Academic Editors: Giuseppe Biondi Zoccai and Victor L. Serebruany
Background: A potential relationship between oral health and
cardiovascular diseases has been proposed. However, uncertainty remains as to
whether there is sufficient data to support this association. This review aims to
appraise the relationship between apical periodontitis and cardiovascular disease
based on data from observational studies. Methods: The databases Medline
(via PubMed) and EMBASE (via Scopus) were searched up to August 2020 for
observational studies (case-control, cross-sectional, and cohort) assessing the
association of apical periodontitis with cardiovascular disease among adults.
Pooled relative risk/odds ratio and 95% confidence interval (CI) were estimated
using a random-effects model. Sensitivity analyses and random-effects
meta-regressions were performed. Results: The initial search yielded
2537 documents, of which 15 were eligible for inclusion, including 8
cross-sectional studies, 5 case-control studies, and 2 cohort studies. The
majority of studies enrolled both men and women, with mean age ranging from 41 to
66 years. In cross-sectional studies, the presence of apical periodontitis was
significantly associated with cardiovascular disease with a combined odds ratio
of 1.53 (95% CI: 1.02–2.29, p = 0.039; I
Cardiovascular diseases, including peripheral arterial disease, ischemic heart disease, heart failure, stroke, and several other cardiac and vascular disorders, are the leading cause of death worldwide and are a major cause of disability and low quality of life [1, 2, 3]. Cardiovascular diseases exert a significant personal, social, and economic burden; this is particularly important in older people. In 2019, ischemic heart disease and stroke were the top-ranked causes of disability-adjusted life-years after the age of 50 [1]. These two clinical events (ischemic heart disease and stroke) share the same underlying chronic and progressive cause—atherosclerotic vascular disease [4]; which is a dynamic and gradual process of endothelial dysfunction and chronic low-grade inflammation [5, 6].
Apical periodontitis is defined as a chronic inflammatory process surrounding the apex of a root, being primarily a consequence of microbial infection of the periradicular tissues [7, 8]. The prevalence of apical periodontitis has been increasing in the last decade in teeth with and without endodontic treatment [9]. Notwithstanding, the prevalence of apical periodontitis is high (33%) in root canal-treated teeth [10].
Over the last decades it has been suggested that the combination of some physiopathological mechanisms, namely inflammation, apical periodontitis and other chronic periodontal diseases may potentiate the progression of the atherosclerotic process and incite acute cardiovascular events [4]. Previous cross-sectional [11, 12] and longitudinal [13] studies showed a positive association between apical periodontitis and cardiovascular disease, yet there are also case-control [14] and cross-sectional [15, 16] studies that did not report a significant association. A recent umbrella review summarizing the results of four systematic reviews [17, 18, 19, 20] concluded that the association between cardiovascular disease and apical periodontitis is weak [21], yet only one systematic review included meta-analysis [17]. Aminoshariae et al. [17] conducted a meta-analysis summarizing data derived from three cohort studies and concluded that the risk ratio of the incident of cardiovascular disease was not significantly different between those with and without apical periodontitis. The present systematic review and meta-analysis aims to augment existing knowledge by including other observational studies in addition to cohort studies, such as cross-sectional and case-control studies to the search strategy to estimate the relationship between apical periodontitis and cardiovascular disease based on data from observational studies.
The systematic review and meta-analysis follows the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) and Meta-analyses of Observational Studies in Epidemiology. Two reviewers performed all selection and data extraction steps (e.g., study selection, data extraction, and methodological quality assessment) independently. Any disagreement between reviewers was resolved by consensus or consulting a third reviewer. The study protocol was previously registered on PROSPERO (CRD42020204379).
A comprehensive computerized literature search of the databases Medline (via PubMed) and EMBASE (via Scopus) (from inception to August 2020) was conducted using free-text terms based on the PICO strategy (Participants: human subjects; Interventions (exposure): Apical periodontitis or endodontic infection or necrotic teeth; Comparator: adult subjects without apical periodontitis (number of radiolucent periapical lesions = 0); Outcomes: cardiovascular disease). The reference list of previous reviews and original studies on the topic were manually checked to determine other studies that may be eligible.
Observational studies assessing the association of apical periodontitis with cardiovascular disease were eligible. Search terms included (apical periodontitis OR periapical periodontitis OR apical lesion OR apical infection OR periapical lesion OR periapical infection OR periapical lesion OR endodontic infection) AND (cardiovascular disease OR coronary heart disease OR coronary artery disease OR atherosclerosis OR vascular disease OR cerebrovascular disease OR stroke OR heart failure OR hypertension OR angina pectoris OR myocardial infarction). Detailed search strategy per database is provided in Supplementary Table 1.
The selection of the studies was conducted using the following inclusion
criteria: (i) involved adults (
Data were extracted using a standardized form and coded as follows: (a) first author and year of publication; (b) country; (c); study design (d) sample size and age of the participants (years); (e) sex (% of men and women); (f) type of cardiovascular disease; (g) diagnosis or assessment of cardiovascular disease; (h) type of evaluation of the apical periodontitis (e.g., radiography, tomography); (i) type of apical lesion; and, (j) results (e.g., correlation coefficient, odds ratio). Additionally, if data were unclear or were not available in the published articles, the corresponding author was contacted by e-mail to request the required information. The methodological quality of the studies was determined applying the National Heart, Lung, and Blood Institute (NIH) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [24].
Pooled relative risk and 95% confidence interval (CI) (random-effects) model
were estimated based on the Der Simonian and Laird method, separately for
cross-sectional and longitudinal studies (case-control and cohort studies) [23].
Odds ratio (OR) estimates are reported for cross-sectional and case control
studies, while risk ratio (RR) was used for cohort studies. Fixed effects models
were used when heterogeneity was not important or moderate. Heterogeneity across
studies was assessed using the I
A sensitivity analysis was performed to determine the robustness of the
aggregate estimates and to detect whether any specific studies represent a large
percentage of heterogeneity. Random-effects meta-regressions were used to
correlate the results with the age and percentage of males, as those variables
might also give an explanation for the observed heterogeneity. Finally,
publication bias was assessed by visual examination of the funnel plots and Egger
tests, considering that a p-value
Fig. 1 illustrates the process of search and selection of studies. The initial literature search identified a total of 2715 documents (Supplementary Table 1). After removing 178 duplicates, 2537 relevant titles and abstracts were reviewed prior to downloading the full-text versions for further analysis. Consequently, 2462 documents were excluded, and 75 were eligible for full-text review. A total of 15 studies met the criteria to be included in the review and were incorporated in the meta-analysis (Fig. 1).
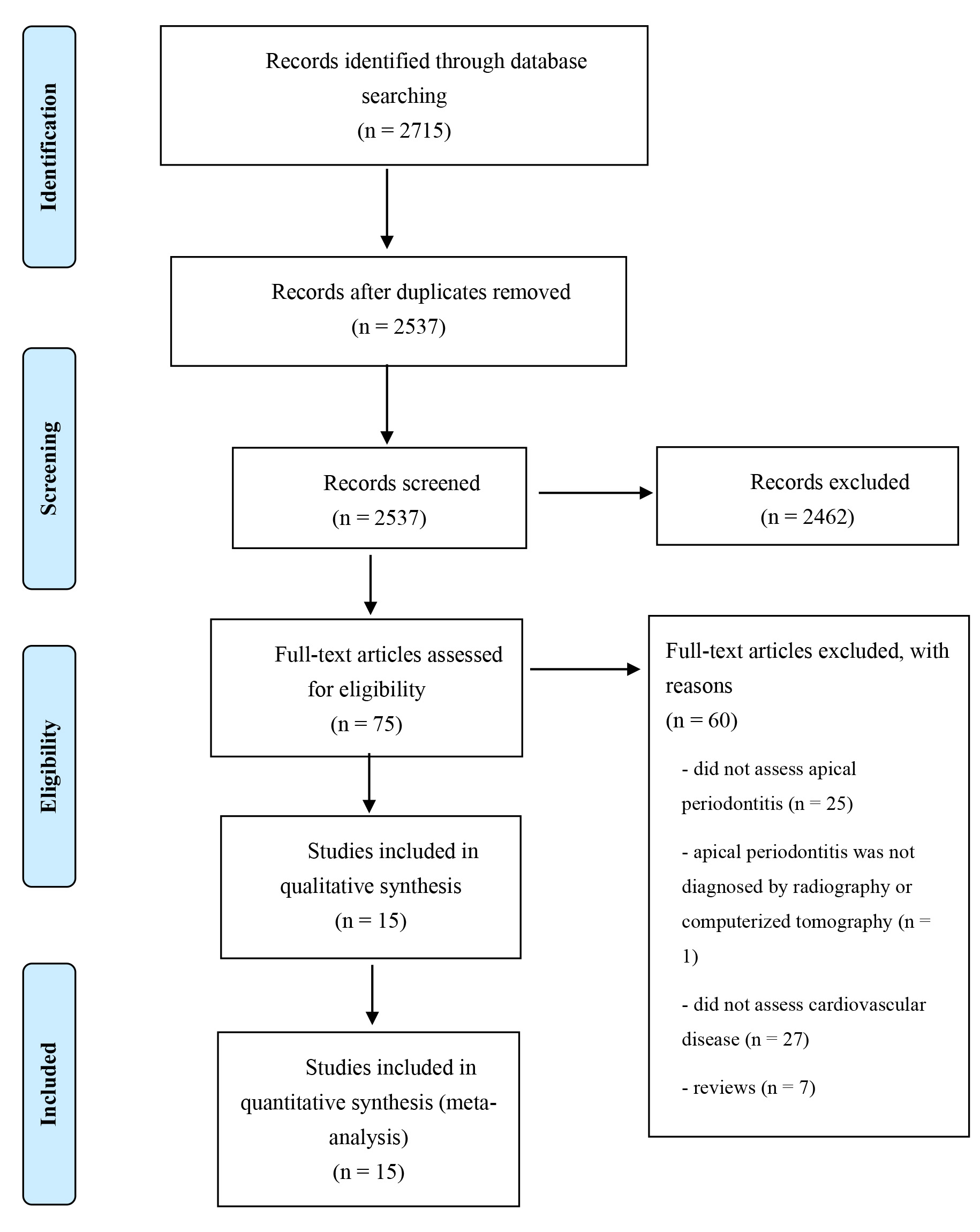 Fig. 1.
Fig. 1.Flow chart of identified, included, and excluded studies.
A general description of the 15 studies (8 cross-sectional studies, 5 case-control studies, and 2 cohort studies) included in the meta-analysis is shown in Table 1 (Ref. [11, 12, 13, 14, 15, 16, 28, 29, 30, 31, 32, 33, 34, 35, 36]). The 15 studies enrolled 673 083 adults. The sample size of the included studies ranged from 103 [11] to 666 768 [28] participants. The majority of studies enrolled both men and women; one study included only men [29], while another study included only women [16]. Participant’s age ranged from 41 [30] to 66 [16] years old; two studies [15, 28] did not specify the age of the sample (Table 1). The studies were accomplished in Europe (n = 9, 60%), USA (n = 4, 26.7%), and Brazil (n = 2, 13.3%). The great majority of studies diagnosed apical periodontitis using panoramic radiography, in some cases supplemented with periapical radiography. Regarding cardiovascular disease, six studies [11, 15, 16, 29, 31, 32] analysed the association between apical periodontitis and coronary artery disease (also known as coronary heart disease), and two [33, 34] with acute myocardial infarction. Four studies [12, 28, 30, 35] defined cardiovascular disease as an umbrella term including, for instance, cardiovascular disease-related systemic diseases in accordance with the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes [12] or according to the ICD-9-10 [35] (Table 1).
| Authors/Year | Country | Type of study | Sample | Age (years) | Gender | Type of evaluation | Type of cardiovascular disease | Covariates |
| An et al., 2016 [12] | USA | Pair-matched, cross-sectional study | 364 (182 per group) | 49.1 |
26.9% men | Digital radiography | Cardiovascular disease* | Race/ethnicity and hypertension |
| Caplan et al., 2006 [29] | USA | Cohort study (median follow-up: 24.0 yrs) | 708 | 47.4 | men | Dental radiographic series | Coronary heart disease | – |
| Correia-Sousa, et al., 2015 [30] | Portugal | Cross-sectional study | 421 | 41 |
43% men | Panoramic radiography | Cardiovascular disease** | – |
| Costa et al., 2014 [11] | Brazil | Cross-sectional study | 103 | 61.9 |
50.5% men | Periapical radiography | Coronary artery disease | Sociodemographic, clinical, and laboratory variables |
| Frisk et al., 2003 [16] | Sweden | Cross-sectional study | 1056 | 66.0 |
100% women | Panoramic radiography | CHD (angina pectoris and/or myocardial infarction) | – |
| Gomes et al., 2016 [13] | USA | Cohort study (mean follow-up 17.4 yrs) | 278 | 55.0 |
51.4% men | Panoramic radiography | Cardiovascular events (e.g., angina, myocardial infarction) | Sociodemographic, medical, and dental variables |
| Liljestrand et al., 2016 [36] | Finnish | Cross-sectional study | 508 | 62.1 |
65.0% men | Panoramic radiography | Acute coronary syndrome | Age, sex, smoking, diabetes, body mass index, alveolar bone loss, and number of teeth |
| Messing et al., 2019 [28] | USA | Cross-sectional study | 666 768 | 18 to 65 (mean age not specified) | Not specified | Radiography | Cardiovascular disease*** | – |
| Meurman et al., 2017 [31] | Finland | Case-control study | 473 (231 cases, 242 controls) | 59.6 |
63.5% men | Panoramic radiography | Coronary artery disease | – |
| Oliveira et al., 2017 [15] | Brazil | Cross-sectional study | 1346 | Not specified | 32.5% men | Radiography | Coronary artery disease | – |
| Pasqualini et al., 2012 [32] | Italy | Case-control study | 100 (51 cases, 49 controls) | 47.4 |
79% men | Panoramic radiography | CHD (angina pectoris and/or myocardial infarction) | Clinical factors, family history, and smoking |
| Segura-Egea et al., 2010 [14] | Spain | Case-control study | 91 (40 cases, 51 controls) | 56.8 |
47% men | Panoramic radiography | Hypertension | – |
| Virtanen et al., 2017 [35] | Sweden | Cross-sectional study | 120 | 52.1 |
47.5% men | Panoramic and periapical radiography | Cardiovascular disease§ | Age, gender, income, smoking, and periodontitis |
| Willershausen et al., 2009 [33] | Germany | Case-control study | 250 (125 cases, 125 controls) | 62.6 |
81.2% men | Panoramic and periapical radiography | Acute myocardial infarction | – |
| Willershausen et al., 2014 [34] | Germany | Case-control study | 497 (248 cases, 249 controls) | 62.9 |
76.5% men | Panoramic and peri-apical radiography | Acute myocardial infarction | Age and gender |
| * Cardiovascular disease-related systemic diseases according to the
International Classification of Diseases, Ninth Revision, Clinical Modification
(ICD-9-CM) codes (e.g., coronary heart disease, cerebrovascular disease,
peripheral arterial disease, rheumatic heart disease, congenital heart disease,
etc); ** Coronary heart disease, stroke, hypertension, atherosclerosis, and
myocardial infarction; *** hypertension, rheumatic fever, heart murmur, mitral
valve prolapse, myocardial infarction, cerebrovascular accident, cardiac surgery,
chest pain, angina, irregular/rapid heartbeat, palpitations, pacemaker, heart
valve disease, presence of blood clots, infective endocarditis, coronary artery
disease, congestive heart failure, atrial fibrillation, heart block, cardiac
arrhythmia, and deep vein thrombosis; § Cardiovascular disease
according to the World Health Organization International Classification of
Diseases (ICD-9-10); | ||||||||
In cross-sectional studies (n = 8), the presence of apical periodontitis was
significantly associated with a higher pooled risk estimate of cardiovascular
disease (OR = 1.53; 95% CI: 1.02–2.29, p = 0.026); however, there was
substantial heterogeneity in the estimates (I
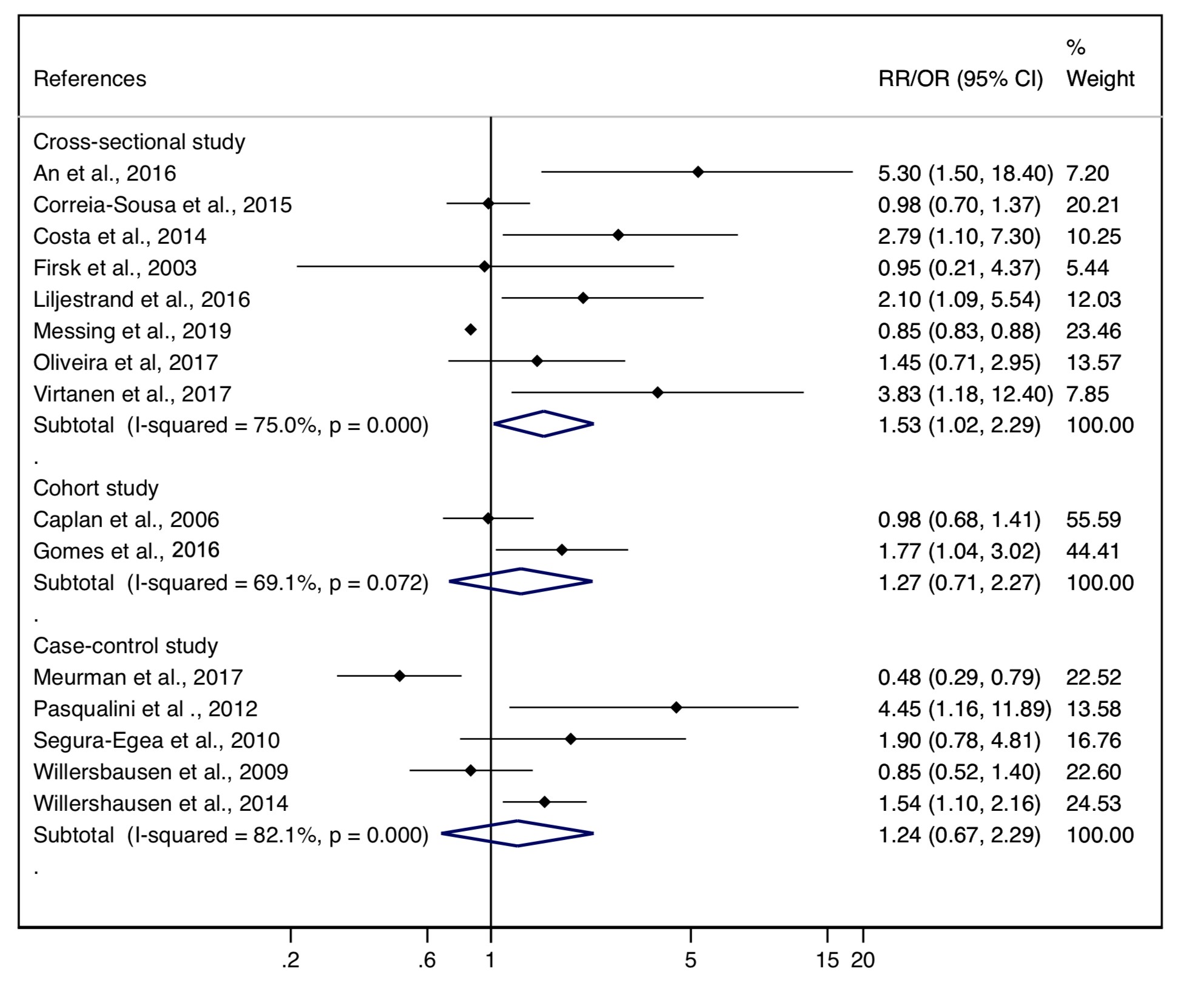 Fig. 2.
Fig. 2.Forest plot of the pooled odds (OR) and risk (RR) ratio for cardiovascular disease in cross-sectional, cohort, and case-control studies.
The combined odds ratio of the 5 case-control studies showed no significant
association between apical periodontitis and cardiovascular disease (OR = 1.24;
95% CI: 0.67–2.29, p = 0.494); these studies showed significant
heterogeneity (I
Random-effects meta-regression models indicated that age and percentage of men did not influence the association of apical periodontitis with cardiovascular disease in both cross-sectional (Supplementary Fig. 1) and case-control studies (Supplementary Fig. 2).
Overall, the studies presented a low risk of bias, showing moderate to good internal validity; most studies failed to provide a sample size justification or power description (criteria 5); furthermore, as most of the studies were cross-sectional there is no timeline to observe an effect (criteria 7), since the exposures and outcomes are assessed simultaneously (Supplementary Table 2).
Evidence of publication bias was established by funnel plot asymmetry and the
Egger test in cross-sectional (p = 0.001, Supplementary Fig.
3), but not in case-control studies (p = 0.147, Supplementary
Fig. 3). Regarding the impact of including/excluding each study in our findings,
the sensitivity analysis showed a decrease in the pooled OR from the
cross-sectional studies when removing one at a time from the analysis, the
studies with an OR
This study proposed to estimate whether apical periodontitis is associated with cardiovascular disease. Overall, the results of the eight cross-sectional studies included in the meta-analysis show that apical periodontitis is weakly associated with cardiovascular disease. Notwithstanding, when the meta-analysis focused only on the cohort and case-control studies included in the present review, the odds/risk ratio decreased and the association between apical periodontitis and cardiovascular disease lost statistical significance. The existence of publication bias, the considerable heterogeneity, and the contrasting results observed in studies with different design suggest caution when interpreting our results.
Previous systematic [18] and umbrella reviews [21] suggested a weak association
of apical periodontitis with cardiovascular disease highlighting the moderate-low
quality of the existing evidence. Our results also seem to suggest an association
of apical periodontitis with cardiovascular disease. Overall, our pooled odds
ratio estimate from cross-sectional studies shows an association between apical
periodontitis and cardiovascular disease (OR = 1.53) among adults. Yet, several
cross-sectional studies integrated in this meta-analysis showed an OR of less
than 1 (Fig. 2), suggesting that the presence of apical periodontitis was
associated with a reduction of the risk of cardiovascular disease. On the other
hand, there are studies showing a very high increase in risk; for instance, An
et al. [12] showed that adults with apical periodontitis were 5.3 times
more likely to have cardiovascular disease than adults without apical
periodontitis. Additionally, based on a limited number of cohort studies (n = 2)
and case-control studies (n = 5), our meta-analysis shows that apical
periodontitis did not significantly increase the risk or odds of cardiovascular
disease. There is a clear need for cohort studies with larger samples sizes in
which the population at baseline are free of cardiovascular disease. Only two
cohort studies, with a mean follow-up time
Several elements might also contributed to the substantial heterogeneity observed in the present meta-analysis, for example the lack of control for well-known cardiovascular disease risk factors (e.g., smoking, family history of cardiovascular disease, physical inactivity) in several studies, and the clinical heterogeneity among studies regarding the cardiovascular disease outcome. The small number of studies made it impossible to determine a pooled risk estimate by cardiovascular disease (e.g., coronary artery disease, heart failure).
It is important to mention that our results suggest an association, they do not support a causal relationship amongst apical periodontitis and cardiovascular disease. Yet, a link between oral diseases promoting systemic inflammation and endothelial dysfunction and cardiovascular disease, namely atherosclerotic-related diseases, has been proposed [4]. Chronic apical periodontitis, which is regularly related to poor endodontic treatment quality, is a consequence to endodontic infection initiated by bacterial infection of the root canal system [37]. The host response to microbial infection that emerges from the root canal system of the affected tooth may trigger systemic inflammation and endothelial dysfunction, hence promoting atherogenesis, as well as destabilizing pre-existing atherosclerotic plaques, therefore, inciting acute cerebro-cardiovascular events [4]. Despite this proposed link between oral and cardiovascular disease, whether the treatment of apical periodontitis reduces the risk of cardiovascular disease remains to be investigated.
Limitations. Despite including only studies diagnosing apical periodontitis using imaging techniques—to increase the consistency of the methodology—the meta-analysis presents high heterogeneity. Furthermore, the methodological quality of the studies was evaluated applying a recognized quality assessment tool (NIH tool for observational studies). We acknowledged that longitudinal cohort studies are preferable to cross-sectional studies or case-control studies, still, we included cross-sectional and case-control studies besides cohort studies in an attempt to increase the number of potential studies to be integrated in this systematic review. Some publication bias should not be neglected as only studies published in English were included. Additionally, the outcome (Outcomes: cardiovascular disease) was not consistent across studies. Cardiovascular disease was expressed as coronary heart/artery disease, angina pectoris and/or myocardial infarction, or a large spectrum of cardiovascular disease-related systemic diseases in accordance with the International Classification of Diseases. The heterogeneity in the outcome of interest may also limit its association with apical periodontitis. Finally, cardiovascular disease is associated with numerous risk factors, including lifestyle habits for example daily physical activity, smoking habits, and diet; although some studies adjusted for some risk factors for cardiovascular disease, it would have been interesting to examine their influence on the association between apical periodontitis and cardiovascular disease.
The results of the meta-analysis do not provide the necessary evidence to establish a strong association between apical periodontitis and cardiovascular disease. Based on cross-sectional studies, our meta-analysis suggests an association of apical periodontitis with cardiovascular disease; nevertheless, when the analysis was restricted to cohort and case-control studies the correlation became non-significant. Our results should be interpreted with caution, warranting additional longitudinal studies with long-term follow-up, with a priori sample size calculation, and exposure assessment the before the outcome.
RN, MT and FR have contributed to the development of the research question and study design. RN and MT developed the literature search. RN and MT performed the study selection. IC-R and CA-B analysed the data. RN, MT and FR interpret the results and wrote the manuscript. All authors reviewed and approved the manuscript.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
