
which is more challenging to re-enter. In the present study, we compared the
technical success of CrossBoss/Stingray system for CTOs with distal moderate
stenosis (50%–70%) landing zone and with severe stenosis (
To our knowledge, this is the first piece of clinical data to specifically
investigate the use of CrossBoss/Stingray devices in CTOs with distal diffuse
landing zone. We found a high success rate using CrossBoss/Stingray system, even
for these very difficult cases (49 cases were with J-CTO
The present study was a single center experience with relatively small sample size, and the external validity of our experience is restricted. Clinical outcomes were collected mostly by telephone calls and angiography follow-up was not mandatory. However, according to the aim of the present study, the technical success may be more relevant for evaluating the efficacy and safety for expanding the indication of the CrossBoss/Stingray system. Prospective, multicenter, larger scale, with angiography follow-up trials, were warranted in the future.
The present study showed that in CTO with a distal diffuse landing zone, the use
of CrossBoss/Stingray system was safe and had an acceptable success rate. No
significant difference in technical success rate between the moderate stenosis
group (50%–70%) and the severe stenosis group (
LT and CL had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. RW, GC and FM contributed to the data collection, analysis and interpretation, and the writing of the manuscript. YL, ZY, BW, HG, CG, CL and LT contributed substantially to study design, the data analysis and interpretation, and the critical revision of the manuscript. All authors read and approved the final manuscript.
The study protocol was approved by the local institutional review board of Xijing Hospital and complied with the declaration of Helsinki. All written informed consents were obtained.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
