†These authors contributed equally.
Academic Editor: Peter A. McCullough
Both Transthoracic echocardiography (TTE) and cardiac magnetic resonance (CMR)
have well-established role in mitral regurgitation (MR) quantification for
optimal management strategy. We assessed the correlation between TTE and CMR in
the quantification of MR. Participants with isolated MR and echocardiographic
mitral regurgitant volume (RVol)
Mitral regurgitation (MR) is a major cause of morbidity and mortality affecting 38,270 persons per 1 million US adult population [1]. Subgroup analysis of the European registry of MR (EuMiClip) data showed a 5.2% prevalence of significant MR and 70% of patients with severe primary MR had a class I indication for surgery [2]. Transthoracic echocardiography (TTE) is the standard approach for the assessment of MR. Despite its numerous technical and non-technical limitations, TTE has been recommended by the American Society of Echocardiography for the quantification of MR [3]. Cardiac magnetic resonance (CMR) is a favored diagnostic imaging technique for valvular heart disease due to its numerous features as non-ionizing radiation, excellent imaging quality, unlimited scan widows with high accuracy and reproducibility, and tissue diagnosis [4]. We wanted to evaluate the correlation between TTE and CMR in the quantification of MR and explore their complementary use for enhancing diagnostic accuracy and improving patient outcomes.
Our study was a 1-year cross-sectional, open-labeled, non-randomized, single cohort study conducted at a single cardiac center in a tertiary care hospital. Investigators weren’t blinded to the study group. The study design was approved by the hospital ethics committee review board, all participants signed written informed consents, study procedures were carried out following the Code of Ethics of the World Medical Association (Declaration of Helsinki), all information/images were anonymized, and the privacy rights of the study participants were observed diligently.
Study participants were patients referred to the cardiology department. They were subjected to history taking and data collection for age, gender, risk factors especially hypertension, diabetes mellitus (DM), chronic kidney disease, coronary artery disease, smoking and hyperlipidemia, nature and course of ischemic, pulmonary congestion and low cardiac output symptoms, and comprehensive clinical examination.
Thirty eligible participants were enrolled, consecutively assigned and allocated
in a single cohort, and underwent TTE using Phillips EPIQ 7 ultrasound system for
cardiology equipped with xMATRIX transducer (X5-1). Data documented with TTE
included jet dimensions, vena contracta, mitral regurgitant volume (RVol)
quantification by proximal isovelocity surface area (Echo_RVol), effective
regurgitant orifice area, mitral regurgitant fraction (RF) determined by the
quantitative Doppler method (Echo_RF), early diastolic mitral E wave velocity (E
wave), left atrial (LA) volume, and left ventricular (LV) volume and function by
the modified Simpson’s biplane method. MR was categorized based on Echo_RVol and
Echo_RF into mild (
| Mild | Moderate | Moderate-Severe | Severe | |
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | |
| Qualitative | ||||
| Colour Doppler jet area | Small, central jet ( |
Signs of MR greater than mild present, but no criteria for severe MR. | large jet (area | |
| Doppler vena contracta width (mm) | 30-49 | 50-69 | ||
| Quantitative | ||||
| Regurgitant volume (mL) | 30-44 | 45-59 | ||
| Regurgitant Fraction (%) | 30-39 | 40-49 | ||
| Regurgitant orifice area (cm |
0.20-0.29 | 0.30-0.39 | ||
| Additional essential criteria | ||||
| LA size | Enlarged | |||
| LV size | Enlarged | |||
| LA, left atrium; MR, mitral regurgitation. | ||||
The enrolled study participants underwent cardiac magnetic resonance (CMR)
within one week for quantification of MR using Siemens Magnetom Aera 1.5T
magnetic resonance imaging scanner. Data documented with CMR include indirect
quantification of mitral RVol by measuring the difference between left and right
ventricle stroke volumes (CMR_RVol
| Direct estimation of flow and volume by VENC * |
| MR = LVSV- RVSV* |
| MR = LVSV-AVSV |
| MR = LASV-AVSV |
| * The methods used in our study. AVSV, aortic valve stroke volume; LASV, left atrium stroke volume; LVSV, Left ventricle stroke volume; MR, mitral regurgitation; RVSV, Right ventricle stroke volume; VENC, velocity encoding. |
 Fig. 1.
Fig. 1.Echo and CMR images of patient with severe eccentric MR.
Showing severe primary MR with eccentric jet by echo (Rvol 62 mL, EROA 0.48
cm
The study evaluated the correlation between Echo_Rvol and CMR_RVol
The echocardiographic and CMR assessment outcomes were coded, and the data was
analyzed with the Statistical Package for the Social Sciences software for MAC
(SPSS®) version 26. Quantitative (continuous) data was expressed
as means and standard deviations, while qualitative (categorial) data was
expressed as medians and ranges. Parametrically distributed quantitative
variables were compared with the Independent two-tailed t-test and
correlated with Pearson’s Correlation Coefficient, respectively. Pearson’s
Correlation Coefficient (r) value was interpreted as follows: 1 means perfect
correlation, 0.75-1.0 is strong correlation, 0.50-0.75 is moderate correlation,
0.25-0.5 is weak correlation, and
We recruited 30 patients from one hospital in one country from January 2019
through December 2019. The study group was balanced with regards to baseline
characteristics and risk factors. The key sociodemographic feature of enrolled
participants was equal gender representation (Mean age 52.7
| Age (Years) | 52.7 | 19.3 |
| Male | 15 | 50.0% |
| Diabetes Mellitus | 10 | 33.3% |
| Hypertension | 14 | 46.6% |
| Hyperlipidemia | 14 | 46.6% |
| Chronic Kidney Disease | 10 | 33.3% |
| Coronary Artery Disease | 12 | 40.0% |
| Smoker | 6 | 20.0% |
| Chest pain | 6 | 20.0% |
| Shortness of Breath | 16 | 53.3% |
| Palpitations | 5 | 16.6% |
| Echocardiography | ||
| Mild | - | - |
| Moderate | 17 | 56.6% |
| Mod-Sev | 8 | 26.6% |
| Severe | 5 | 16.6% |
| Cardiac Magnetic Resonance | ||
| Mild | 5 | 16.6% |
| Moderate | 12 | 40.0% |
| Moderate-Severe | 10 | 33.3% |
| Severe | 3 | 10.0% |
| Mitral Regurgitation type | ||
| Primary | 12 | 40.0% |
| Secondary | 18 | 60.0% |
| Jet direction | ||
| Central | 20 | 66.7% |
| Eccentric | 10 | 33.3% |
| Ejection fraction | ||
| 20 | 66.7% | |
| 10 | 33.3% | |
| Values are mean | ||
The mean left ventricle end-diastolic volume (LVEDVi) was 80.2
| Echo | CMR | ICC | P-value | ||||
| Mean | SD | Mean | SD | ||||
| EDVI | 80.2 | 33.5 | EDVI_ CMR | 103.1 | 29.3 | 0.839 | |
| ESVI | 44.6 | 30.5 | ESVI_ CMR | 60.8 | 33.4 | 0.888 | |
| SVI | 34.3 | 15.8 | SVI_ CMR | 42 | 16.7 | 0.786 | |
| EF | 47 | 19.2 | EF%_ CMR | 44.7 | 19.7 | 0.956 | |
| LAVI | 45.8 | 16.1 | LAVI_ CMR | 46.8 | 18.1 | 0.751 | |
| *Significant. EDVI, left ventricle end-diastolic volume, index; EF, LV ejection fraction; ESVI, left ventricle end-systolic volume index; LAVI, left atrium volume index; SVI, left ventricle stroke volume index. | |||||||
The mean mitral RVol was 45.0
| Intraclass Correlation |
95% Confidence Interval | F Test with True Value 0 | |||||
| Lower Bound | Upper Bound | Value | df1 | df2 | Sig | ||
| Single Measures | .752 |
.554 | .873 | 7.253 | 29 | 29 | .000 |
| Average Measures | .859 | .706 | .932 | 7.253 | 29 | 29 | .000 |
| Two-way random effects model where both people effects and measures effects are
random.
a. The estimator is the same, whether the interaction effect is present or not. b. Type A intraclass correlation coefficients using an absolute agreement definition. | |||||||
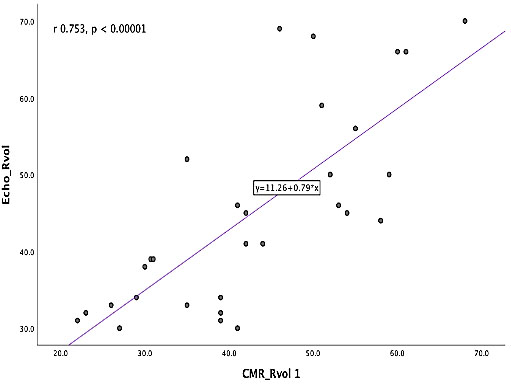 Fig. 2.
Fig. 2.The correlation between Rvol by echo vs CMR by indirect quantification. Simple Scatter plot with fit line demonstrating statistically significant strong positive correlation between echo mitral regurgitant volume (Echo_RVol) and CMR mitral regurgitant volume by indirect quantification (CMR_RVol
 Fig. 3.
Fig. 3.The correlation between Rvol by Echo vs CMR by direct quantification (velocity mapping). Simple scatter plot with fit line demonstrating positive moderate
correlation between Echo-RVol and CMR-RVol by velocity mapping (CMR_RVol
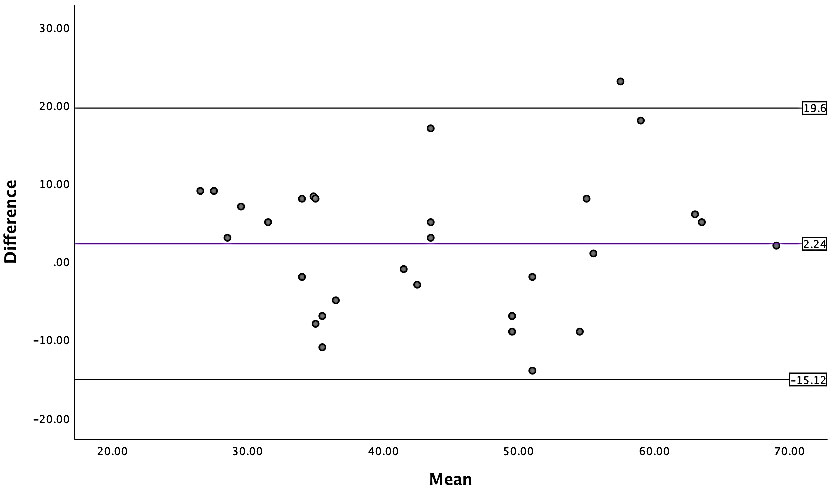 Fig. 4.
Fig. 4.Bland-Altman plot showing bias of 2.24 units between the means
of RVol by Echo vs CMR by indirect quantification within 95% limits of
agreement. Bland-Altman Plot demonstrating bias of 2.24 units between the means
of Echo-RVol vs CMR_RVol
The inter-observer reliability of the MR grade between TTE and CMR was seen in
20 (66.4%) patients showing statistically significant moderate agreement
(
| CMR | Total | |||||
| 1 | 2 | 3 | 4 | |||
| Echo | 2 | 5 | 10 | 1 | 0 | 16 |
| 3 | 0 | 2 | 7 | 0 | 9 | |
| 4 | 0 | 0 | 2 | 3 | 5 | |
| Total | 5 | 12 | 10 | 3 | 30 | |
| Showing the comparison between Echo and CMR when only Regurgitant Volume by Echo (Echo-RVol) was used for the MR category (grade), the overall agreement improved to 20 (66.67%) patients. Yellow color indicates agreement. | ||||||
| CMR | Total | |||||
| 1 | 2 | 3 | 4 | |||
| Echo | 2 | 5 | 8 | 4 | 0 | 17 |
| 3 | 0 | 4 | 4 | 0 | 8 | |
| 4 | 0 | 0 | 2 | 3 | 5 | |
| Total | 5 | 12 | 10 | 3 | 30 | |
| Showing the comparison between Echo and CMR when the Regurgitant fraction (Echo-RF) integrated based approach was used for the MR category (grade) by Echo. The overall agreement was seen in 15 (50%) patients. Yellow color indicates agreement. | ||||||
 Fig. 5.
Fig. 5.Bar chart showing the patients with the same versus different MR category between echo versus CMR based on Rvol. 1. Blue; Patients with mild MR, 2. Red; Moderate MR, 3. Green; Moderate to severe MR and 4. Orange; Severe MR.
 Fig. 6.
Fig. 6.Bar chart showing the patients with the same versus different MR category between echo versus CMR based on RF. 1.Blue; Patients with mild MR, 2. Red; Moderate MR, 3. Green; Moderate to severe MR and 4. Orange; Severe MR.
Mitral regurgitation (MR) is a major cause of morbidity and mortality worldwide.
Transthoracic echocardiography (TTE) is the standard approach for assessment of
MR. Cardiac Magnetic Resonance (CMR) is a favored diagnostic imaging technique
for valvular heart disease. We hypothesized that integration of TTE and CMR will
enhance the diagnostic accuracy of MR and improve patient outcomes. We wanted to
evaluate the correlation between TTE and CMR in the quantification of MR. Our
1-year cross-sectional, open-labeled, non-randomized, single cohort study
revealed a statistically significant good reliability between Echo_RVol and
CMR_RVol
Our study didn’t have missing data allowing robust per-protocol analysis, the investigators who analyzed and reported the CMR assessment outcomes were blinded to the participants’ clinical data and TTE results, and a second investigator blinded to the CMR measurements reported by the first investigator repeated them at a different time interval to evaluate the inter-observer reproducibility. On the other hand, the study has important limitations. It was a single centered study with small sample size. Being a cross-sectional study with a lack of lengthy follow up didn’t allow us to investigate the chronological relationship between the TTE results, the CMR measurements, and the clinically driven outcomes.
In our study, the positive correlation between the TTE and the CMR in quantification of mitral RVol highlights the potential role of CMR as a complementary imaging tool to TTE, especially in limited or inconclusive TTE studies. The RF by CMR is more accessible and reproducible, unlike the challenging Echo_RF. This unique feature of CMR leads to better grading and classification of MR which enhances MR management strategy and may improve patients’ cardiovascular outcomes. Large prospective studies are warranted to improve the sensitivity and accuracy of the phase-contrast velocity mapping and compare CMR vs TTE regarding the measurement of cardiovascular clinical outcomes in patients with valvular heart disease, especially in asymptomatic MR patients who do not have Class I indications for surgery.
bSSFP, balanced steady state free precession; CMR, cardiac magnetic resonance; CW, continuous wave doppler; Echo, echocardiography; EROA, effective regurgitant orifice area; ICC, intraclass correlation coefficient; LAEDV, left atrium end diastolic volume; LAESV, left atrium end systolic volume; LAVi, left atrium volume index; LV, left ventricle; LVEDi, left ventricle end diastolic volume index; LVEF, left ventricle ejection fraction; LVESi, left ventricle end systolic volume index; LVSV, left ventricular stroke volume; MR, mitral regurgitation; MV, mitral valve; PISA, proximal isovelocity surface area; PW, pulsed wave doppler; RF, radio frequency; RF, regurgitant fraction; RV, right ventricle; Rvol, regurgitant volume; SAX, short axis stack; SD, standard deviation; TE, echo time; TR, repetition time; VC, vena contracta; VENC, velocity encoding; VTI, velocity time integral.
WT did the patients recruitment, reviwed, analysed, interpreted the patient data and writing the manuscript. KA reviewed and approved the study proctol, TM helped in writing and reviewing the manuscript. HE has a major contributor in writing and reviewing the manuscript. All authors read and approved the final manuscript.
Approved by Research and Ethical committee.
The authors would like to express their gratitude to AL Badarin, F for editing the manuscript and Rivard, A for conducting and interpreting some of the CMR imaging studies.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare no conflict of interest.
