Academic Editor: Alpo Vuorio
Background: Coronavirus disease 2019 (COVID-19) has significantly the
delivery of healthcare all around the world. In part, an abnormal and unexplained
high non-COVID-related cardiovascular mortality rate was reported during the
outbreak. We assess the correlation between anxiety level and decision to seek
medical care (DSMC) during the COVID-19 pandemic. Materials and methods:
We recruited patients with cardiovascular complaints admitted to the emergency
department in a single institute in Israel between February and September 2020.
Anxiety level was measured using available questionnaires. DSMC was assessed with
a newly designed questionnaire (DM-19). Results: Two-hundreds seventy
patients were included in the study. The mean age was 52.6
The unpredictable nature of the 2019–2020 Coronavirus pandemic has been shown to substantially increase the reported mental health disorders [1, 2, 3, 4, 5, 6, 7].
The social distancing, isolation, lack of familial support, inactivity, temporary or indefinite employment termination, loss of income, and personal autonomy have led to detrimental effects on both physical and mental status in both previously healthy people and those with preexisting conditions [8, 9].
Anxiety and depression were the most prevalent psychological disorders reported during the COVID-19 outbreak [10]. Anxiety is an emotional state characterized by feelings of tension, anxious thought, and apprehension [11]. High anxiety level (HAL) has been shown to affect behavior by avoiding coping, social strategy, and situation [12, 13, 14].
Decision-making is a cognitive behavior of selecting a course of action among various possible alternatives. It is commonly influenced by values, preferences, beliefs, knowledge, and situations and could be rational or irrational [15, 16, 17, 18]. Therefore, the decision to seek medical care can be particularly complex given the inherent nature of preserving one’s health and welfare. Previous studies demonstrate how variability in the population can affect decisions to seek medical care. Commonly cited factors include provider proximity, socioeconomic status, health insurance, and preexisting illness knowledge. Specifically, individuals who have dealt with an illness in the past and been informed by an educated provider are more knowledgeable, sensitized, and fearful of possible signs of relapse or worsening of their conditions [19, 20, 21, 22, 23].
Moreover, individuals living with a partner were more likely to seek health care than singles. One explanation for this is that discussing symptoms or concerns may prompt one’s partner to seek health care. Demographics also play a major role where women and elderly individuals, albeit without disabilities, are more likely to seek care. Nevertheless, the correlation between anxiety level and the decision to seek medical care during the outbreak is lacking [24, 25, 26].
The impact of COVID-19 on mental health disorders has been demonstrated in large and worldwide cohort studies. The initial reports of the outbreak in the news and the social media platforms lead to a disturbing increase in anxiety due to psychological and physical stressors, fear of contracting the disease, concerns for financial consequences, life routine disruption, and more [1, 2, 3, 4, 5, 6, 7, 8].
The outbreak has created an enormous global challenge for all health maintenance organizations (HMOs). Hospitals, intensive care units, and internal wards were converted into treating mainly COVID patients. The general lockdown, HMO reorganization, and the tremendous restrictions on the general population, medical care providers, and the general population’s mental state had a substantial and direct influence on the medical admission rate [27, 28, 29, 30, 31].
The study’s goal was to examine whether the COVID-19 outbreak affected the level of stress and anxiety among patients who sought medical care due to cardiovascular-related complaints and whether it impacted their decision to do so.
Our single-center study explores the prevalence and impact of anxiety among cardiac patients arriving to the emergency department in the initial COVID-19 outbreak. We demonstrate how high anxiety levels substantially impact patients’ decisions to seek medical care. Our results may explain cardiovascular mortality trends during the outbreak and should be considered in health crisis management.
We designed a cross-sectional survey-based prospective cohort study conducted in the Cardiology Department at Emek Medical Center in Israel in collaboration with the Med-Psych service and the Emergency Department. Patient recruitment began in February 2020 and lasted until September 2020. The study population included patients admitted to the Emergency Department with a cardiovascular complaint. Patients were excluded from the study if they were younger than 18, mentally disabled, pregnant, or tested positive for COVID-19 infection. Patients were recruited only after complete triage screening and preliminary medical examination to exclude urgent scenarios. Supplemental data on demographics, clinical data, and medical history were obtained using computerized medical records (“Orion”, “Ofek”, and “Chameleon”).
Patients were instructed to independently complete four questionnaires written in Israel’s four most used languages (Hebrew, Arabic, Russian, and English): The Beck Anxiety Inventory, the Cardiac Anxiety Questionnaire, and the General Anxiety Questionnaire.
The Generalized Anxiety Disorder Assessment (GAD-7) is a seven-item self-assessment questionnaire used to assess the severity of generalized anxiety disorder (GAD). The GAD-7 score is calculated by assigning 0–3 for each of the seven questions and obtaining a sum score between 0 to 21. Scores of 5, 10, and 15 are taken as the cutoff points for mild, moderate, and severe anxiety, respectively. Using a threshold score of 10, the GAD-7 has a sensitivity of 89% and a specificity of 82% for detecting high anxiety levels requiring further workup. The Beck Anxiety Inventory (BAI) is a 21 self-assessment multiple-choice question used to measure the severity of anxiety among adults. The standardized cutoffs are 0–7, 8–15, 16–25, and 26–63 for minimal, mild, moderate, and severe anxiety, respectively [24, 25, 26].
We designed a fourth self-assessment questionnaire (DM-19 questionnaire, Supplementary Table 1) to assess whether the patient considered COVID-19 before seeking medical treatment.
The DM-19 questionnaire contains two parts: the first is a nine-item multiple-choice survey designed to assess the importance of COVID-19 in patients’ daily decisions and assess decision-making concerns before seeking medical care. It contains five ‘Yes’, ‘No’ and ‘Do not know’ answers and four common escalating scale questions (i.e., extremely worried, worried, and do not worry). In the second part, the patients were instructed to choose three out of 12 sentences best describing their concerns before seeking medical care to assess the importance of concerns. For analysis purposes, we clustered these sentences into four clusters: regulations-related, illness-driven, non-illness-related, and financial-driven concern (Supplementary Table 2). Patients who did not fulfill at least 30% of the questionnaire were excluded from the analysis.
Patients’ medical information regarding essential characteristics and occupational and marital status were collected from the Clalit health data system (Orion, Ofek, and Chameleon software; Tel Aviv, Israel).
The Ethics Committee approved the study of the hospital following the Helsinki Convention (Approval No. EMC-20-0057). All subjects gave their informed consent for inclusion before they participated in the study. Recruitment was performed within 24–48 hours of hospital arrival after obtaining informed consent. Eligible patients underwent a personal interview during which they were asked to answer a structured self-assessment questionnaire written in their native language.
Calculation of the sample size was based on three main criteria: the population size—the total number of patients who were admitted to the emergency department during the study period due to chest pain (estimated as 840 patients), an estimated recruitment rate of about 0.3 and a response distribution of 50%. To achieve a margin of error of 5% and a 95% confidence level, we needed to recruit at least 264 patients.
A chi-square test was performed to analyze the association between the questionnaires and categorical variables. For continuous variables, we used the t-test (alternatively, the Wilcoxon two-sample test). Categorical variables were presented using frequencies and percentages. Means and standard deviations were calculated for continuous data, while frequencies and percentages were used for categorical data. 95% confidence intervals were calculated for key admission characteristics. Pearson correlation test was performed to test the association and the correlation between BAI and GAD-7 and the DM-19 to the rest of the questionnaires. Differences considered statistically significant were at the 2-sided p-value of 0.05. Statistical analysis was performed using SPSS version 24 (IBM, Chicago, IL, USA).
During the study period, 810 patients were admitted to the Emergency Department
with cardiovascular complaints. Thirty-six patients did not meet the inclusion
criteria (Age
 Fig. 1.
Fig. 1.Criteria determining eligibility. Patients admitted to Emek medical center with cardiovascular complaints were assessed for inclusion criteria and subsequently recruited to this study.
Two hundred eighty-seven patients participated in the study. The total
participants’ mean age was 52.6
The mean anxiety level was 10.3
Age was found to be a strong independent factor (
| Patient’s characteristics | GAD-7 | p-value | BAI | p-value | |||
| Low score |
High score |
Low score |
High score | ||||
| N = 123 | N = 164 | N = 144 | N = 143 | ||||
| Age Mean |
39.9 |
62.28 |
45.4 |
59.9 |
|||
| Gender (Male) | 79 (64.2%) | 104 (63.4%) | 0.88 | 95 (66.0%) | 88 (61.5%) | 0.43 | |
| Marital status | 0.01 | 0.04 | |||||
| Married | 103 (83.7%) | 153 (93.3%) | 118 (81.9%) | 138 (96.5%) | |||
| Single | 19 (15.4%) | 6 (3.7%) | 16 (11.1%) | 9 (6.3%) | |||
| Divorce | 1 (0.8%) | 5 (3.0%) | 3 (2.1%) | 3 (2.1%) | |||
| Employed | 79 (64.2%) | 104 (63.4%) | 0.88 | 95 (66.0%) | 88 (61.5%) | 0.43 | |
| Ethnic group | 0.29 | 0.49 | |||||
| Arabs | 53 (43.1%) | 75 (45.7%) | 68 (47.2%) | 60 (42.0%) | |||
| Jews (Israeli Born) | 35 (28.5%) | 50 (30.5%) | 38 (26.4%) | 47 (32.9%) | |||
| Jews (Former USSR) | 30 (24.4%) | 27 (16.5%) | 31 (21.5%) | 26 (18.2%) | |||
| Jews (African Born) | 5 (4.1%) | 12 (7.3%) | 7 (4.9%) | 10 (7.0%) | |||
| Smoker | 52 (42.3%) | 80 (48.8%) | 0.27 | 65 (45.1%) | 67 (46.9%) | 0.77 | |
| Obesity | 42 (34.1%) | 75 (45.7%) | 0.04 | 56 (38.9%) | 61 (42.7%) | 0.51 | |
| Family history of IHD | 37 (30.1%) | 56 (34.1%) | 0.46 | 49 (34.0%) | 44 (30.8%) | 0.55 | |
| Hypertension | 33 (26.8%) | 115 (70.1%) | 53 (36.8%) | 95 (66.4%) | |||
| Hyperlipidemia | 40 (32.5%) | 116(70.7%) | 64 (44.4%) | 92 (64.3%) | 0.001 | ||
| Diabetes mellitus | 15 (12.2%) | 76 (46.3%) | 29 (20.1%) | 62 (43.4%) | |||
| CABG | 3 (2.4%) | 11 (6.7%) | 0.09 | 6 (4.2%) | 8 (5.6%) | 0.57 | |
| Atrial fibrillation | 3 (2.4%) | 22 (13.4%) | 0.001 | 8 (5.6%) | 17 (11.9%) | 0.04 | |
| IHD | 12 (9.8%) | 70 (42.7%) | 27 (18.8%) | 55 (38.5%) | |||
| Heart failure | 5 (4.1%) | 22 (13.4%) | 0.007 | 12 (8.3%) | 15 (10.5%) | 0.52 | |
| CVA/TIA | 8 (6.5%) | 24 (14.6%) | 0.03 | 15 (10.4%) | 17 (11.9%) | 0.69 | |
| Anxiety | 21 (17.1%) | 63 (38.4%) | 26 (18.1%) | 58 (40.6%) | |||
| Depression | 9 (7.3%) | 36 (22%) | 0.001 | 10 (6.9%) | 35 (24.5%) | ||
| Psychiatric disease | 11 (8.9%) | 52 (31.7%) | 18 (12.5%) | 45 (31.5%) | |||
| CABG, Coronary artery bypass graft surgery; IHD, Ischemic heart disease; USSR, Union of Soviet Socialist Republics; CVA, Cerebrovascular accident; TIA, Transient ischemic attack. | |||||||
 Fig. 2.
Fig. 2.Correlation between age and anxiety level. (A) Anxiety assessed byGAD-7 questionnaire; (B) anxiety assessed by the BAI (B) questionnaire.
The most common initial presentation was chest pain seen in more than eighty
percent of patients regardless of anxiety level. HAL patients were diagnosed more
commonly with unstable angina and Non-ST elevation myocardial infarction and had
a higher rate of coronary catheterization (significant p-value for all).
Nevertheless, the diagnosis of coronary artery disease (defined as
| Patient characteristics | GAD-7 | BAI | |||||
| Low score |
High score |
p-value | Low score |
High score |
p-value | ||
| N = 123 | N = 164 | N = 144 | N = 143 | ||||
| Primary complains | |||||||
| Chest pain | 106 (86.2%) | 141 (86.0%) | 0.61 | 124 (86.1%) | 123 (86.0%) | 0.63 | |
| Dyspnea | 6 (4.9%) | 11 (6.7%) | 7 (4.9%) | 10 (7.0%) | |||
| Palpitation | 10 (8.1%) | 12 (7.3%) | 12 (8.3%) | 10 (7.0%) | |||
| Other | 1 (0.8%) | 0 (0.0) | 1 (0.7%) | 0 (0.0) | |||
| ECG changes on admission | 8 (6.5%) | 29 (17.7%) | 0.005 | 11 (7.6%) | 26 (18.2%) | 0.008 | |
| High serum troponin I | 8 (6.5%) | 24 (14.6%) | 0.03 | 11 (7.6%) | 21 (14.7%) | 0.04 | |
| High serum CPK level | 8 (6.5%) | 23 (14.0%) | 0.04 | 11 (7.6%) | 20 (14.0%) | 0.05 | |
| Preliminary diagnosis | |||||||
| Stable angina | 6 (4.9%) | 29 (17.7%) | 0.002 | 8 (5.6%) | 33 (23.1%) | ||
| Unstable angina/NSTEMI | 9 (7.3%) | 24 (14.6%) | 11 (7.6%) | 24 (16.8%) | |||
| Myocarditis | 3 (2.4%) | 2 (1.2%) | 4 (2.8%) | 1 (0.7%) | |||
| Coronary catheterization | 14 (11.4%) | 67 (40.9%) | 22 (15.3%) | 59 (41.3%) | |||
| Significant lesion (per CAQ group/per coronary catheterization) | 11 (8.9/78.6) | 38 (23.2/58.5) | 0.002/ |
18 (12.5/72.0) | 31 (21.6/52.5) | 0.03/ | |
| ECG, electrocardiogram; CPK, creatine phosphokinase; NSTEMI, non-ST elevation myocardial infarction. | |||||||
Two hundred eighty-seven patients completed the DM-19 questionnaire. We weighted the answers of the DM-19 based on its impact on the decision to seek medical care. Answers were weighted +1 or +2 if the pandemic significantly impacted the decision before seeking medical care; ‘0’ if the pandemic had some level of concern but did not alter the normal medical decision to seek care as before the outbreak, and ‘–1’ if the pandemic was not a concern when seeking medical care. Three questions weighted ‘2’ points due to the answers’ direct nature and their impact on decision-making (Supplementary Table 1). The scores ranged from –8 to 12. Analyzing all possibilities yield the following results: scores between –8 and 5 suggest the outbreak did not influence the decision to seek medical care, scores between 5 and 7 indicate the outbreak had been part of the patient’s concerns before seeking medical care, and a score of 8 or higher imply that the decision to seek medical care was significantly affected by the outbreak.
Based on score interpretation of the DM-19, fifty-five (19.2%) patients had a
score of less than 5, and 232 (80.8%) patients had a score of five or greater.
The mean score of the total study population was 6.4
The total score on the DM questionnaire showed a positive correlation with the
categorized anxiety level of GAD-7 and the BAI questionnaires (R
 Fig. 3.
Fig. 3.Correlation between time to seek medical care and anxiety. (A) Anxiety assessed by GAD-7 questionnaire; (B) anxiety assessed by the BAI (B) questionnaire.
Moreover, question analysis of the DM-19 reveals a connection between anxiety and the time to seek medical care. Most HAL patients sought medical care more than two days from symptoms onset, whereas most LAL patients sought medical care on the same day of symptoms onset (Fig. 3).
Analyzing the patient’s concern of coming to the hospital regarding anxiety level showed different distribution graphs. Non-illness-driven concern was the most prominent among HAL patients in both questionnaires. Illness-related concerns and losing financial support were the most prominent among LAL patients in both questionnaires (Fig. 4).
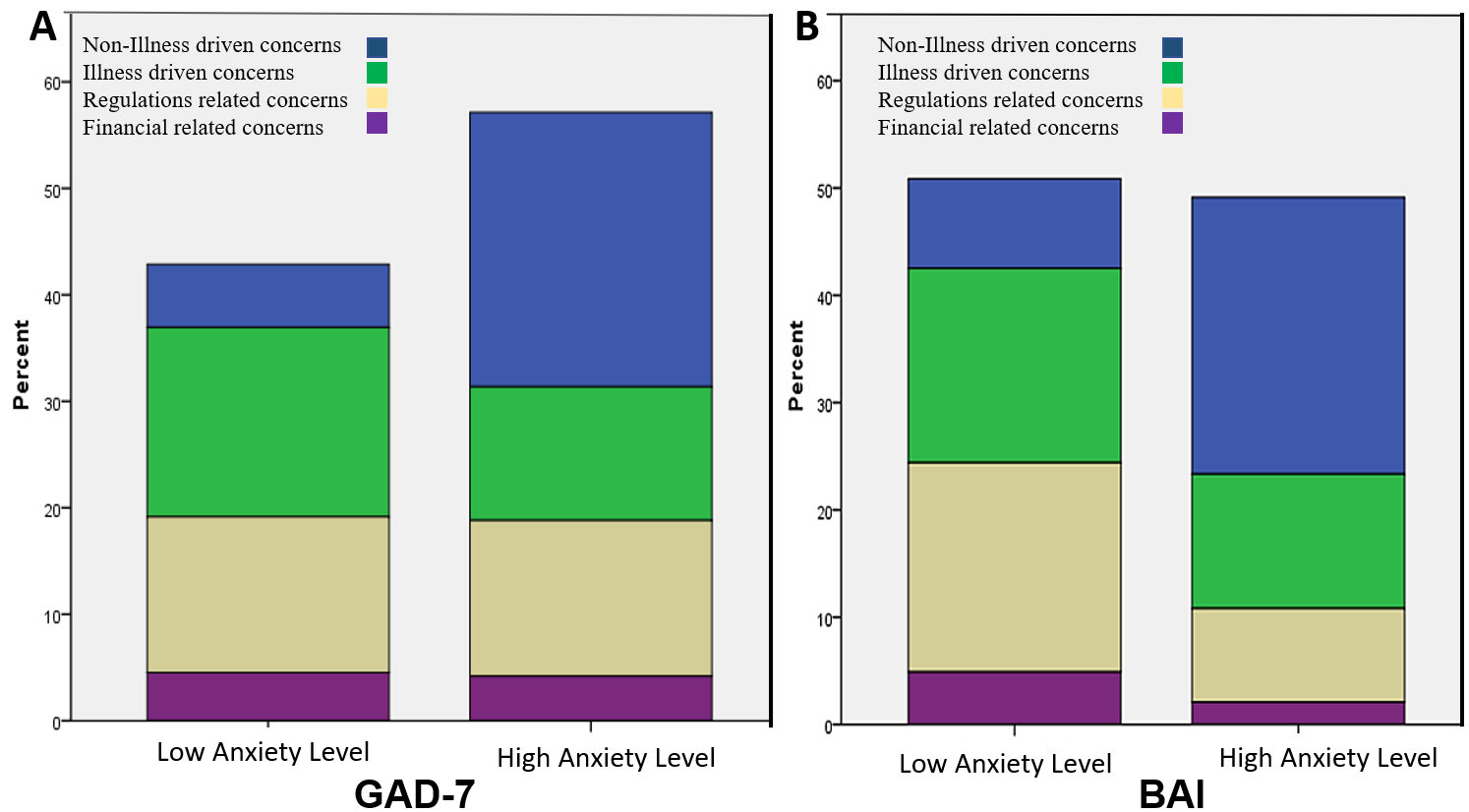 Fig. 4.
Fig. 4.Decision-driven concerns based on the DM-19 questionnaire: restriction-related concerns (blue), illness driven (green), financial-driven (grey), and anxiety-driven (purple) concerns. (A) Anxiety level according to GAD-7. questionnaire; (B) anxiety level according to BAI questionnaire.
Our study demonstrated a disturbingly high level of anxiety among non-COVID patients who sought medical care during the outbreak in Israel and was more pronounced in the elderly population. The normal fear of cardiovascular disease could explain the strong and positive correlation of age with high anxiety levels, yet we believe that the high mortality rate reported from the COVID infection in the elderly population had a major impact.
The high prevalence of myocardial injury in HAL patients strengthens the widely known notion that anxiety levels usually accommodate a real physical condition. Moreover, we could see that more coronary catheterization was performed on HAL patients than LAL patients. These procedural rates are consistent with the more impressive risk factors and clinical presentation of HAL compared to LAL patients as demonstrated in Tables 1,2. Nevertheless, the absence of anxiety does not directly correlate with the prevalence of coronary artery disease, nor its severity, as seen in the high rate of coronary artery disease among LAL patients.
Our study shows a positive correlation between anxiety level and the decision to seek medical care of non-COVID patients, which eventually results in deferring serious medical care. This observation could provide an additional explanation for the higher incidence of out-of-hospital cardiac arrest and higher mortality rate reported during the outbreak [32, 33, 34, 35, 36, 37, 38]. Our data is consistent with retrospective observational studies conducted outside of Israel [39, 40]. In March of 2020 in Austria and Italy, investigators demonstrated a dramatic decline in the admission and treatment rates across all subtypes of acute coronary syndromes. Meanwhile, deaths related to acute coronary syndromes tripled. Similarly, in the US, the rate of STEMI-related catherization lab activations declined precipitously.
We believe that Health organizations services should be aware of the high level of anxiety of non-COVID patients and its impact on seeking medical care. In doing so, the healthcare field can adapt the necessary provisions to inform medical care during a global pandemic. One important factor is the education of policymakers, legislative parties, and media outlets. These groups play a large role in modern-day public perception, particularly with the ongoing pandemic’s social, health, and economic uncertainty [41]. Using these influencing bodies, public campaigns can help encourage people to promptly seek health care upon noticing signs or symptoms unrelated to COVID-19 infection [42, 43, 44, 45, 46].
Additionally, recommendations to current health policy guidelines may also influence the population in seeking medical care. One solution is instituting more frequent virtual primary consultations. Gaining increasing popularity in the last decade, virtual visits help avoid physical proximity to providers and other patients, thereby reducing the risk of contracting COVID-19 [47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59]. Moreover, providers can use the virtual platform to maintain care for their patients, namely vulnerable individuals more likely to defer care during the pandemic. This includes those with a severe, known disease requiring close monitoring, the elderly, and psychiatric patients. Virtual visits can also be a means to distribute short questionnaires to address lingering health concerns, assess anxiety levels, and help determine appropriate timing for an in-person or additional virtual consultation. Lastly, healthcare providers can be educated, encouraged, and incentivized to offer more comprehensive and strong emotional support to non-infected patients.
With regards to limitations, the study lacks a strict causal design, making some of the inferences and analyses difficult to interpret. Specifically, we did not have data to demonstrate our patient population’s healthcare-seeking behavior before the pandemic. In large part, this was due to the abrupt onset of the pandemic and its ongoing status. Therefore, it would be insightful to assess further changes in anxiety level and healthcare-seeking behavior in light of updated news and regulations. Additionally, a comparator group of patients who did not enter the emergency department with health problems was not available, further limiting this analysis’s findings and causal nature.
Decision-making is a complicated field in psychology with limited assessment tools. The rapid nature of the pandemic requires us to design a new, concise (as the clinical scenario indicated) and multilingual survey to reflect the aim of the study best. Therefore, the DM-19 questionnaire could not be validated before the study. Moreover, we focused on the main observations and showed the raw data from the surveys instead of implying multiple analytic methods. Finally, self-assessment questionnaires are inherently subjective and do not account for variability in patient responses. This is particularly relevant in the context of our study where we asked patients to quantify their anxiety. For instance, it is possible that the highly anxious patients are more likely to report a falsely higher score on the DM-19 questionnaire compared to those with lesser levels of anxiety [60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72].
Our study represents a single center’s experience in the northeast of the country and therefore does not truly represent the entire population. However, the pandemic did not have geographical diversity, and the national regulations applied to the entire population. Therefore, we believe that geographical variation did not play a major role in decision-making during that period. Nonetheless, it is imperative to determine whether our findings are pertinent across different regions in the world. Differences in government response, containment, and politicization of the pandemic likely affect patient perception of the pandemic and therefore their routine behavior including decisions to seek medical care [73, 74, 75, 76, 77, 78, 79, 80]. Additionally, our study was conducted prior to the distribution of the coronavirus vaccine. Future studies may demonstrate a shift in patient perception and anxiety given increased vaccine’s protective effects [81, 82, 83, 84].
Nearly half of patients admitted to the emergency department during the COVID-19 outbreak display high anxiety level. Old, married, and unemployed patients with multiple cardiovascular comorbidities and a history of anxiety, depression, or psychiatric disorder demonstrated significant HAL.
While patients with HAL presented with more objective evidence of myocardial injury, they were less frequently diagnosed with coronary artery disease via coronary catheterization.
The decision to seek medical care has a positive and significant correlation with anxiety levels. HAL patients reported seeking medical care 2–4 days from symptom onset, which was significantly higher than LAL patients. HAL patients were also more concerned about non-illness-derived anxiety than LAL patients, while the latter was more concerned about an illness-derived concern and losing financial support.
A future study involving patients in different geographic regions across different pandemic peaks at various vaccination stages may give us more information on human behaviors in seeking medical care during the pandemic.
OK, SAR, ER, YT, KZ, WS, DI and EM designed the research study. SAR, MB, MS, AS, KZ, WS, DI and EM performed the research. OK, MB, MS, AS, and EM analyzed the data. OK, RN, VP, EN, YT, ER analyzed the data. OK, RN, EN, VP assist in revision the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
The Ethics Committee approved the study of the hospital following the Helsinki Convention (Approval No. EMC-20-0057). All subjects gave their informed consent for inclusion before they participated in the study.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
