Academic Editor: Peter A. McCullough
The coronavirus disease-19 (COVID-19) pandemic has forced hospitals to prioritize COVID-19 patients, restrict resources, and cancel all non-urgent elective cardiac procedures. Clinical visits have only been facilitated for emergency purposes. Fewer patients have been admitted to the hospital for both ST-segment elevation myocardial infarctions (STEMI) and non-ST segment elevation myocardial infarctions (NSTEMI) and a profound decrease in heart failure services has been reported. A similar reduction in the patient presentation is seen for ischemic heart disease, decompensated heart failure, and endocarditis. Cardiovascular services, including catheterization, primary percutaneous coronary intervention (PPCI), cardiac investigations such as electrocardiograms (ECGs), exercise tolerance test (ETT), dobutamine stress test, computed tomography (CT) angiography, transesophageal echocardiography (TOE) have been reported to have declined and performed on a priority basis. The long-term implications of this decline have been discussed with major concerns of severe cardiac complications and vulnerabilities in cardiac patients. The pandemic has also had psychological impacts on patients causing them to avoid seeking medical help. This review discusses the effects of the COVID-19 pandemic on the provision of various cardiology services and aims to provide strategies to restore cardiovascular services including structural changes in the hospital to make up for the reduced staff personnel, the use of personal protective equipment in healthcare workers, and provides alternatives for high-risk cardiac imaging, cardiac interventions, and procedures. Implementation of the triage system, risk assessment scores, and telemedicine services in patients and their adaptation to the cardiovascular department have been discussed.
The coronavirus disease-19 (COVID-19) outbreak caused by the severe acute
respiratory syndrome coronavirus-2 (SARS-CoV-2) initially originated in the city
of Wuhan, China in December 2019. Owning to the rapid transmissibility rate of
the virus, the outbreak spread across international borders affecting nearly 218
countries and territories worldwide. It was soon declared as a pandemic by the
World Health Organization (WHO) on 11
There have been suggestions to prioritize and triage cardiac patients which would potentially reduce the patient load and the risk of exposure to healthcare workers. This can be possible through the use of telemedicine, which also enables specialists to timely evaluate patients [4]. Prioritization of patients can be standardized and objectively carried out through scoring systems, adjusted according to the need versus the risk of performing cardiovascular procedures in patients during an ongoing pandemic. One study proposed a medically necessary, time-sensitive (MeNTS) procedure scoring system that enabled quantification of certain procedure factors, patient factors, and disease factors that reflected the number of resources to be utilized by patients. A higher score reflected higher resource consumption [5]. In this review, we have discussed the massive impact of the pandemic on various cardiology services and proposed solutions to minimize the disruptions in the services.
An extensive literature review was conducted using PubMed/MEDLINE and Google Scholar databases from their inception until December, 2020 for this review. The following search string was employed: (“COVID” OR “SARS-CoV-2”) AND (“cardiovascular services” OR “cardiac patients” OR “cardiac consultations” OR “cardiac interventional procedures”). No time or language restrictions were set. All articles retrieved from the initial search were transferred to Endnote Reference Library (Version X9; Clarivate Analytics, Philadelphia, Pennsylvania) where duplicates were identified and removed. Initially, the search included 3736 articles, 1033 duplicates were identified between Google Scholar, and PubMed were excluded. A total of 2703 titles and abstracts were scanned, of which 152 studies were found relevant. A further 22 exclusions were made as the full text was not available for these studies. Another six studies were excluded as they were not available in English. Total of 124 full texts were then retrieved, and a further 33 exclusions were made as these studies were beyond the scope of this review. The exclusions were made on the basis of studies not being relevant to effects of COVID-19 on cardiology department, staff, procedures, surgeries and services. Finally, 91 studies were included in this scoping review.
Due to the high risk of SARS-CoV-2 infection, many patients opted to stay at home and approach for medical help via telehealth rather than an in-person visit to the hospital for consultation. This led to a worldwide decrease in the cardiac patient’s inflow. Hospitals reserved their finite healthcare resources for COVID-19 by decreasing cardiac catheterization laboratory (CCL) procedures [6]. Reservation of hospital beds was considered as a suitable option to facilitate COVID-19 positive patients. This led to a reduction in patients being admitted to hospital which was not in the best interest of patients with comorbidities such as diabetes mellitus, hypertension, or severe cardiac conditions like valvular heart diseases, or heart failure [7]. Since resources were reserved for COVID-19 positive patients to tackle the massive inflow, the bed capacity of intensive care units (ICUs) had decreased. Cardiac surgeries require ICUs for monitoring patients and mechanical ventilation and reduced availability led to a regression in admissions [8, 9]. Italy reserved 64% of hospital beds and 88% of ICU beds for COVID-19 patients, canceling all non-urgent elective cardiac procedures [10]. Canada, along with Italy had taken the same precautionary measures so that COVID-19 patients were given utmost priority [11]. According to a study, there was a 53% drop in patients presenting with symptoms to the cardiac ward, and 40% fewer patients were diagnosed with myocardial infarctions [12].
Similar studies have demonstrated a reduction in admission for acute myocardial infarctions (AMI) during the pandemic. A registry study mentioned a global decrease in MI admissions during lockdown [13]. Studies conducted in the US and France showed a decline in admissions of MI patients [14, 15, 16]. Patients referred to heart failure services were reported to decrease by 34% during the lockdown period [12]. A study based in Italy assessed one week in 2020 (during the pandemic) and compared it to 2019, stating a 48.4% reduction in AMI for both ST-segment elevation myocardial infarctions (STEMI) and non-ST segment elevation myocardial infarctions (NSTEMI) with a 52.1% decrease in North Italy and South Italy and 59.3% decrease in Central Italy. Weekly admissions for NSTEMI were seen to drop from 350 in 2019 to 122 in 2020, which is more than a 50% decline. Only 82 patients were admitted for heart failure in 2020, in contrast to 154 patients in 2019 [17].
It has already been established that close contact poses a high risk of contracting SARS-CoV-2 infection via transmission by aerosol droplets. Hence, aerosol-producing procedures such as intubations and positive pressure ventilation should be avoided, which can pose a threat to healthcare workers [18]. In addition, patients with suspected COVID-19 infection should not be intubated in the catheterization lab due to unavailability of proper ventilation for infection isolation [7]. Even if personal protective equipment is worn for intubations, one study found that unexposed skin and hair can still be contaminated [19]. Patients with COVID-19 or suspected COVID-19 requiring intubation should be intubated prior to arrival at the catheterization laboratory [7].
It is recommended to avoid elective procedures within the catheterization
laboratory on patients with significant comorbidities expecting to require
hospital stay
Furthermore, cardiac procedures on confirmed or suspected cases of COVID-19 must be performed in a dedicated COVID-19 catheterization laboratory [25]. Uninfected patients undergoing treatment for acute coronary syndrome should be discharged within 24 hours to reduce exposure. COVID-19 infected NSTEMI patients with high-risk features of myocardial infarction prompt a difficult decision to be made regarding the performance of an urgent PCI without waiting for the SARS-CoV-2 PCR test result [25]. This poses a threat of exposure to the staff. A retrospective multicenter study also found high rates of stent thrombosis in COVID-19 infected STEMI patients undergoing PCI, warranting strict monitoring of thrombotic events in such patients [26].
For the patient’s safety, early discharge is preferred right after the cardiac procedure to minimize the risk of COVID-19 transmission, given that hospitals are high-risk zones. Early discharge has reduced cardiology trainee exposure to patients and caused inadequate examinations being performed. This has affected their learning experience [7]. Minimizing staff members to prevent crowding in hospitals caused unemployment and fewer medical personnel available on duty [8]. Staff affected with COVID-19 quarantined themselves, leading to a shortage of hospital staff and reduced patient admission classified as non-urgent cases as demonstrated in Fig. 1 [8].
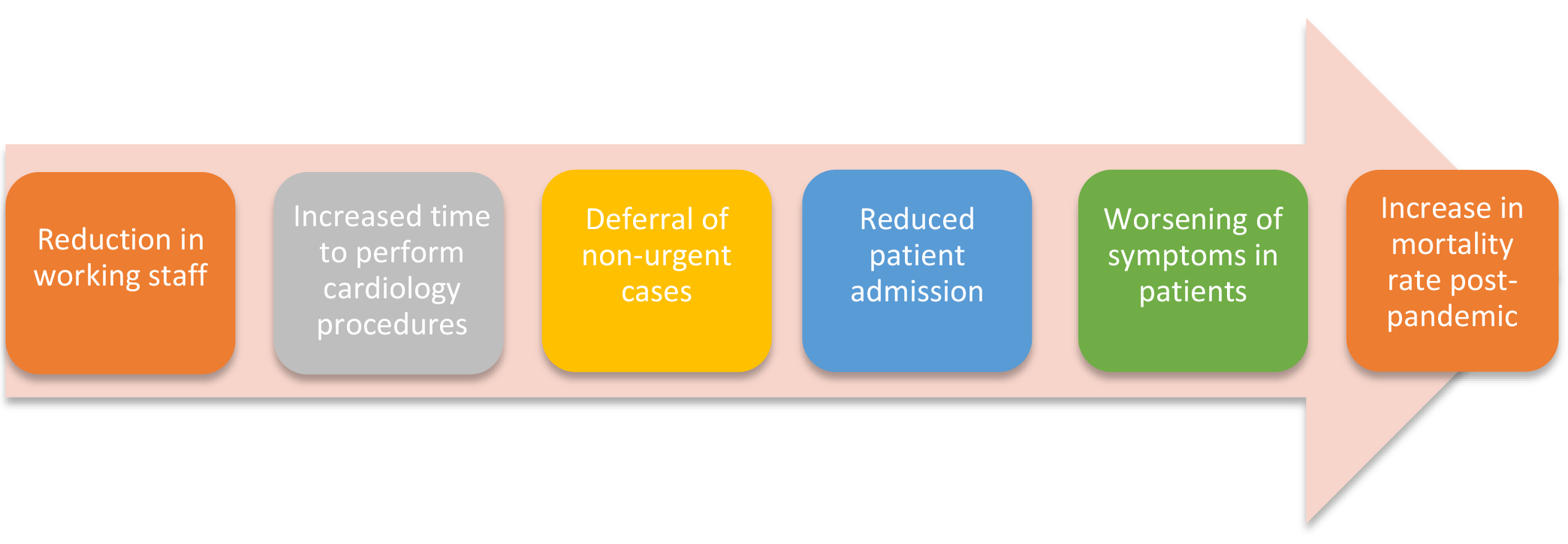 Fig. 1.
Fig. 1.Variation in hospital staff leading to increased cardiac mortality rates post-COVID-19. Reduction in working personnel due to quarantined staff members or minimization of staff to prevent overcrowding in the hospital results in increased time taken to perform cardiac procedures such as PCIs and echocardiography. This leads to deferral of patients classified as non-urgent cases that might increase mortality rates in cardiac patients following the COVID-19 pandemic. Abbreviations: COVID-19, coronavirus disease-19; PCIs, percutaneous coronary interventions.
Percutaneous coronary interventions (PCIs) have been widely used as the management of choice for STEMI patients [24, 27, 28]. According to statistics, PCI performed in Spain decreased by 40% from February to March 2020 during the COVID-19 pandemic [27]. In Austria, a 39.4% decline in PCI was noticed in acute coronary syndrome (ACS) patients [28]. In the US, there was a 38% reduction in PCIs being performed in STEMI patients [24]. Increased time taken for a PCI to be performed is a major contributing factor leading to fewer procedures being done. This may be attributed to the increased time taken to reach a definitive diagnosis of the primary cause to be STEMI or COVID-19. Moreover, some time is utilized in the catheterization lab due to wearing and disposing of personal protective equipment (PPE) for each procedure, contributing to longer intra-procedural time and fewer procedures being performed [29]. Due to the COVID-19 pandemic, PCI is no longer considered a first-line treatment among STEMI patients. This is to ensure the minimization of viral transmission especially due to the unavailability of negative pressure in catheterization labs [22]. The inability to use protective gear as part of the COVID-19 protocol, while using under-wires in PCIs also reduced the total number of PCIs being performed [22].
It is important to provide cardiac patients with timely care to minimize the adverse effects on cardiac tissues. A study from Hong Kong stated that before the pandemic, it took nearly 88 minutes for a patient to present to the hospital after the onset of symptoms. While during the pandemic, it was noticed to be four times the usual time i.e. 319 minutes [30]. The time spent to reach the catheterization lab and wire crossing increased by 11 minutes; 22 min before and 33 min after the pandemic [30]. Door-to-door device time was found to be increased by 30 min in a study with a median of 110 minutes in 2020, in contrast to 84.9 minutes a year before [30]. These statistics help conclude that the pandemic has caused delays in medical attention given to patients presenting with cardiac complaints due to the reduced in-hospital staff. A retrospective registry study carried out in 77 European high volume PCI centers across 18 countries concluded a 19% decrease in PCI procedures compared to 2019 [31]. A study comprising acute ischemic syndrome (AIS) patients with large artery occlusion highlighted an increase in hospital arrival to puncture time by 48.5 minutes and arrival to reperfusion time by 41 minutes [32]. This delay was due to the COVID-19 screening tests that are mandatory for all patients according to the protocol set by the National Health Commission (NHC) [32]. Further studies should be conducted to determine the reduction in PCI procedures on a global scale.
Clinical consultations have been decreased to maintain social distancing and to limit viral exposure to patients [6]. Only emergency cases are facilitated and brought to the hospital, abiding by the pandemic protocol. A study highlighted a 93% decrease in the outpatient presentation. This implies almost a complete absence of patients presenting to outpatient consultation [12]. Patients were advised not to visit the hospital for follow-ups and to avail telemedicine services where applicable [12]. Reducing physical contact meant cancelling all consultation appointments [28, 33]. A decline in patient presentation was noted for cardiac diseases comprising ischemic heart disease, decompensated heart failure, and endocarditis. However, delays should be avoided for these diseases since it can have a deleterious impact on patient’s health [27, 34, 35]. Reduced patient presentation implies decreased diagnosis of patients with cardiac problems as previously highlighted by the American College of Emergency Physicians, which predicted a smaller number of patients to be diagnosed with ACS due to all resources being allocated to COVID-19 patients [36]. As highlighted in another study, the ACS protocol has been delayed as hospitals continued to shift their attention towards the COVID-19 pandemic [37].
During the early phase of the pandemic, massive cancellations were noticed in hospital records. Using risk scoring assessments [21, 22] meant facilitating urgent cases that caused a greater than half reduction in investigations being performed, such as electrocardiograms (ECGs) and outpatient echocardiograms [12]. Other investigations such as the exercise tolerance test (ETT) and dobutamine stress test were also affected. Computed tomography (CT) angiography was observed to decrease by 63% with reductions also noticed in transesophageal echocardiography (TOE). Imaging for all non-emergency cases was cancelled until further notice to reallocate resources towards COVID-19 positive and emergency cardiac patients [38]. Delaying cardiac imaging can have devastating effects on patients, leading to worsening of cardiac symptoms and increased mortality due to delayed medical care. Similarly, a smaller number of elective angiograms were performed, giving priority to emergency cases presenting to the hospital [39]. A study comprising the pediatric age group following the COVID-19 protocol showed an increase in the time taken to perform echocardiography. The study mentioned that one of the causes was a reduction in staff to prevent transmission of the virus [21].
Considering that pandemic triage-based admissions were taking place, this led to the categorization of patients into priority groups according to the severity of the disease [22]. Pacemakers were only implanted in priority groups since all non-urgent cases were deferred, reducing the number of pacemaker implantations usually performed [12]. Cardiac surgeries have also been decreased according to the Centre for Medicare and Medicaid Services. In the US, cardiac surgeries have only been limited to extremely symptomatic patients [40]. A study compared data from last year’s hospital admissions and determined that in March 2020, only 57 patients were admitted to the hospital for severe emergent cardiac disease, while 117 patients were admitted last year [41]. The data shows an approximate 50% decline in patients’ admissions and fewer procedures being performed. This was further supported by another study which showed a 49% decrease in cardiac surgeries for March and April 2020 compared to the same two months in 2019 [42]. The study also mentioned a 9% decline in coronary artery bypass graft (CABG) procedure for two months in comparison to 2019 [43]. Major aortic surgeries were observed to decrease by 44% compared to last year [43]. Heart and lung transplantation and ventricular assist device implantation reported a 50% decrease since the COVID-19 pandemic [43]. To reduce the COVID-19 transmission, hospitals were divided into COVID-19 and non-COVID-19 health centers to facilitate all kinds of patients. Unfortunately, this could not be implemented well. For instance, the Friuli Venezia Giulia region, Italy has 3 hub hospitals where PCI and pacemaker implantations are performed but these 3 hospitals have been reserved for COVID-19 patients only [41]. Another study reported a 13.3% decrease in PCI for NSTEMI patients in a week in 2020, compared to 2019 [17].
Early diagnosis and detection of certain serious heart conditions are imperative
in forming a suitable and quick treatment plan to lower patient morbidity and
mortality. A decrease in diagnostic services could result in a remarkable
increase in the number of patients suffering from severe cardiac complications
further down the line [42]. A study suggests that cardiovascular procedures have
an urgency of 2 weeks [9]. Therefore, a significant lack of overall cardiac
services could culminate in serious short-term as well as long-term implications.
Delay in getting hospital care along with risk scoring methods [21, 22] has
deprived cardiac patients of timely medical attention. Hospital admission of only
severe cardiac conditions can cause the worsening of preexisting cardiac
diseases. According to many epidemiological studies, it has been concluded that
patients with preexisting cardiac disease and patients with atherosclerotic risk
factors are prone to develop ACS [44, 45, 46, 47]. Late presentation to the hospital can
lead to hospital cardiac arrests [39]. This prediction is supported by data from
France; an analysis pointed out an increase in 13% of hospital cardiac arrests
due to delayed medical help [48]. In most countries postponement of elective
cardiology procedures has caused an accumulation of cardiology cases [9]. Recent
statistics have shown that there has been a sharp decline in cardiac
hospitalizations across the UK [46] while another study from the European Society
of Cardiology reported the number of heart attack patients seeking urgent
hospital care to drop by
A marked decrease in the access to emergency departments (by 30% in Milan) and a decline of up to 50% in the incidence of NSTEMI cases have been reported [51]. This suggests that reduced access to cardiology services may lead to a continued and increased incidence of more severe cardiac problems [52]. Cancellation of outpatient elective services may have adverse consequences, such as an increased risk of sudden cardiac death (e.g. primary prevention defibrillators), hospitalization due to cardiac events, poorer outcomes due to postponement of intervention (e.g. aortic stenosis, atrial fibrillation ablation), receiving treatments associated with inferior outcomes (e.g. PCI in multi-vessel disease rather than CABG) [53]. Moreover, an analysis in the US shows an estimate of a 38% decrease in PCI for STEMI treatment [14]. This decrease in PCI may have harmful long-term effects on patient mortality and morbidity. A current study estimates that more than 50% of elective surgical cases could potentially cause significant harm or impairment in patients’ health if cancelled or delayed [35]. Therefore, these postponements or cancellations could lead to a prolonged low quality of life, along with exacerbating symptoms. They may even cause presentations of some atypical symptoms that patients may not be aware of and an increase in emergency hospital admissions [39]. The absence or delay of pertinent surgical care may result in the worsening of physiological conditions of vulnerable patients; the ensued deterioration in patients’ health could make them more susceptible to contracting COVID-19 [54].
A recent study conducted in the UK shows that the second interval of the pandemic presented with a gradual increase in patients referred to cardiology services and a rise in the investigation and diagnosis of myocardial infarctions compared to the first interval of the pandemic [3]. Hence, the cessation of cardiology services during the COVID-19 outbreak could result in a rebound influx of patients referred to cardiology services, which in turn could lead to a significantly increased workload on cardiology services post-pandemic, as estimated in the study conducted by Fersia et al. [3]. However, more studies are needed to further evaluate the long-term implications of the disruption in cardiology services due to limited data currently available.
Additionally, the COVID-19 pandemic has had several psychological consequences resulting in a broad range of mental health disorders primarily induced by fear, anxiety, and stigma [55]. A study comprising 1210 respondents across 194 cities in China reported 54% of respondents to rate the psychological impact of the COVID-19 outbreak as ‘moderate or severe’; 29% reported ‘moderate to severe anxiety’ symptoms, and 17% reported ‘moderate to severe depressive’ symptoms [56]. These psychological implications caused certain patients to be reluctant to seek immediate medical assistance, consequently putting their lives at a greater risk [42] as reflected by a study published in Mattioli, which enlisted ‘patients afraid of contracting COVID-19 when entering hospital’ as one of the contributing factors for reduction in STEMI presentation. Furthermore, a delay or cancellation in cardiology services could exaggerate these negative psychological impacts amongst patients and may have increased adverse effects on their mental health [57]. Concurrently, it is possible that these psychological implications combined may cause reservations and reluctance among patients to seek timely medical help even after the COVID-19 outbreak is resolved [58]. The impact of the COVID-19 pandemic on the psychological health of cardiac patients is presented in Fig. 2.
 Fig. 2.
Fig. 2.The impact of the COVID-19 pandemic on the psychological health of cardiac patients. The worsening of mental health among cardiac patients could be attributed to the reluctance to receive medical assistance during the pandemic in addition to the fear and anxiety due to delayed cardiology services being provided by hospitals. Both fear and reluctance stem from the general stigma associated with COVID-19 and the fear of contracting the virus, especially from the hospital. The figure highlights the interconnection between the associated factors.
Abbreviations: COVID-19, coronavirus disease-19.
Hence, it is more than probable that cessation and suspension of cardiology services may have several significant long-lasting implications on the physiological in addition to psychological wellbeing of affected individuals. From worsening underlying cardiac comorbidities to deteriorating psychological health, it is evident from the factors stated above that serious consequences due to these suspensions are inevitable.
Considering the impact that COVID-19 pandemic has posed on the provision of cardiology services, appropriate protocol and strategies need to be implemented to ensure the smooth running of an already overburdened healthcare system. We propose a few solutions for the cardiology department to counter the repercussions that this pandemic has had on its services. Some of the solutions have been summarized in Table 1.
| Impact of COVID-19 on cardiology services | Consequences for the hospital and patients | Potential strategies |
| Contamination of equipment and risk of COVID-19 transmission during imaging and interventional procedures | Decreased cardiac investigations and imaging procedures | |
| Reduced cardiac interventions | Adverse effects on patient morbidity and mortality | Prioritization of patients with worse risk stratification scores for interventional procedures |
| Increased time to reach the hospital and receive medical attention | Late presentation to the hospital can increase hospital cardiac arrests | Triage can also be utilized along with risk stratification scores to cater to critically ill patients |
| Aerosol generation during cardiopulmonary resuscitation and intubation | Risk of exposure to healthcare workers | |
| Early discharge of patients after cardiac procedures | Reduced cardiology trainee exposure to patients | |
| Quarantined staff members | Reduced working personnel | |
| Abbreviations: COVID-19, Coronavirus disease-19; INR, International normalized ratio; TEE, Transesophageal echocardiogram; CT, Computed tomography; FoCus, Focused cardiac ultrasonography; SPECT, Single photon emission computed tomography; WHO, World Health Organization; AI, Artificial intelligence; PPE, Personal protective equipment; ICUs, Intensive care units. | ||
According to the World Health Organization (WHO) guidelines, all healthcare workers are required to wear appropriate PPE in all procedures [72]. There has been a worldwide shortage of PPE available for healthcare personnel. Hospitals can ensure that they have adequate supplies by contacting local manufacturers and purchasing them in bulk as PPE is mandatory for all aerosol producing procedures including transesophageal echocardiography (TEE), cardiopulmonary resuscitation (CPR), intubation, extubation, ventricular tachycardia ablation, and echocardiography [53]. Healthcare setups need to ensure that their PPE equipment includes all the mentioned necessary components. Training of the catheter lab staff regarding the donning and doffing of PPE is very important to avoid wastage.
Cardiovascular disease usually presents at an advancing age and is more prevalent in patients with an impaired immune system and elevated levels of angiotensin-converting enzyme-2 (ACE-2) receptors [73]. It is essential to take extra precautions regarding the usage of medications like ACE inhibitors and angiotensin receptor blockers in such patients for the management of hypertension, coronary artery disease, and congestive heart failure. Similarly, antiretroviral drugs like Lopinavir/Ritonavir may not be advisable for infected patients following the CABG procedure due to associated side effects such as prolonged PR and QT interval [74]. Patients with frequent QTc prolongation abnormalities should be assessed with electrocardiogram measures [73]. Elevated cardiac troponin levels found post-operatively as part of the follow-up strategy for CABG might also indicate a likely COVID-19 infection [74]. Rural populations, when compared with urban populations, have relatively greater risk factors for cardiovascular disease and COVID-19, including obesity, hypertension, and diabetes mellitus. Patients in rural hospitals are also more likely to exhibit poorer outcomes for cardiovascular disease [75]. This is more likely to be exacerbated by COVID-19. Telemedicine can help improve access to rural areas, especially during the pandemic.
Imaging procedures put the imaging staff at risk of transmission as well as contamination of equipment. Table 1 demonstrates some of the devices that can be used to help provide whole-body scans and allow cardiologists to monitor patients with heart failure, valvular heart diseases, and atrial or ventricular enlargement. Handheld ECGs that display heart electrical activity on portable devices can be shared between healthcare workers [76]. This can prove to be a fast means of communication between cardiologists and help accelerate the management and screening of such patients. Schedules can also be allocated such that cardiologic scanning can be done on infected patients only during specific timings so that they can be effectively disinfected after use.
Since most elective and non-urgent cardiology procedures have been postponed, the risk stratification protocol places cardiothoracic surgeries under “urgent-elective” which means that they must be performed in less than 2 weeks of patient presentation [54]. This can be incorporated to triage procedures and ensure delivery of the necessary cardiac care to the patients who need it. Negative pressure procedure rooms and proper disinfection of the equipment before and post-procedure is imperative. The operation theatre staff should be limited and communications with team members outside should be done with electronic devices or telephones [77]. All patients must be screened for COVID-19 before any interventional procedures. In case of a shortage of testing kits, a chest CT is also a reliable source to screen patients for any viral infection including COVID-19 [78]. Screening of patients and staff members of interventional cardiology departments including catheterization lab and ICU coupled with disinfection of all equipment can help ensure that these departments are strictly COVID-19 free. Within these wards, separate procedure rooms can be allotted to COVID-19 positive patients [79].
The triage system has been implemented in emergency departments to manage limited resources and massive patient influx. History, examination and measurement of oxygen saturation, and, initial workup of cardiac and inflammatory markers at the time of hospital admission can help determine the urgency of the hospital care needed [80]. Patients with stable angina or structural heart diseases with less severe symptoms can be treated remotely at their homes. Short term prognosis, age, and risk stratification scores can be effectively used to categorize patients according to the severity of their illness for emergency cardiac care, ICU admissions, cardiology imaging, interventional procedures, and life-saving protocols such as advanced life support which requires the use of many of hospital’s resources and puts staff at risk of contracting COVID-19. Table 2 shows specific ways in which a triage system can be implemented for various procedures.
| Patients with cardiovascular disease requiring cardiovascular interventions in the catheterizationlab [81] | |
| Patients requiring transcatheter aortic valve replacement [82] | |
| Note: It is reasonable to postpone TAVR in asymptomatic patients for 3 months or until resumption of elective procedures. However, possible monitoring via telehealth should be continued. | |
| Patients requiring percutaneous mitral valve repair [82] | Emergent: |
| Patients requiring valve-in valve transcatheter mitral valve replacement [82] | Emergent: |
| Patients requiring electrophysiological procedures*** [6] | Emergent: |
| Semi-urgent: | |
| Elective: | |
| Abbreviations: MI, myocardial infarction; LM disease, left main disease; AS, aortic stenosis; MR, mitral regurgitation; NYHA, New York Heart Association class; NSTE-ACS, non-ST-segment elevation myocardial infarction (NSTEMI)-acute coronary syndromes; HFrEF, heart failure reserved ejection fraction; CAD, coronary artery disease; CAG, coronary angiogram; EF, ejection fraction; CHF, congestive heart failure; TAVR, transcatheter aortic valve replacement; ICU, intensive care unit; VT, ventricular tachycardia; AF, atrial fibrillation; AFL, atrial flutter; AV, atrioventricular; WPW, Wolff-Parkinson-White; EOS, end of service; ERI, elective replacement indicator; ICD, implantable cardioverter defibrillator; CRT, cardiac resynchronization therapy; AV, atrioventricular; HF, heart failure; TEE, transesophageal echocardiography; LAA, left atrial appendage; CIED, cardiovascular implantable electronic device; EP, electrophysiology. ***These triage guidelines for EP procedures have been adopted from the previous American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association guideline (2020). | |
Patients with cardiac arrest should be moved to negative-pressure rooms quickly to avoid aerosol generation. A compressions-only CPR can be performed on the way to a negative pressure room. Table 1 further illustrates the ways of reducing aerosol transmission for chest compressions and the use of an oxygen mask. An oxygen mask with a flow of 10 L/min should be used to cover the mouth and nose of the patient and additional layers can be added using a towel or cloth [83].
According to a recent meta-analysis, there has been a reduction in heart failure patient admission and mortality for those monitored by telemedicine [84]. Table 1 shows how telemedicine can be tailored to the need of the cardiology department for the patients and for teaching purposes. Additionally, it also shows how monitoring devices can be utilized for patients with arrhythmias. The Brazilian society of cardiology has issued telemedicine guidelines for cardiology which can be followed for diagnosis, management, and treatment of cardiac patients and can also be used to impart preventive measures to patients with severe cardiac diseases [85]. Smart weighing devices can also be used to monitor the sudden increase in weight, especially in heart failure patients [86]. Patients with acute chest pain should be encouraged to not wait too long but instead called into STEMI networks for immediate care. At the same time, pre-hospital electrocardiogram and diagnosis can be made possible with telemedicine for faster diagnosis and prevention of symptoms deterioration [87]. There are conflicting results from studies assessing the effects of telemedicine on cardiac events such as cardiovascular death, mortality, hospitalization, and emergency admission rates [88]. However, the success of a tele-monitoring system requires adherence from patients and depends upon structural organization to manage large amounts of data. This can translate to having a culturally appropriate infrastructure and integration of technologies to manage the existing data, along with insurance coverage [89]. One proposed organizational model suggests remote monitoring with cardiac implantable electronic devices (CIED). This model is organized into five aspects, first involving cardiovascular technicians who should be updated on the CIED technology, a physician who should monitor the clinical devices and patients, an ambulatory team, a reporting system to the general practitioner and outpatient cardiologist, and lastly the patient [88]. Considering the potential for cardiac involvement in COVID-19 patients and the risk of poor outcomes in cardiac patients, remote monitoring and virtual visits should be encouraged. It can enable monitoring of heart rhythm and blood oxygen saturation, allowing for decisions to be made regarding hospitalization of quarantined cardiac patients in case of an emergency.
Lack of adequate equipment needed for thrombolysis, respiratory care, PCIs, and appropriate PPE needs to be managed by hospitals to ensure the flow of patient care. According to the Harvard Business review, hospitals need to manage supplies by predicting short term demands, managing shortages by identifying the root cause, enhancing coordination among hospitals, and countering staff shortages [90]. Risk stratification scores mentioned in Table 1 include thrombolysis in myocardial infarction (TIMI) score, global registry of acute coronary events (GRACE) score and the platelet glycoprotein IIb/IIIa in unstable angina: receptor suppression using integrilin therapy (PURSUIT) [21, 91]. Furthermore, the shortage of staff needs to be tackled. In the United Kingdom (UK), general nurses were trained for respiratory care under supervision. Healthcare workers with comorbidities should not be allowed to perform invasive procedures for cardiology patients. They also need to monitor themselves every 2 days for fever or respiratory symptoms. If symptoms occur, such workers need to be immediately removed and screening of the exposed staff should be done through RT-PCR [68].
Along with other drastic effects of the pandemic, it is impossible to not take short-term and long-term effects on cardiology services into consideration. Measures like reduction in cardiology procedures such as PCI, intubation, imaging, in-hospital staff, and increased time taken to complete cardiac procedures have gradually led to a reduction in clinical visits due to the long-term psychological impact and stigma associated with COVID-19 and the risk of contracting it. This will most likely lead to worsening of cardiac symptoms in COVID-19 recovered and non-COVID-19 affected patients. Such far-reaching effects may not only burden but collapse cardiac departments during the pandemic and post-pandemic era. Incorporating smart use of telemedicine, monitoring devices, triage, and risk scoring protocols, and ensuring bulk hospital supplies of safety equipment and machines are the urgent need of the time, which if not done, can lead to a steady rise in cardiac diseases related deaths.
FY: conception of the study, major drafting of the work, final approval and agreeing to the accuracy of the work. SMS: conception of the study, major drafting of the work, final approval and agreeing to the accuracy of the work. AN: conception of the study, major drafting of the work, final approval and agreeing to the accuracy of the work. AJ: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. SMIS: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. RKO: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. OM: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. AAK: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. SJ: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. AAR: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. SS: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. SAKK: help in design of the study, drafting of the work, final approval and agreeing to the accuracy of the work. AM: supervision, critical revision of the manuscript, final approval and agreeing to the accuracy of the work. HML: supervision, critical revision of the manuscript, final approval and agreeing to the accuracy of the work.
None to declare.
This research received no external funding.
The authors declare no conflict of interest.
